 |
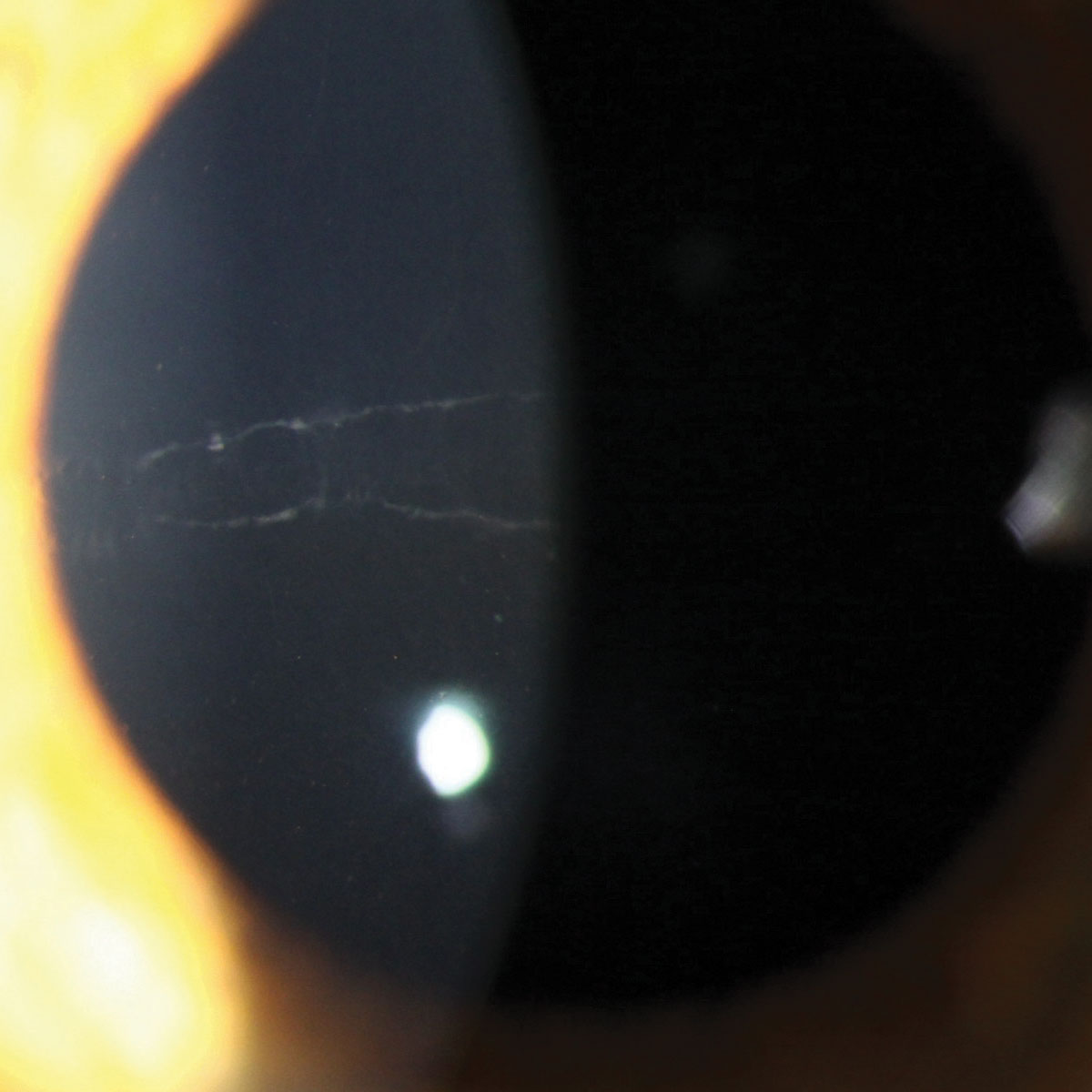
A 14-year-old boy presented with bilateral decreased vision. Ocular examination showed gray linear deposits on the posterior central cornea but no edema. The patient was refractable to 20/40 OD, 20/30 OS. Gonioscopy did not reveal anterior synechiae. His intraocular pressures (IOPs) were 16mm Hg OD and 17mm Hg OS.
The patient was given his refractive correction and counseled about posterior polymorphous dystrophy (PPMD), a rare autosomal-dominant dystrophy that causes abnormal developmental differentiation of endothelial cells. It can present in early childhood, but symptoms generally appear in the second or third decade.1
While corneal dystrophy is, by definition, a bilateral condition, PPMD may be asymmetric or unilateral.1
PPMD is best viewed at the slit lamp by retroillumination with a widely dilated pupil. It appears as gray collagenous tissue at the level of Descemet’s membrane and can form various shapes, including isolated dots, diffuse clusters or linear lesions.
Lesions range from small (0.1mm to 1mm) vesicles to bands anywhere from 2mm to 10mm in length. These are differentiated from tapered, smooth-edged Descemet’s tears seen in congenital glaucoma, trauma and hydrops by the presence of parallel scalloped edges; they also do not taper toward the ends. Numerous other dystrophies are in the differential.
PPMD generally does not progress and can remain unchanged for many years. However, patients should be monitored for endothelial decompensation. It is rarely extensive enough to cause visual impairment; however, band keratopathy or stromal clouding can develop. There can be peripheral iridocorneal adhesions in about 25% of cases. IOP should be monitored, as it will be elevated in about 15% of cases.1
While asymptomatic cases do not require treatment, patients with corneal edema, vision decrease or increased IOP require intervention. Mild corneal edema can be managed with sodium chloride 5% drops and ointment, a soft bandage contact lens for ruptured bullae, and stromal micropuncture for areas of localized swelling and poor endothelial adherence.2 Severe cases may require surgical intervention, such as some form of corneal transplantation or glaucoma surgery. The presence of anterior synechiae signifies a poor visual prognosis.
 |
| Click photo to enlarge. |
1. Dahrouj M, Vislisel JM, Raecker M, Maltry AC, Goins KM. Posterior Polymorphous Corneal Dystrophy (PPMD). www.eyerounds.org. Accessed Aug. 21, 2018. 2. The IC3D Classification of the Corneal Dystrophies. Cornea. 2008;27(Suppl. 2). |


