Specialty contact lenses have taken optometry by storm. Although optometrists have been fitting these medical devices for decades, booms in technology, education and training have encouraged more clinicians to use them to enhance the vision, health and well-being of patients.
Each specialty contact lens modality—including rigid gas permeable (GP), hybrid, piggyback and scleral contact lenses—has its own pros and cons and can be applied to a broad array of conditions.1 For example, GPs can improve visual outcomes in children who suffer from ocular trauma and the quality of life for people with keratoconus.2-4 Scleral lenses can aid patients with ocular surface disease, combat corneal neovascularization and help treat persistent corneal epithelial defects.5-7
These corneal disease cases and their fitting considerations demonstrate how scleral lenses and GPs can improve patients’ livelihoods.
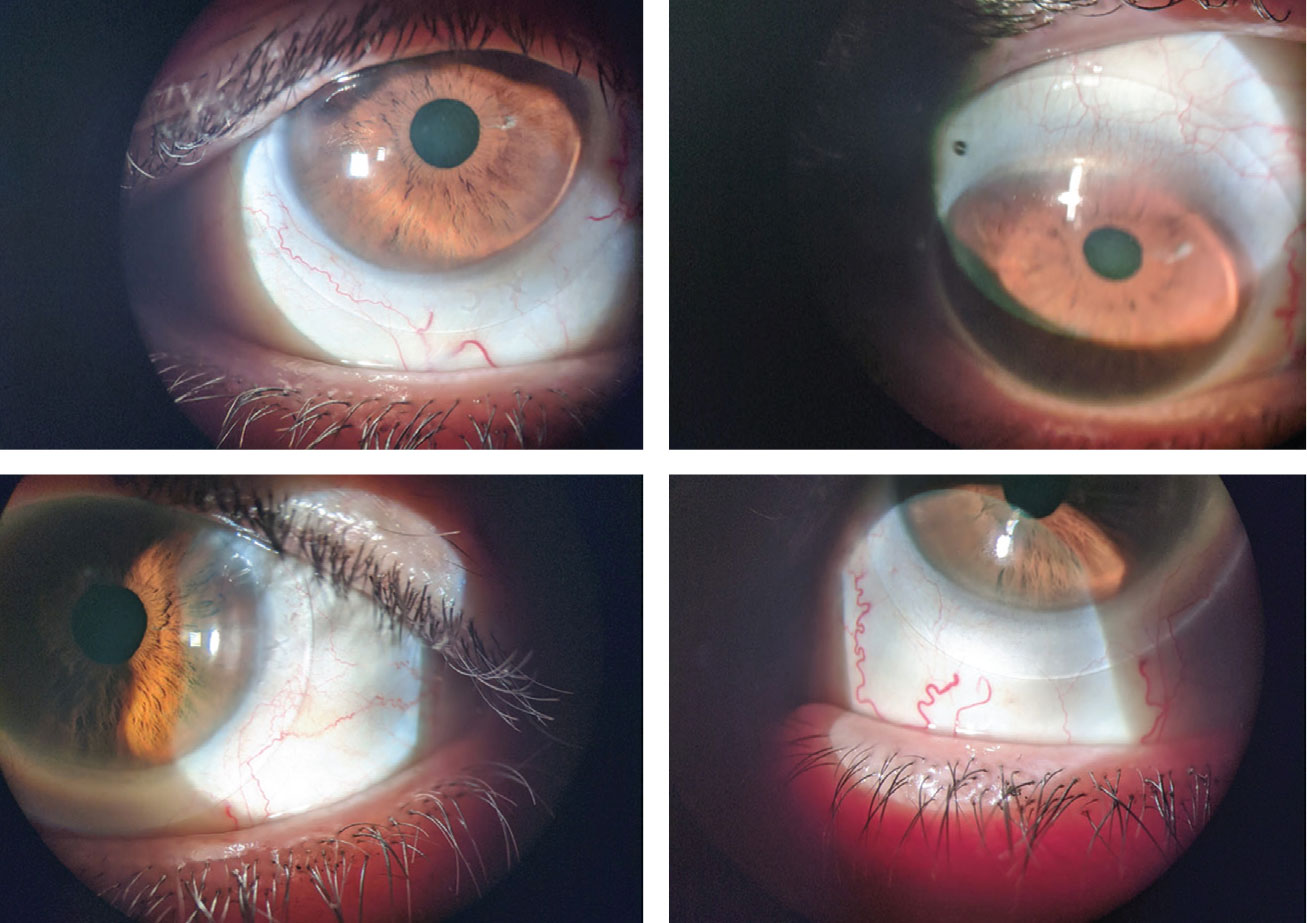 |
| The patient in case 1 was fit with scleral lenses (OD on top). Click image to enlarge. |
Case 1: Post-refractive Surgery Ectasia
A 69-year-old Caucasian female presented for a scleral lens evaluation. She underwent a scleral lens fitting in both eyes four years prior and had not been to an eye doctor since. With her lenses in place, she reported discomfort, worsening vision in both eyes and pain upon lens removal.
