While it’s no secret that scleral contact lenses can provide massive visual benefits to patients, fitting these lenses can have a steep learning curve. With the emergence of new technologies, such as scleral topographers, the initial challenges are much easier to overcome, particularly for practitioners new to scleral lens fitting. Even for experienced fitters, the use of these topography systems can provide many benefits. This article aims to discuss the currently available scleral topographers and how to best use them to maximize fitting success by boosting clinical acumen, improving contact lens fits and generating revenue.
Empirical Fitting
Scleral lenses can vastly improve visual acuity in a variety of their indicated uses, particularly in conditions like corneal ectasia.1 Before the fit, it can be easy to promise your patients a marked improvement in both vision and ocular comfort, only to have the patient discouraged by going through two, three, sometimes even six or more trial lenses while looking for the optimal fit and/or an improvement in vision. This issue is further compounded as recent studies have shown that a majority of scleras have asymmetric topography, completely independent of their corneal topographic counterparts.2,3 That news can be discouraging to the practitioner as well, as dealing with this can take up valuable chair time. Scleral topographers can expedite the fitting process by providing the ability to fit empirically—similar to how many of us already fit corneal gas permeable (GP) lenses.
The first advantage to empirically guided scleral lens fits addresses the scenario previously outlined: you only need one diagnostic trial lens. Scleral topographers can map out the scleral surface and provide the patient with a custom-designed lens, unique to that particular eye. This effectively eliminates the need for the trial-and-error process of finding the trial lens that best fits the patient’s eye. Once the scleral surface is mapped, a best-fit lens is generated and available to order. The only trial lens necessary is simply used to calculate over-refraction, trial lens fit be damned.
The second advantage to empirically guided scleral fits is chair time. Most practitioners have their ancillary testing instruments separate from the exam rooms, which means three things. First, the patient is no longer in the exam room as you test the many different trial lenses previously mentioned, meaning it frees up the time that would have been spent in the room with the patient doing trial-and-error. Next, the entire fitting process can be done before the patient enters the exam room. Both of these chair time–saving consequences not only save the practitioner’s time but also the patient’s.
Lastly, you no longer have to have the patient return to clinic for multiple repeat visits as you reorder and reorder lenses—the fit is nailed down within the first one or two. This not only saves chair time on the day of initial lens fitting but also lessens the demand for lens fitting follow-ups, which frees up future chair time.
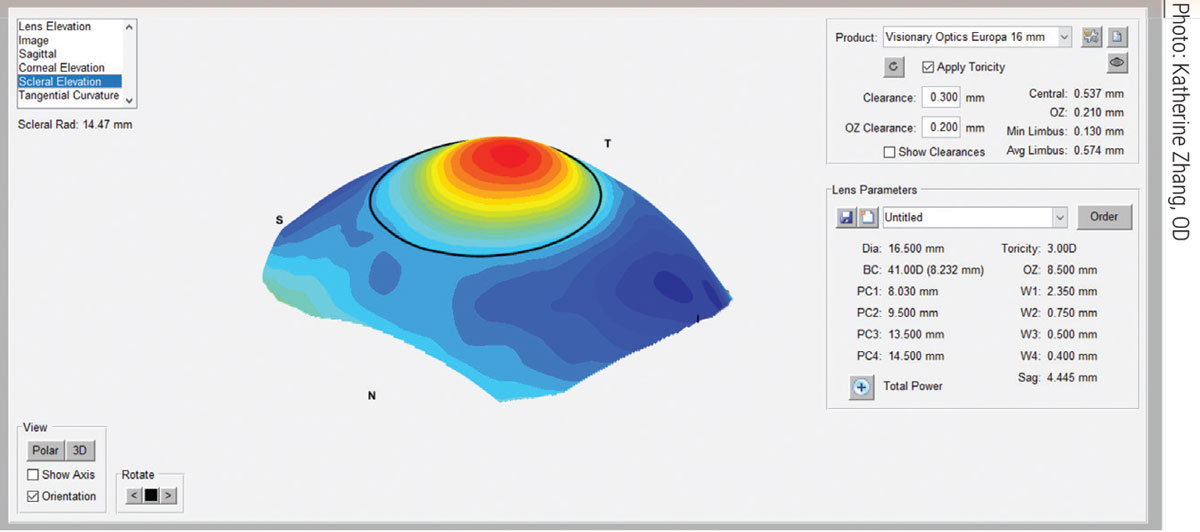 |
The sMap 3D scleral elevation map after image-stitching. Click image to enlarge. |
Pathologic Elevation
Pingueculae, irregular corneal transplant graft tissues and other pathologic ocular surface elevations like Salzmann’s nodular degeneration can all make scleral lens fits quite difficult. In some conditions, such as filtering blebs or tube shunts in glaucoma patients, traditional scleral lens fit can even be contraindicated. With the traditional best-fit trial lens approach, fitting over these ocular surface elevations often requires heavy lens modifications such as notching, peripheral lens elevations, quadrant-specific designs or truncations.
