 |  |
Specialty lenses give many patients a clear and functional window to the world. At times, fitting these lenses is straightforward and follows a predictable process. At other times, we need to be more creative to make sure these lens fits are ideal for patients. This column discusses four strategies to improve specialty lens success.
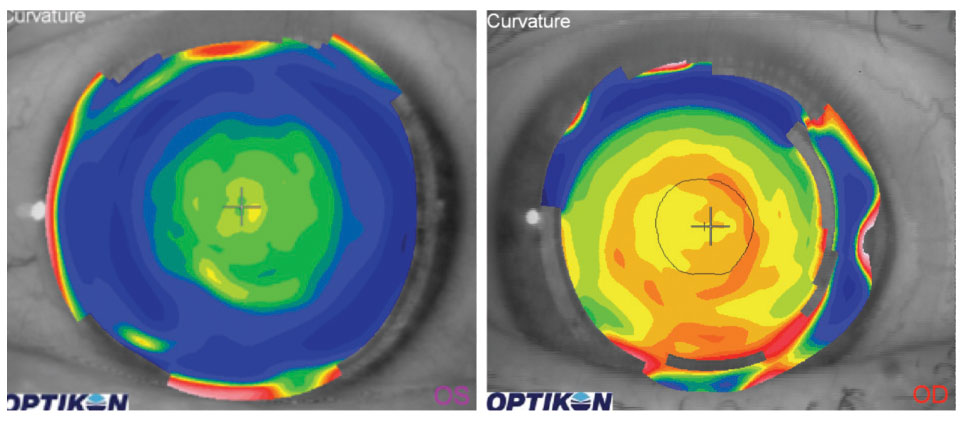 |
| Figs. 1a and 1b. The topography of a near-center multifocal lens (left) shows a steeper region centrally that corresponds to near optics. The topography of a distance-center multifocal lens (right) shows a flatter region centrally that corresponds to distance optics. |
Taking Topography
Multifocal lenses provide patients an opportunity to see at distance and at near with minimal to no need for supplementary glasses. Unfortunately, some patients have a difficult time with them. Soft multifocals are based on the premise that we look through the center of the lens and the distance and near optics focus on the retina. Neuroadaptation allows patients to adjust to distance and near vision when these lenses are fit and worn successfully.
The optical centers of multifocal lenses don’t always line up with a patient’s line of sight. Most patients look through a point that is nasal to the geometric center of the pupil. Many of the optical properties of soft multifocals are located on the anterior surface of the lens. If a topography measurement is taken over the surface of a multifocal lens, because of the differences in optical properties, steeper zones associated with more plus power will be evident. For example, when a topography measurement is taken over the surface of a near-center lens, it will be steeper centrally (Figure 1a). If a patient is wearing a distance-center, near periphery lens, there will be steeper regions in the peripheral portion of the lens and flatter zones in the central portion (Figure 1b).
Most topographers can identify a patient’s line of sight to help you see where it is with respect to the optical center of the lens on the eye. In our experience, the closer a patient’s line of sight is to the optical center of the lens, the higher the likelihood of success with the multifocal lens design. A patient is usually less successful when their line of sight diverges from the optical center of the lens (Figure 2). Specialty lens designs in soft and scleral lenses can now alter the position of the optics in the center of the lens to more appropriately align with a patient’s line of sight.
Topography can be taken over the surface of most lenses, including gas permeable (GP) multifocals. These lenses are typically designed with their distance optics in the center of the lens and their near optics located more peripherally. Topography taken over the GP lens demonstrates a flatter profile centrally and a steeper profile peripherally. When the lens and line of sight are aligned appropriately, patients tend to do very well. If the lens is decentered from a patient’s line of sight, however, it can alter the optical zones and degrade the patient’s visual quality at distance and at near (Figure 3).
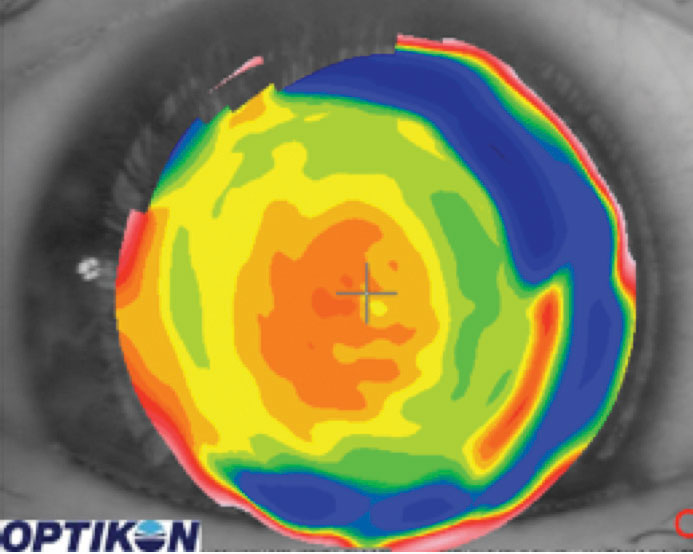 |
| Fig. 2. The near zone of this lens is decentered inferior temporally. |
Conquering Comfort
There are certain cases in which patients may be able to see remarkably well out of their specialty lenses but experience poor comfort that precludes them from being able to wear them. Several strategies—including modifying lenses, switching solutions and prescribing drops—may improve comfort. If patients have comfort issues but do not have dry eye, they may benefit from a Lacrisert placed in the lower fornix.
A Lacrisert is a prescription ophthalmic insert comprised of hydroxypropyl cellulose. After the insert is placed, it slowly dissolves over 24 hours, releasing demulcents into the tear film and providing more comfort.1 Teach users to place the insert in the lower fornix only after they have placed the lens on their eye so it does not fall out.