Ocular history was significant for LASIK and post–refractive surgery ectasia in both eyes. Scleral lenses were initially fit to improve the poor vision that had resulted from the loss of corneal integrity, which is commonly associated with corneal thinning, steepening, a decrease in visual acuity and induced irregular astigmatism.8
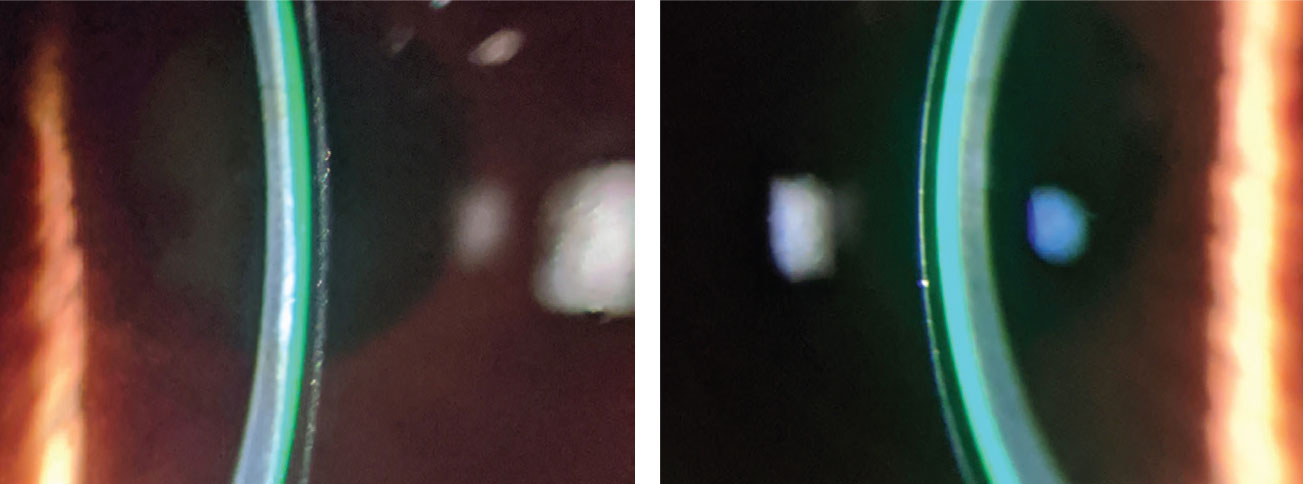 |
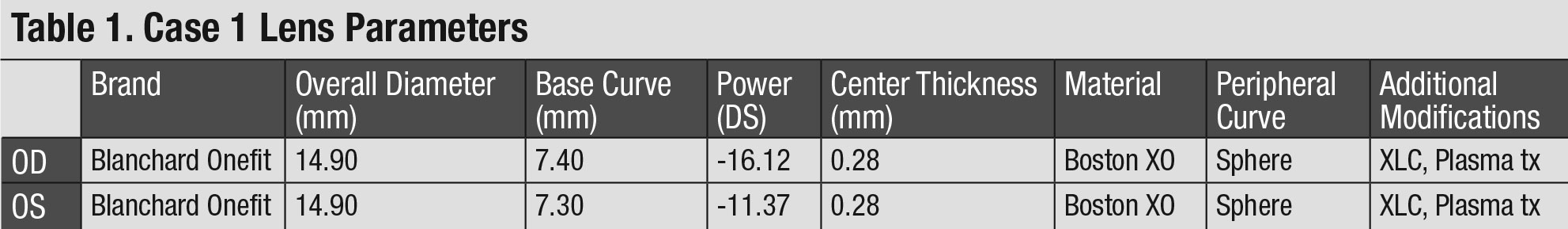
| The first case’s patient’s scleral lens fit displayed adequate central clearance (OD on the left). Click image to enlarge. |
The patient’s best-corrected distance visual acuities (BCDVAs) with scleral lenses were 20/30-2 OD and 20/30- OS. A scleral lens evaluation after two hours of wear revealed no central corneal clearance and significant 360° compression of the bulbar conjunctiva in both eyes. Compression of the bulbar conjunctiva can cause a number of problems, such as irritability, and was likely the culprit of the patient’s discomfort and pain after removing the lenses.9 A significant conjunctival compression ring was evident after removing the lenses.
After a short washout period, a diagnostic scleral lens fit was performed in both eyes. Diagnostic lenses with a small sagittal depth (sag) were selected to mimic the shape of the patient’s oblate corneas. The fit was acceptable with the exception of inadequate limbal clearance. After the appropriate adjustments to the lens parameters were made, new scleral lenses were ordered (Table 1).
The patient reported improved vision and comfort with the well-fitting lenses at the dispensing visit and was later able to wear them throughout the day without issue. BCDVAs improved to 20/25+ OD and 20/20 OS. The scleral lenses were finalized, and the patient has been wearing them successfully ever since.
 |
