 |
A 67-year-old male presents with complaints of bilateral ocular pain and photophobia, increasing in severity over the past week. He says the pain is an 8/10 and nothing relieves the discomfort, and he prefers a dark room with his eyes shut. His medical history is only significant for hepatitis C.
 |
|
Click image to enlarge. |
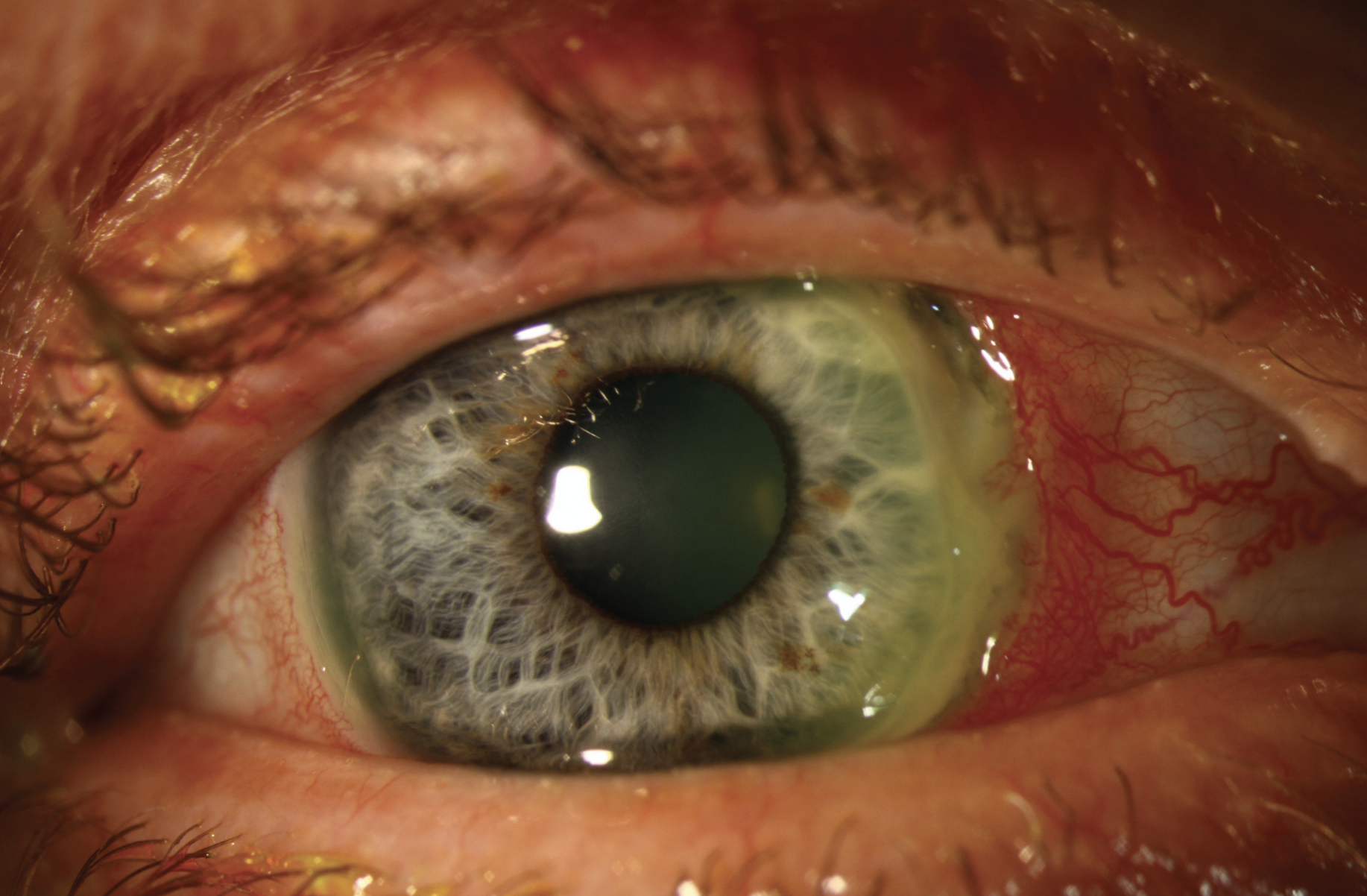
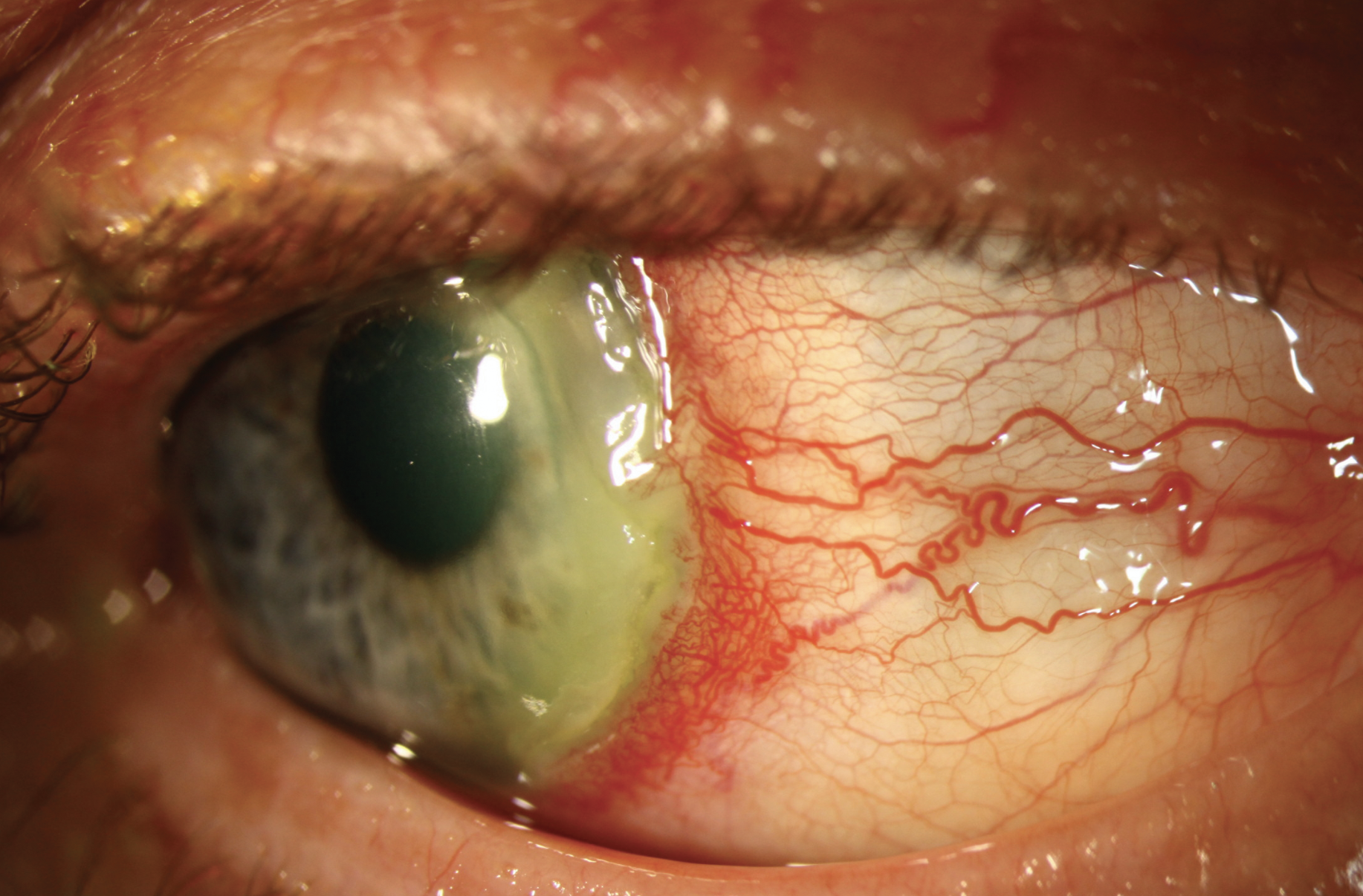
On ocular examination, deep guttering and staining is seen adjacent to the limbus nasally OD and temporally OS, both spanning six clock hours, with areas of exceedingly thin stroma at risk for perforation. He was diagnosed with peripheral ulcerative keratitis (PUK) and started on moxifloxacin TID OU, vitamin C 2000mg daily, doxycycline 100mg BID and ibuprofen 800mg TID. He was also fit with a scleral lens and referred to rheumatology for systemic evaluation.
Causes and Interventions
PUK is associated with autoimmune diseases such as Sjögren’s syndrome, granulomatosis with polyangiitis, relapsing polychondritis, systemic lupus erythematosus, polyarteritis nodosa and most commonly with rheumatoid arthritis. Differential diagnoses includes Mooren’s ulcer and Terrien’s marginal degeneration. PUK (also known as corneal melt) develops when there is an imbalance between specific collagenase (MMP-1) levels and tissue inhibitors (TIMP-1). This imbalance can cause keratin in the corneal epithelium to break down rapidly. As the stroma thins, the eye is at risk for corneal perforation, which can lead to vision loss.
 |
| Click image to enlarge. |
In addition to topical antimicrobials, oral doxycycline is used for its anti-collagenase activity, along with oral vitamin C to promote collagen synthesis and stromal repair. Topical corticosteroids should be avoided because of the risk of accelerating keratolysis and suppressed wound healing. Topical 1% medroxyprogesterone acetate (compounded drop) may be helpful in cases of PUK because it reduces inflammation and promotes collagen repair. Scleral lenses are helpful by keeping the ocular surface moist and preventing exposure-related breakdowns of the epithelium. In addition, scleral lenses improve ocular comfort and decrease inflammation.
