  |
A 31-year-old male presented to the clinic with a history of keratoconus, treated with corneal crosslinking (CXL) several years ago. The patient also had a history of corneal gas permeable (GP) lens intolerance and was fit with scleral lenses, which were difficult for him to apply and remove, leading to discontinuation. The persistent irritation with rigid lenses and difficulty with handling raised interest in an easier, more comfortable alternative.
On initial presentation, best-corrected visual acuity (BCVA) with manifest refraction was 20/25- OD and 20/30 OS. Scheimpflug tomography showed a point of maximum keratometry of 50.1D OD and 50.4D OS and an IS ratio of 9.5D OD and 8.7D OS.
Considerations
Here, we highlight how each of us would proceed in this case.
Dr. Su. Traditionally, corneal GP lenses have been the first-choice option in patients with irregular corneas, especially keratoconus. The varying severity of elevation and asymmetry can make GP fitting a challenge. These patients may experience poor comfort due to edge lift, apical bearing and poor stability, which can impact corneal health and result in complications with long-lasting effects such as corneal scarring. Additionally, lens decentration and small optic zones can lead to suboptimal vision. In these cases, scleral lenses can certainly help as they provide the visual benefits of a GP lens but with a larger optic zone and increased stability without touching the corneal surface, providing comfort and vision improvement.
That said, scleral lenses can be challenging for some patients due to the application and removal process. It is unsurprising that handling issues, such as in this patient, are among the main reasons for scleral lens dropout.
In this case, it is fair to start with a soft lens and assess the patient’s visual potential. A custom soft lens is ideal for this patient as it has vast parameter customizations compared with the ready-made traditional soft contact lenses that typically fit the average “normal” corneal shape and depth. Changing the thickness of a custom soft contact lens also allows us to somewhat mask the elevations and asymmetry in an irregular cornea. Thus, a custom soft lens may provide adequate visual stability, comfort and centration. Other options to consider are a piggyback system using a soft lens to cushion the GP or hybrid lenses to maintain the optics of a GP lens while also increasing lens stability and comfort.
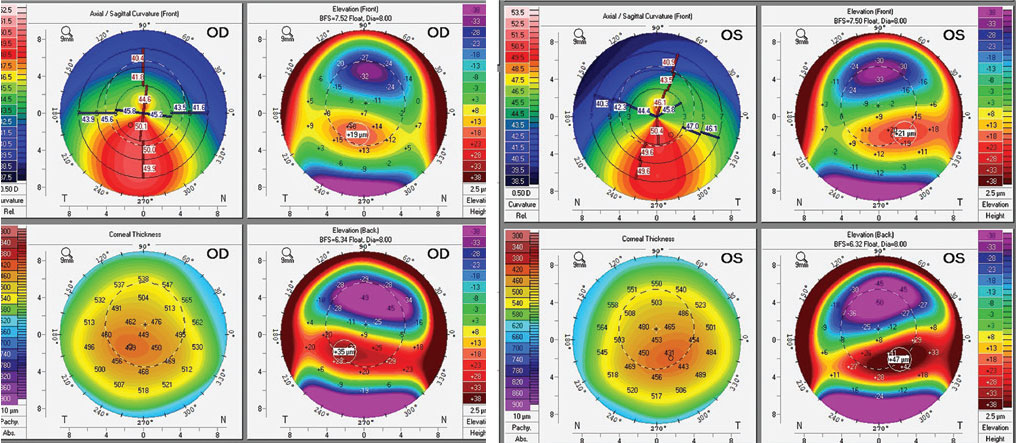 |
| Corneal tomography of the patient’s right and left eye. Click image to enlarge. |
Dr. Gelles. In our clinic, we have found that keratoconus patients with low amounts of asymmetry, decently correctable with manifest refraction, are generally successful in custom soft lenses. Another option to consider is a hybrid lens; this could prove to be an excellent alternative for the patient before revisiting a corneal GP with a piggyback or scleral lens. I am always hesitant to repeat modalities the patient has tried in the past unless it is truly the best or only option.
Custom soft lenses for irregular corneas work by increasing the lens center thickness to reduce lens drape and mask mild irregular astigmatism. However, this modality is significantly compromised when it comes to Dk/t, with center thicknesses ranging from 0.2mm to 0.6mm and a lens made of a low Dk—typically 15 to 30—hydrogel material or a 60Dk silicone hydrogel material, creating a very low Dk/t. Following these patients on a six-month interval is prudent to monitor corneal health. Additional considerations for patients like this who have failed other contact lens options include surgical interventions.
A collaborative and comprehensive approach to keratoconus management has patients undergo CXL to prevent disease progression, specialty contact lens fitting to provide the best visual acuity and optional corneal contouring procedures to improve spectacle and uncorrected visual acuity. This combination of procedures and lenses differs for each patient based on their physiology and needs.