All these processes can require many trial lenses, frequent consultation with the manufacturing lab and sometimes even in-office lens modifications (e.g., getting out a dremel and modifying the lenses yourself). Even if an adequate lens fit is achieved after all these steps, it can prove to be a frustrating and time-consuming process.
Perhaps one of the biggest selling points of scleral topographers is their ability to create freeform lenses. Such lenses are not spherical and are often asymmetric with multiple meridians of toricity or highly irregular surfaces. The first big advantage to freeform lenses is that they can vault these pathologic elevations, without sacrificing other lens parameters such as diameter or base curve. The second advantage: practitioners oftentimes no longer need to rely on complicated lens modifications such as notching or truncations because of freeform lenses’ ability to vault these lesions.
Current Topographers
There are three currently available scleral topographers that can provide scleral profilometry data. Let’s discuss how each device could benefit an optometrist and their practice.
sMap 3D (Visionary Optics). This device maps over one million data points on the ocular surface, covering an approximate 22mm range of the sclera, with a precision of 10µm.4 It is integrated with Visionary Optics’s Europa and Latitude lens designs. Europa is a standard scleral lens capable of many different modifications, such as toricity, quadrant-specific modifications, truncation and more. Latitude is the company’s freeform lens design that allows for a more exact matching of the ocular surface.
This instrument makes use of sodium fluorescein (NaFl) for its image acquisition. So, from a protocol standpoint, it would go something like this: have the patient sit in front of the sMap 3D device, instill NaFl, perform image acquisition in three gazes (straight ahead, up-gaze and down-gaze). These images are then “stitched” together to one complete ocular surface profile. Lens parameters will be displayed, and you can adjust to your liking or continue with the recommended parameters. Whether that be a best-fit Europa lens or the free-form Latitude lens, the produce is available for order directly from the device.
 |
|
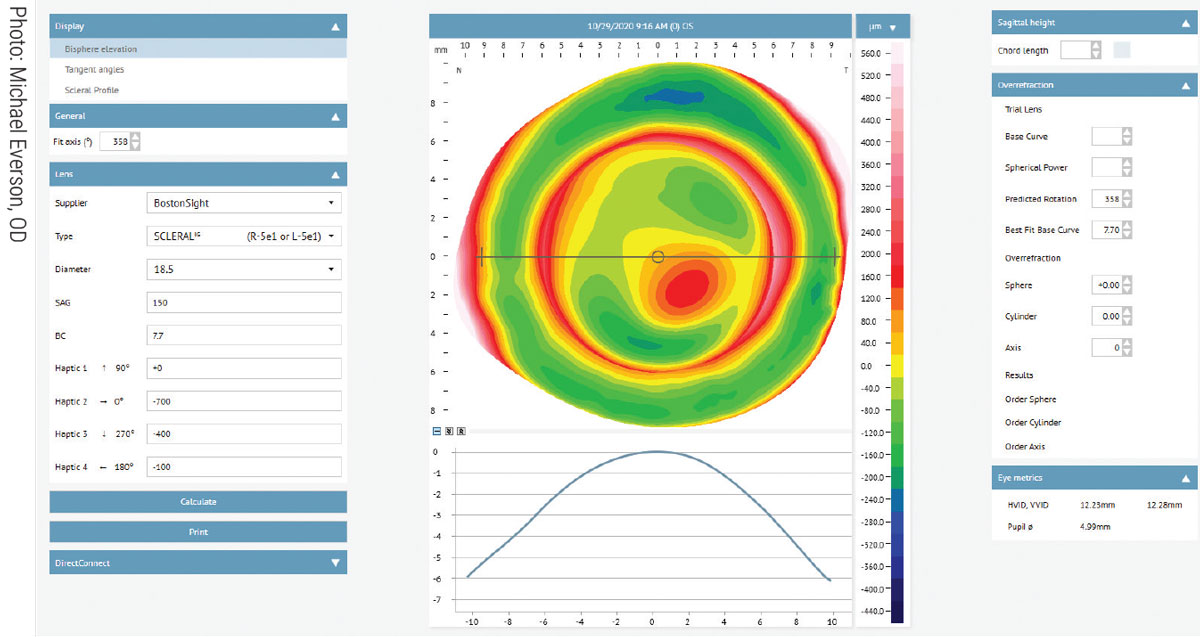
Eaglet-Eye ESP software image of a patient diagnosed with corneal ectasia. Click image to enlarge. |