Takeaway #1. Because LASIK results in a flat cornea (even though steepening occurs with post-refractive surgery ectasia), be sure to fit these patients in a lens with a flatter base curve or a smaller sag to match their oblate corneal shape.
Takeaway #2. Extra limbal clearance can improve areas of insufficient clearance. If a larger limbal clearance is not an option with one scleral design, another may be needed to help achieve appropriate clearance over the limbus.
 |
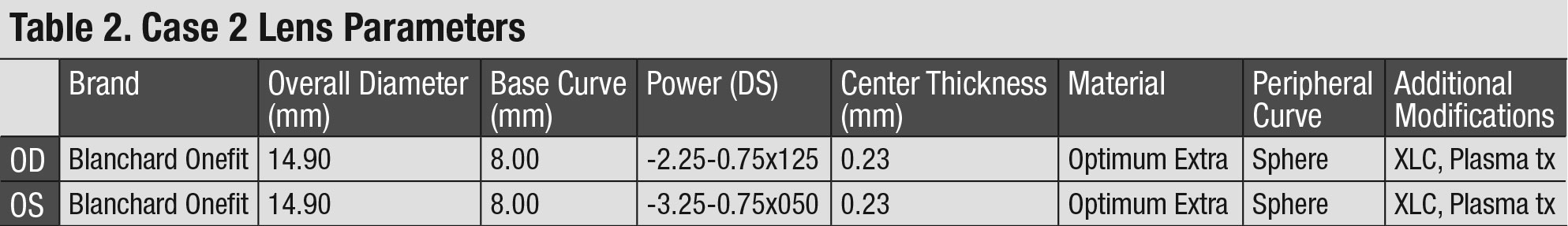
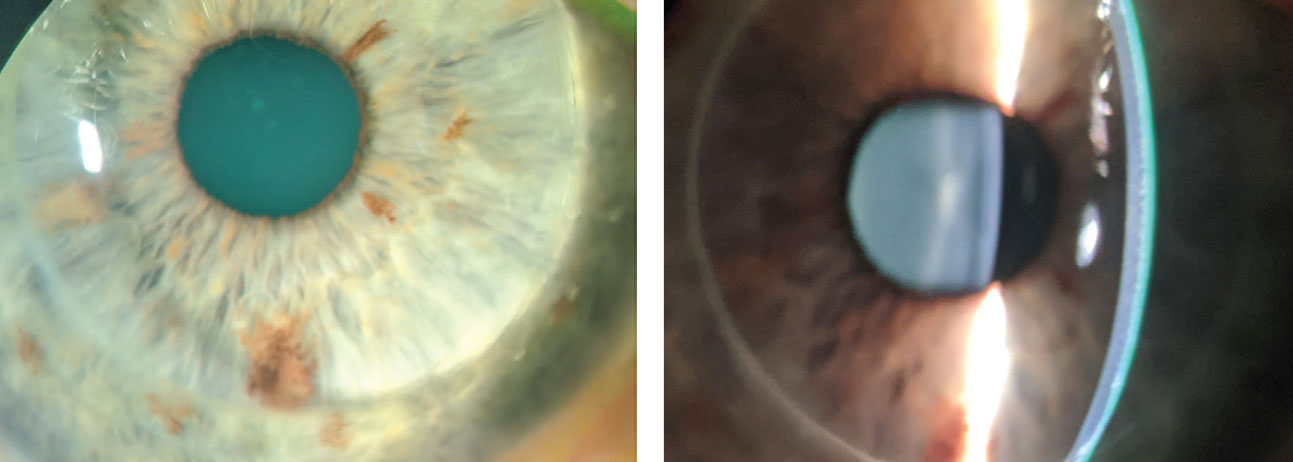
| The patient in case 2 was also fit with scleral lenses, which displayed low central clearance (OD at left). Click image to enlarge. |
Case 2: Keratoconus
A 34-year-old Caucasian male presented for a comprehensive exam and reported that he was overdue for a scleral lens evaluation. He was fit with sclerals three years earlier but had discontinued wear due to his unhappiness with the visual outcome. The patient expressed a desire to get back into scleral lenses to maximize his vision. A slit lamp examination and corneal topography revealed stage II keratoconus in both eyes.
Using diagnostic lenses, the overall fit appeared satisfactory with only minor modifications. The patient reported comfort but disappointment in the 20/25 vision achieved in each eye with a spherical over-refraction. A spherocylindrical over-refraction (SCOR) assessed for residual astigmatism that results from internal refractive components of the eye, mainly the crystalline lens, the posterior cornea or both.10 Corneal topography scans with the lenses in place ruled out flexure as a cause of residual astigmatism. The SCOR revealed -0.75D of residual astigmatism in each eye, the addition of which improved the BCDVA to 20/20+ in each eye.