CXL has opened more surgical options, particularly excimer laser-based procedures that have previously not been used due to the possibility of further biomechanically destabilizing the keratoconic cornea. Prior to CXL, the surgical options for a patient with contact lens intolerance were intracorneal ring segments or a corneal transplant, whether deep anterior lamellar or penetrating. Photorefractive keratectomy (PRK) procedures have become viable options when performed with CXL to increase biomechanical strength. These procedures can be performed sequentially or in combination.
The goal of PRK procedures for keratoconus is not a full refractive correction but rather a targeted, tissue-sparing, topography-guided ablation to improve corneal symmetry and contour. Several studies have shown improvements in BCVA without disease progression, and in our clinic, we have seen this improved contour lead to improved outcomes with spectacles and less complex contact lens options. In this case, the patient has adequate corneal thickness and has had CXL. Should lens options be exhausted, the patient may be a good candidate for PRK. PRK in cases of keratoconus shouldn’t be performed until ocular maturity is reached, and any patient undergoing this combination of procedures needs continued follow-up to monitor for progression.
Dr. Noyes. It can be easy to see patients like this and feel the urge to jump straight to GP or scleral lenses; however, we must remember that we are treating the patient’s eye (as opposed to simply acting as “GP lens designers”), and we must do what is best for the eye/patient.
In milder cases of keratoconus, soft lenses are often an option, and custom soft lenses are able to provide many parameters to aid in fitting these eyes. In this case, custom soft lenses make a great starting point. When I come across this scenario in the clinic, I start with a soft lens and only make the jump to hybrid, GP or scleral if the patient does not have comfortable vision. Remember: if the patient’s keratoconus progresses, you may still be fitting a specialty lens in the future.
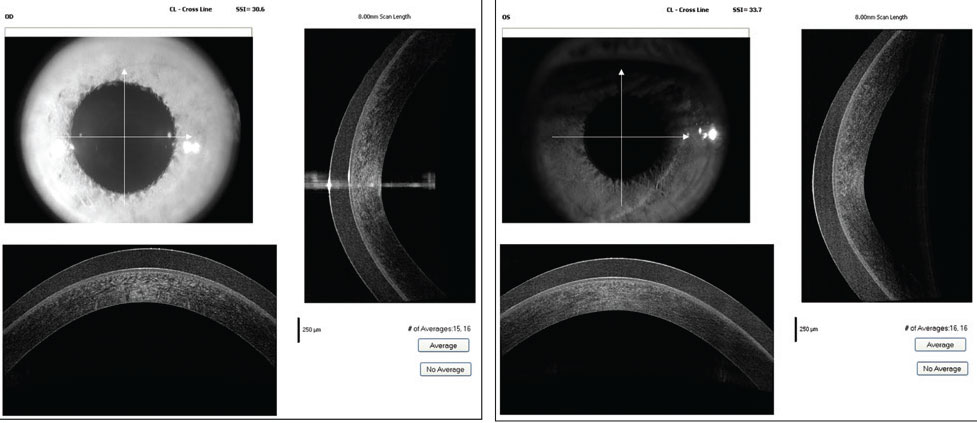 |
| OCT cross-section of the patient’s right and left cornea while wearing the custom soft lenses. Click image to enlarge. |
Discussion
Custom soft contact lenses are a good option for those with mild to moderate cases of keratoconus, especially with a history of GP or scleral lens intolerance. To address the irregular corneal shape, the central thickness of the soft custom lens is increased beyond the center thickness of a standard soft lens in an attempt to replicate the masking nature of a GP lens.
When the initial diagnostic custom soft contact lens is applied and allowed to settle, the physical fit is assessed, as is the visual potential through a spherocylindrical over-refraction.
Sometimes, patients may experience poor visual quality despite improved visual acuity and optimal lens fit due to lens drape and resultant higher-order aberrations. In these cases, lens center thickness can be increased to aid in a masking effect for these higher-order aberrations. Additionally, some visual symptoms can be addressed by changing the diameter of the optic zone of the lens.
As for the fitting relationship, these lenses can offer a variety of parameters for customization, the availability of which depends on the selected design. Some designs have multiple curves—a base curve to fit the cornea and a peripheral curve to control the movement and centration—and customizable diameters. For patients with mild to moderate keratoconus or a history of GP lens intolerance or scleral lenses dropout, custom soft contact lenses may allow for improved comfort, ease of handling and adequate visual correction.
Results
The patient was fit with a 0.3mm central thickness custom soft lens for irregular corneas. He returned for application removal training, which was a success. The lenses were rotationally stable with adequate movement. He ultimately achieved 20/25+ vision OD and OS and was happy to have improved vision, comfort and ease of handling.
Dr. Su is the Cornea and Contact Lens Fellow at the Cornea and Laser Eye Institute (CLEI) Center for Keratoconus. She has no financial interests to disclose.