Eye Surface Profiler (Eaglet-Eye). This instrument is a scleral topographer from Eaglet-Eye. It maps over 350,000 data points, covering a 20mm diameter of the sclera, with an accuracy of 10µm over the sclera (and 2µm to 3µm over the cornea).5 Eaglet-Eye does not manufacture scleral lenses in-house, and instead has partnered with 19 scleral lens labs, some of which are listed here: ZenLens (all sclerals), BostonSight (BostonSight Scleral), Blanchard (all Onefit designs), EyePrint Prosthetics (ScanFit Pro), Acculens (Maxim), X-Cel (Atlantis), Advanced Vision Technologies (Naturalens Scleral), ValleyContax (Custom Stable) and SynergEyes (VS Scleral and Ultrahealth Hybrids). A complete list is available on their website.
In addition to scleral lenses, this device can also be used for GP, hybrid, orthokeratology and even custom soft lens designs (with a compatible lens manufacturing lab).
The Eye Surface Profiler also uses NaFl for image acquisition, as it is usually applied to both superior and inferior sclera. From there, the eyelids are opened and a single image is acquired while the patient is in primary gaze. Once the corneoscleral topography plot is displayed, the practitioner then has the option of adjusting parameters and choosing which manufacturing lab and lens design to proceed with. The device will automatically generate a best-fit lens based on the design of your choosing. Many of the manufacturing labs allow for direct data transmission from the device to the lab through the Eaglet-Eye ESP “DirectConnect” software module.
Pentacam (Oculus). The Pentacam is familiar to most eye care practitioners as a Scheimpflug corneal topographer. However, Oculus now offers a cornea/scleral profile (CSP) module that can detect scleral topographic properties in addition to corneal ones. There are currently three models of the device: Pentacam, Pentacam HR and Pentacam AXL Wave. At the time of publication, the HR and AXL Wave models do not support the CSP module.
The CSP module acquires 250 images for over 100,000 data points, covering an 18mm diameter of the cornea and sclera.6 Pentacam also supports a variety of external manufacturing labs such as EyePrint Prosthetics, Valley Contax, Bausch + Lomb and others. This technology also supports RGP and other specialty contact lens designs on a per-lab basis.