The acceptable levels of visual acuity and refractive residual astigmatism (both are subjective measurements) guided the decision to order the first trial pair of scleral lenses without astigmatic correction.
Upon dispensing the scleral lenses, the fit and comfort were excellent, but the patient still reported dissatisfaction with the visual results. Repeat SCOR showed that -0.75D of residual astigmatism remained in each eye. Lens stability and rotation was confirmed, and new lenses were ordered with the addition of astigmatic correction in a front-surface toric design (Table 2). The patient was pleased with the vision improvement gained from the second trial pair, which yielded 20/15-2 in each eye. The overall fit and comfort were satisfactory.
At follow-up, central clearance was low, measuring 75μm in each eye after 10 hours of wear time. While no universally accepted value for central clearance exists, most scleral lens practitioners prefer a range of 100μm to 200μm. One study reported an optimum central clearance range of 50μm to 200μm after settling.11 A number of experienced specialty contact lens fitters believe some central bearing with scleral lenses may even be well tolerated compared with GPs.12
Central clearance aside, the rest of the scleral lens fit looked great, the comfort was excellent and no ocular surface complications (e.g., microcystic edema, limbal staining) were present after lens removal. The lenses were dispensed, and the patient has been successfully wearing them ever since.
 |
Takeaway #1. Perform a SCOR when suspicions of residual astigmatism arise. However, it may be worth forgoing astigmatic correction in scleral lenses until the patient returns for a follow-up, at which time a SCOR can be repeated to determine if astigmatic correction is the same and reasonable to add.