Systemic immunosuppression is often required to control ocular inflammation. Initial treatment is with oral steroids, prednisone (1mg/kg/day) or methylprednisolone (1g/day x 3 days). In cases with impending perforation not controlled by steroids, or in patients with rheumatoid arthritis who are at risk for vascular events, steroid-sparing agents are used. These include antimetabolites such as methotrexate, azathioprine or mycophenolate mofetil, T-cell inhibitors such as cyclosporine or tacrolimus, alkylating agents such as cyclophosphamide and chlorambucil, and biologic agents such as infliximab and rituximab.
Management Course and Prognosis
Our patient reported significant improvement in comfort with scleral lens fitting with an extended wear application. He was cautioned that significant mucin would build up under the lens, which would look terrible but was not harmful. The lens was removed in office every several days and cleaned and sterilized. Systemically, he was started on mycophenolate, since the more commonly used methotrexate is contraindicated in someone with liver-concerning diseases, such as hepatitis C. It is our recommendation that 24/7 application of the scleral lens, as well as aggressive oral and systemic therapies and comanagement, should continue until the guttering has filled in and the eyes are no longer at risk for perforation. This is not a fast process and may take months to see improvement.
1. Singh G, Salvador VB, Bagchi A, Tushabe R, Abrudescu A. Rheumatoid arthritis-associated corneal ulceration with superimposed infection by methicillin-resistant Staphylococcus aureus: a complicated type of corneal melt. Am J Case Rep. 2014 Nov 27;15:523-5. 2. Sule A, Balakrishnan C, Gaitonde S, et al. Rheumatoid corneal melt. Rheumatology, 2002; 41(6): 705-6. |


