 |  |
Scleral gas permeable contact lenses have seen a surge in popularity over the past decade, but they have been evolving since the late 19th century. Practitioners, past and present, learn the options at their disposal and make the best choices for their patient’s benefit. Follow in their footsteps and be cognizant of the various factors that make up today’s GP lens materials.
Glass remained the primary material used to design contact lenses from 1887 until 1936, when William Feinbloom manufactured a scleral lens that combined glass and plastic to make the lens thinner and easier to wear.1
In 1948, Kevin Tuohy’s patent for what would become the first corneal contact lens described a lens made from polymethyl methacrylate (PMMA).1 The lens design had blunt edges and fitted flatter than current methods but rested entirely on the corneal surface. PMMA remained the primary rigid lens material until the introduction of the more oxygen permeable silicone-based lens in 1979.1
Modern Materials
To improve the nonexistent oxygen permeability (Dk) of PMMA lenses, silicone side branches were added to the methacrylate monomer, increasing the space between the polymer chain and allowing for an increased flow of oxygen.1,2 While lenses made from this silicone/acrylate (S/A) copolymer have a higher Dk, silicone is inherently hydrophobic, which may result in poor wettability and a surface prone for deposition. Wetting agents and crosslinking agents can also be added to the polymer to attract water molecules and increase the rigidity, respectively.1
The next generation of GP lenses added fluorine, which, in addition to being more resistant to deposition, also aids in oxygen transmission.1 Fluoro-silicone/acrylate (F-S/A) materials have less silicone, allowing increased stability of the lens while still retaining a high level of oxygen permeability. Their specific characteristics vary, but the vast majority of GP materials being used today are F-S/A polymers.
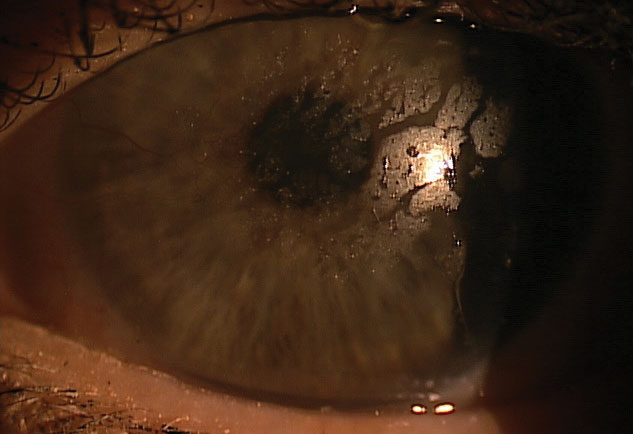 |
| Patients with ocular surface disease or an unstable tear film may suffer from poor surface wettability. |
Material Properties
Designing GP lenses is a fully customizable process. Base curve, diameter and power are paramount to an order, and material choice can easily become an afterthought. To choose a material, a basic familiarity with material properties is essential.
Oxygen permeability. When classifying GP lenses based on Dk, they can be split into three categories: low Dk (25 to 50), high Dk (51 to 99) and hyper Dk (≥100).1
However, the amount of oxygen transmission through an individual lens is also dependent on the thickness of each lens (Dk/t). If lenses are made with identical materials and Dk values, the Dk/t will decrease with increasing center thickness.
Surface wettability. This refers to how well the tear film spreads across the contact lens surface. Disruption or evaporation of the tear film from the anterior surface can increase deposition and may affect both the quality of vision and comfort of the lens.
Similar to the effect of a reduced tear break-up time, a GP lens that does not have an even tear layer will cause fluctuating vision that is often described as foggy or smeared. In vitro, wettability is measured by the wetting or contact angle. For GP lenses, the wetting angle is measured by captive bubble technique.
When a GP lens is submerged in water, the wetting angle is formed between the surface of the lens and an air bubble placed on the surface by a syringe. A wetting angle of zero would be a completely wettable surface, so lower wetting angles are desirable.3 Nevertheless, wetting angles and clinical performance don’t always correlate, since tear film chemistry can affect lens wettability.
Even with lower wetting angles, patients with ocular surface disease or an unstable tear film may still suffer from poor wettability. These patients may benefit from the addition of Hydra-PEG (Tangible Science) coating.