Takeaway #2. Work within your comfort level. Different doctors may have different reactions to the low central clearance described in this case. In these instances, sometimes the thought that the enemy of good is better comes to mind.
 |
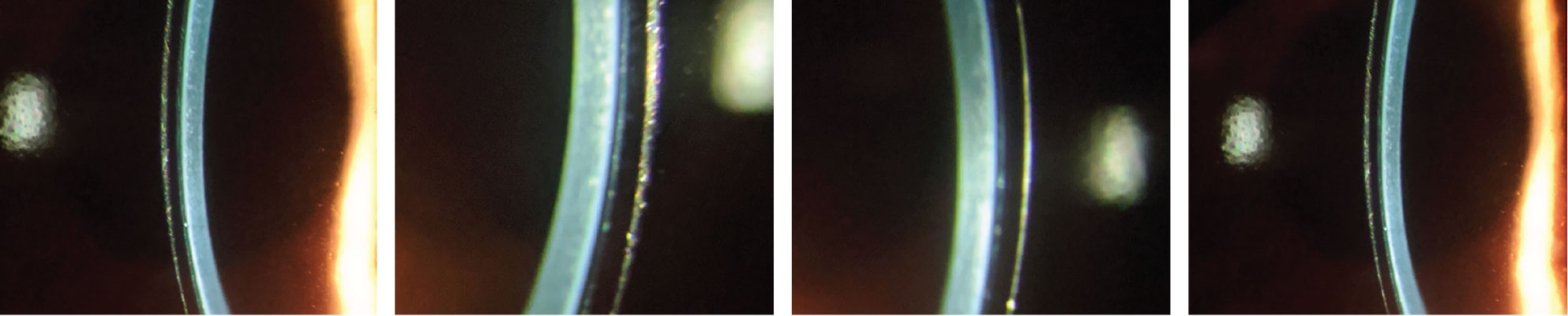
| The patient in case 3 had a PKP in his right eye (left). An optic section highlights the graft-host junction of the PKP. Click image to enlarge. |
Case 3: Penetrating Keratoplasty
A 51-year-old Caucasian male was referred for a contact lens examination. He had worn GPs for years but noticed a steady decline in vision and reported longstanding lens awareness. His most recent pair of GPs was two years old. His ocular history was significant for a successful penetrating keratoplasty (PKP) in the right eye and stage III keratoconus in the left eye.
BCDVA with the GPs was 20/30-2 OD and 20/30- OS. Evaluation revealed a flat fit with excessive inferior edge lift in the right eye and a steep fit in the left eye. Excess edge lift is a common cause of lens awareness, discomfort or both.
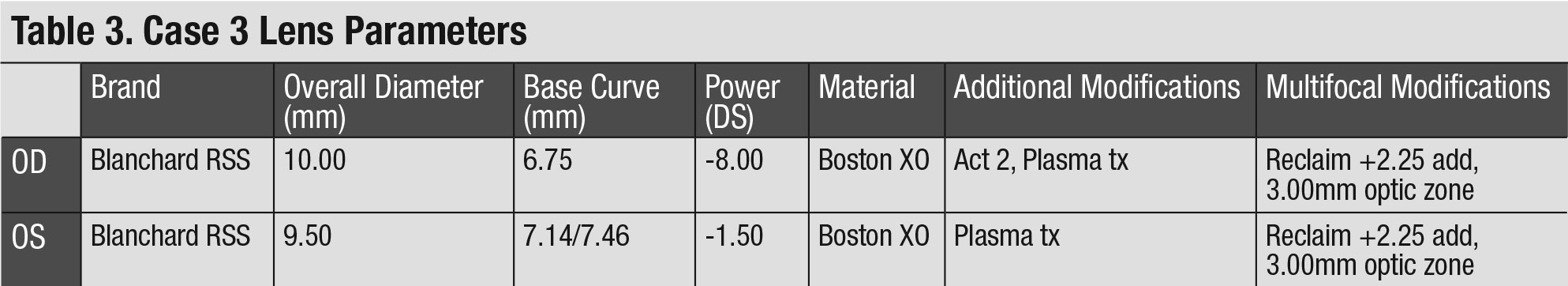
The patient was successfully refit with GPs that had a post-graft design in the right eye and a keratoconic design in the left eye. Because the initial right trial lens demonstrated excessive inferior edge lift, asymmetric corneal technology (ACT) was added to improve edge lift. Different grade levels for ACT exist depending on the required lift change.