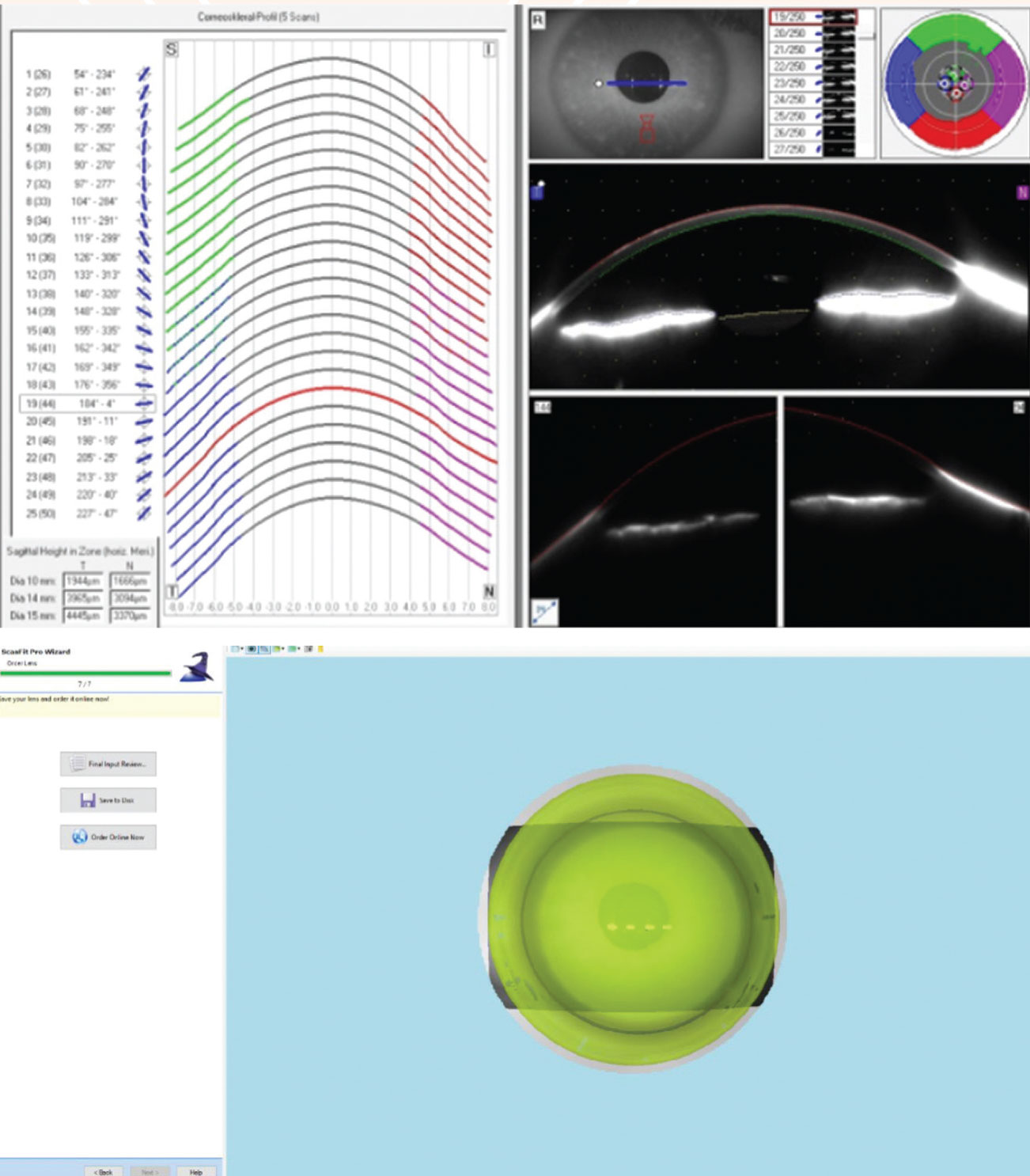 |
|
Scheimpflug imaging of the corneoscleral surface (top). The same data translated through ScanFit Pro software (bottom). Click image to enlarge. |
As mentioned above, the Pentacam relies on Scheimpflug imaging for image acquisition, so it does not require the use of fluorescein. This may be advantageous for fitting patients with dry eyes or with low tear production. To begin, the patient puts their chin in the rest, and the Pentacam takes 250 images throughout a series of five gazes (up, down, left, right and primary gaze). These images are then stitched together to create an ocular surface profile.