Specific gravity and refractive index. Specific gravity (SG) is the ratio of the density of a solid, in this case the GP lens, to the density of equal volume of water (SG=1.00) at the same temperature. Materials with a higher SG will therefore have a greater mass. Changing the SG can affect the lens mass by up to 20%.4
Similar to spectacle lenses, a GP lens with a higher refractive index (RI) will be thinner, which can reduce lens mass. A higher RI can also produce a higher add power on a front surface aspheric multifocal.5
Hardness and modulus. The hardness of plastics, including GP lenses, can be measured using the Rockwell R or Shore durometer methods. The two tests measure the resistance to indentation from various weighted loads. Although neither test can predict strength or scratch resistance, they can suggest a higher degree of durability. Shore hardness can also serve as a general indicator for modulus.6 Modulus describes the flexibility of a material, with a higher modulus resulting in a stiffer lens. Lower modulus lenses may cause flexure, especially on an astigmatic cornea.
Choosing a Material
While there is no algorithm for choosing a material, the approach will typically differ between scleral lenses and corneal GPs. For scleral lenses, oxygen permeability and surface wettability are arguably the most important considerations for choosing a material. Maintaining corneal health should be at the forefront of every scleral fit, especially with diseased and compromised corneas. The larger diameter lens will vault over the cornea, and the stagnant fluid reservoir will slow the diffusion of oxygen, depending on the varying amount of clearance beneath the lens.
Hyper-Dk materials are chosen as a default, but certain ocular conditions where hypoxia is of greatest concern, such as post-penetrating keratoplasty or limbal stem cell deficiency, will require the highest oxygen permeability available. Higher-Dk lenses tend to have less silicone, therefore tend to have a lower modulus and lower durability. Depending on the thickness of the lens and the haptic system, these lenses may be more prone for flexure or torsion.
Advise patients with scleral lenses on the proper care regimen to avoid scratching the lens surface or warping the lens. The greater surface area of scleral lenses also increases the importance of surface wettability.
With corneal GPs, pay attention to the patient’s ocular anatomy, tear film, refractive error and visual demands. Lens centration, comfort and optics tend to be more important factors leading to a successful outcome. Tear exchange will often mitigate the need for a hyper-Dk material, but Dk must be considered when dealing with high refractive errors. High myopic powers will have a thinner center thickness, so a lower Dk lens may provide a more stable fit. Conversely, high hyperopic lenses will be thicker, making a higher Dk more appropriate to increase Dk/t.
Lens thickness may also affect lens mass, which can be increased or decreased by changing SG and RI. To improve centration, a high-riding, lid-attached fit may need a larger, heavier lens, while a low-riding or interpalpebral fit may need a lens with less mass. Despite the smaller surface area, if patients have a poor tear film or have trouble with their cosmetics, wettability and deposition can be an equal nemesis to corneal GPs.
If plasma treatments or Hydra-PEG are considered, keep in mind that not all cleaning and care regimens are compatible with these. If patients are set in their ways with an abrasive cleaning regimen or tap water rinse, choosing a material with lower silicone may improve the wettability before adding plasma treatments or Hydra-PEG.
Unfortunately, experience will remind us there is no material that can be universally used for every patient, but understanding each one’s properties can help us make the best choice.
| 1. Bennett ES. Gas-permeable material selection. In: Bennett ES, Henry VA, eds. Clinical Manual of Contact Lenses. 4th Ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2014:89-111. 2. Musgrave CSA, Fang F. Contact lens materials: A materials science perspective. Materials. 2019;12(2):261. 3. Campbell D, Carnell SM, Eden RJ. Applicability of contact angle techniques used in the analysis of contact 4. Ghormley NR. Specific gravity–does it contribute to RGP lens adherence? Int Contact Lens Clin. 1991;18:125. 5. Bennett ES. GP insights: how high index GP materials will impact your practice. CL Spectrum. February 2009. 6. MatWeb material property data. Shore (durometer) hardness testing of plastics. www.matweb.com/reference/shore-hardness.aspx. Accessed March 19, 2019. |