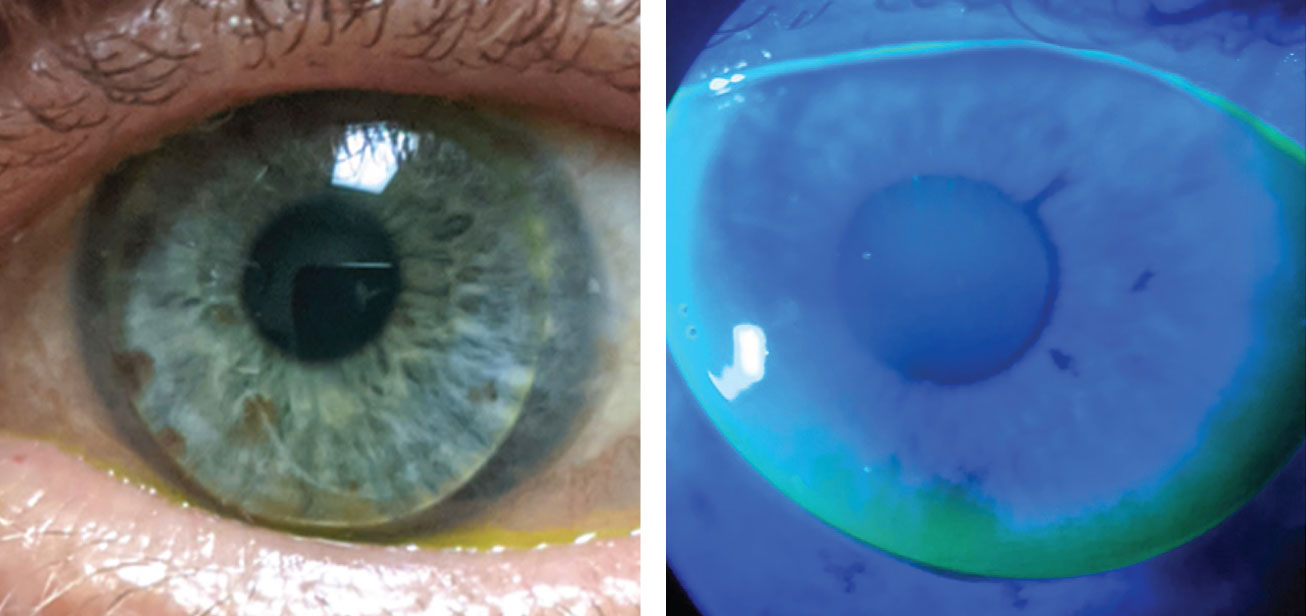 |
| The patient in case 3 had keratoconus in his left eye and slight, but acceptable, inferior edge lift remains after ACT adjustment in the right eye. Click image to enlarge. |
With the newly designed GPs, the patient experienced improved distance vision and a noticeable increase in comfort, which was likely attributable to an improved inferior edge lift design via an ACT grade two modification. Slight inferior edge lift remained with the right lens, but further enhancement was deferred, as there were no stability or comfort issues.
The patient did, however, report difficulty completing near tasks. He worked as a handyman and found his growing dependence on reading glasses inconvenient. Multifocal GPs were discussed as an option to improve the patient’s functionality, and he decided to move forward with a multifocal GP fitting.
The patient was fit in the same GP lenses as above with the addition of an aspheric front surface design to incorporate a near add. Trial lenses were ordered to integrate over-refraction adjustments for both lenses (Table 3).