This data can then be used for Oculus’s in-house Wave lens or can be sent to your lab of choice via compatibility with external software such as BostonSight’s BostonSight Scleral, EyePrint Prosthetics’s ScanFit Pro or Valley Contax’s Custom Stable, for example.
Impression-Based Lenses
While not technically scleral topography, impression-based technology can offer similar benefits. The most common impression-based technology is from EyePrint Prosthetics (EyePrint Pro). EyePrint Prosthetics offers three lens designs. The first is the EyePrint Pro lens, capable of constructing an exact replica of the ocular surface, regardless of pathology like filtering blebs, tube shunts and even symblepharon.
The company’s middle tier offering is the EyeFit Pro—also an impression-based design. This lens also creates an exact replica of the ocular surface, but is for slightly less irregular surfaces, such as corneal ectasia, post-traumatic ocular surfaces, irregular corneal transplants and Salzmann’s nodules. Finally, its newest offering is the ScanFit Pro. This one is the most affordable lens design and is used in conjunction with the aforementioned scleral topographers, foregoing the impression process completely. It is typically used for corneal ectasias, pingueculae and other small surface nodules. All lens offerings from EyePrint Prosthetics are freeform technology.
Combining Technologies
Scleral topographers can also be used in tandem with other instruments to create some truly unique designs, which further widens the breadth of what can be corrected. One example is decentered optics. This concept is useful in patients with irregular pupils (e.g., post-trauma patients) or abnormal visual axes (e.g., scarring, corneal ectasia, corneal transplants).
Another example of combining technologies is higher-order aberration (HOA) correction. We know that many ocular surface conditions, most notably corneal ectasia, cause an increase in HOAs. Because freeform scleral lenses typically do not show marked rotation on the ocular surface, this makes them an ideal solution for HOA wavefront correction, which in turn can be quite significant to improving visual acuity in many patients.7
 |
| Click image to enlarge. |
Takeaways
Scleral topography and profilometry can be excellent tools both for those practitioners new to scleral lens fitting and those who are expert fitters already. These devices allow for the elimination of the traditional “trial-and-error” process of scleral lens fitting—empirically providing either the best-fit lens or freeform lenses that match the ocular surface on a micron scale. This can help you save time and money while ensuring optimum comfort and vision for your patients. They can also be combined with existing technologies such as HOA correction and decentered optics to create truly personalized options per patient, per eye.
Traditionally, fitting scleral contact lenses can be complicated. While the best way to learn more about scleral lens fitting and the treatment of ocular surface conditions is to get involved by going to conferences, talking with colleagues and seeking out mentors and using and understanding emergent technology like scleral topographers can greatly reduce the steep learning curve, making life easier for both the patient and the practitioner alike.
Dr. Noyes is a clinical assistant professor of ophthalmology and visual sciences at the University of Iowa Carver College of Medicine. He is a Fellow of the American Academy of Optometry and of the Scleral Lens Society.
1. van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: a review. Cont Lens Anterior Eye. 2014;37(4):240-50. 2. Consejo A, Llorens-Quintana C, Bartuzel MM, et al. Rotation asymmetry of the human sclera. Acta Ophthalmologica. 2018;97(2):e266-70. 3. DeNaeyer G, Sanders D, van der Worp E, et al. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer. JCLRS. 2017;1(1):12-22 4. Visionary Optics. sMap3D. www.visionary-optics.com/smap3d. Accessed August 15, 2021. 5. Eaglet Eye. The ESP—Eaglet Eye. www.eaglet-eye.com/the-esp. Accessed August 15, 2021. 6. Maller K. Pentacam CSP software to improve efficiency and efficacy of complex custom scleral lens design. Modern Optometry. modernod.com/articles/2019-apr-supplement/pentacam-csp-software-to-improve-efficiency-and-efficacy-of-complex-custom-scleral-lens-design. Published April 2019. Accessed August 15, 2021. 7. Rijal S, Hastings GD, Nguyen LC, et al. The impact of misaligned wavefront-guided correction in a scleral lens for the highly aberrated eye. Optom Vis Sci. 2020;97(9):732-40. |