An additional option for increasing comfort is a coating called Hydra-PEG (Tangible Science) that adds hydrophilicity to provide a more moisture-rich surface that resists lipid deposition.2 This coating is applied to the lens surface at the time it is manufactured. Lenses with this coating cannot be rinsed with water and should not be stored dry.
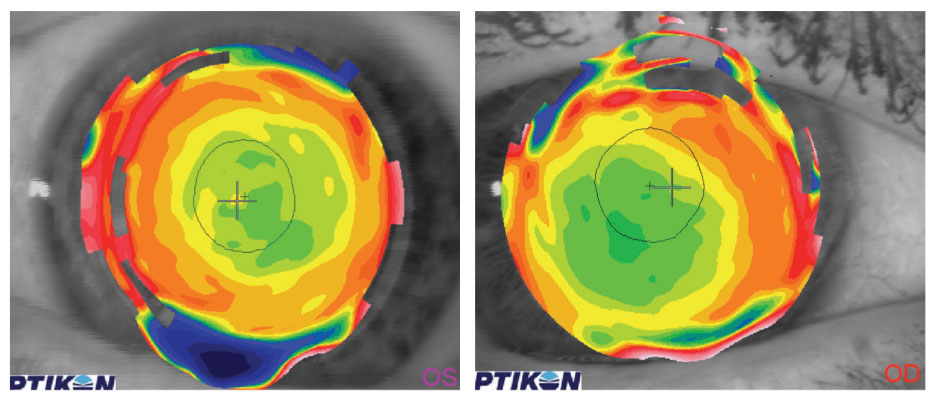 |
| Fig. 3. At left is the topography over a well-centered GP multifocal. At right is the topography over a GP multifocal lens that is decentered inferior temporally. |
Ordering Ortho-K
Ortho-K helps manage and correct myopia. Strategies for fitting the lens appropriately include optimizing the lens fit, dispensing the right lens and following up with topographies and refractions after the patient has worn the lens overnight.
New technologies provide us with greater insights to help guide our ortho-K fits. AS-OCT gives us the ability to measure epithelial thickness before and after treatment, which shows us the effects of ortho-K on the cornea. Visualizing the area of thinned epithelium helps guide lens positioning on the cornea and treatment zone placement (Figure 4).
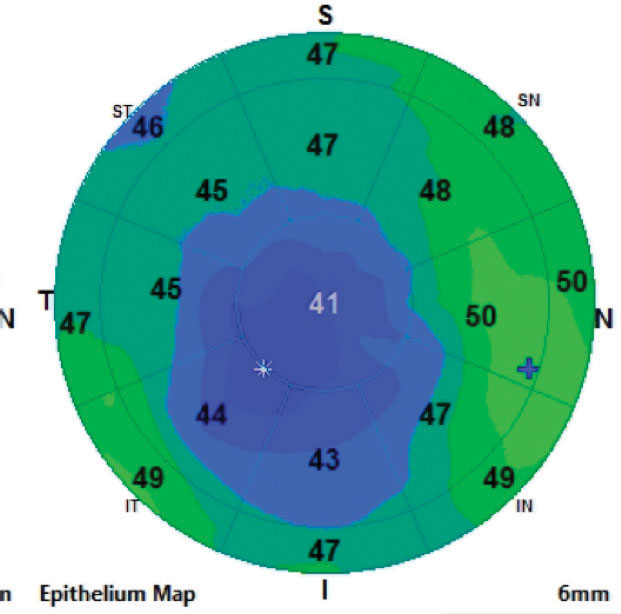 |
| Fig. 4. This epithelial thickness map taken after ortho-k shows an inferior temporally displaced treatment zone. |
Pinpointing Pupils
There are times when pupil dilation degrades the quality of vision that some patients experience with specialty lenses. GP multifocals are designed so that the distance optics are centrally located and the near optics are in the periphery. When the pupil dilates, it may encroach into the near optics, reducing the quality of distance vision. Patients undergoing ortho-K can have issues with night vision if the pupil enlarges into the reverse curve created in the cornea. Patients wearing small diameter lenses, specifically those fit for an inferiorly decentered cone in cases of keratoconus, may notice reduced vision if their pupils dilate in low light levels past the optical zone of the lens or, in extreme cases, the outer edge of the lens.
Fortunately, there is a pharmacological way to prevent a patient’s eyes from dilating. Alpha-2 receptors are located on the presynaptic nerve endings that innervate the dilator muscle. They bind excessive quantities of norepinephrine in the synaptic cleft to down-regulate the release of further norepinephrine. Brimonidine, an alpha-2 adrenergic agonist, binds directly to alpha-2 receptors to prevent pupil dilation by preventing norepinephrine release into the synaptic cleft.3
Brimonidine is available in these concentrations: 0.2%, 0.15%, 0.1% and 0.025%. We typically recommend patients use the drops 30 minutes prior to performing critical viewing tasks in low light levels, such as driving at night. We reserve this strategy for patients whose vision cannot be improved with refractive correction or lens alteration.
There are a handful of strategies that can help our specialty lens users successfully wear their lenses. Any one technique, however, doesn’t always work for all patients. Knowing alternative options gives you the best chance at achieving a good, comfortable fit for the best results in these patients.
| 1. Bausch + Lomb. Lacrisert. www.bausch.com/ecp/our-products/rx-pharmaceuticals/rx-pharmaceuticals/lacrisert. Accessed March 29, 2019. 2. Tangible Science. tangiblescience.com/professionals/. Accessed March 29, 2019. 3. Kato COS, Shimizu K, Kamiya K, et al. Effects of brimonidine tartrate 0.1% ophthalmic solution on the pupil, refraction and light reflex. Sci Rep. 2018;8:9003. |