At the dispensing visit, the patient’s distance and near vision were checked binocularly, as is customary with multifocal contacts. A BCDVA of 20/25+2 was achieved with a near visual acuity of 20/25+. The new GPs demonstrated a significant improvement in near vision.
At follow-up, the patient reported enhanced functionality at work and less reliance on reading glasses.
 |
Takeaway #1. Become familiar with contact lens designs. In this case, a specific change was made using ACT to improve excess inferior edge lift, resulting in improved patient comfort and lens stability.
Takeaway #2. Specialty lens practitioners are eager to achieve optimal results. When paired with a motivated patient, success is achievable. The complexity of this case may have been daunting, but tackling the challenge improved the patient’s quality of life.
Discussion
Advancements in scleral lens education, training and marketing have pushed this modality to the forefront of the specialty contact lens market. Many optometrists now consider these lenses the first-line option for maximizing health and vision.
As optometrists become more comfortable with scleral lens fitting, they should not forget the benefits of GPs. In many instances, GPs may be the best specialty contact lens option for irregular eyes.
Remember that this subcategory of optometric care does not revolve entirely around simply fitting contact lenses. Rather, we are using medical devices to treat and manage complex ocular surface conditions. It is easy to get lost in the wonders of specialty contact lenses and forget that the patients who benefit from them will likely need ongoing medical care, a role optometrists should feel comfortable embracing.
While laboratory consultants can be a tremendous resource, every practitioner should develop enough familiarity and knowledge about lens designs to troubleshoot issues themselves. Tapping into the brain of lens consultants can be extraordinarily useful, but it is no substitute for understanding how to fit your own patients.
The specialty contact lens market is continually expanding. These medical devices provide a unique opportunity to improve the vision, comfort and health of patients. As advancements progress, so do future applications. The possibilities leave a lot to be excited about.
Dr. Lopez graduated summa cum laude from the University of Houston College of Optometry. He practices in Wisconsin with a focus on ocular pathology and specialty contact lenses.
| 1. Andrzejewski T, Gelles J. Irregular corneas meet their match with GP lenses. RCCL. 2020;157(3):22-5. 2. Elseht RM, Nagy KA. Rigid gas permeable contact lens as a vision-sparing tool in children after traumatic corneal laceration. J Pediatr Ophthalmol Strabismus. 2018;55(3):178-81. 3. Pradhan ZS, Mittal R, Jacob P. Rigid gas-permeable contact lenses for visual rehabilitation of traumatized eyes in children. Cornea. 2014;33(5):486-9. 4. Wu Y, Tan Q, Zhang W, et al. Rigid gas-permeable contact lens related life quality in keratoconic patients with different grades of severity. Clin Exp Optom. 2015;98(2):150-4. 5. Schornack M, Nau C, Nau A, et al. Visual and physiological outcomes of scleral lens wear. Cont Lens Ant Eye. 2019;42(1):3-8. 6. Yin J, Jacobs DS. Long-term outcome of using Prosthetic Replacement of Ocular Surface Ecosystem (PROSE) as a drug delivery system for bevacizumab in the treatment of corneal neovascularization. Ocul Surf. 2019;17(1):134-41. 7. He X, Kendall D, Quinones VLP, et al. Case series: overnight wear of scleral lens for persistent epithelial defects. Optom Vis Sci. 2018;95(1):70-5. 8. Wolle MA, Randleman JB, Woodward MA. Complications of refractive surgery: ectasia after refractive surgery. Int Ophthalmol Clin. 2016;56(2):129-41. 9. Denaeyer GW, Michaud L. Scleral Lens Troubleshooting. Cont Lens Spect. August 1, 2017. 10. Ensley R, Miller H. The toric toolbox: don’t forget GPs. RCCL. 2016;153(8):8-9. 11. GP Lens Institute - Scleral Lens Education Society. Scleral lens troubleshooting FAQs. www.gpli.info/pdf/GPLISLSTSGuide11017.pdf. Accessed September 17, 2020. 12. Van der Worp E. A Guide to Scleral Lens Fitting. 2nd ed., Pacific University College of Optometry, 2015. |


