Additionally, the nature of our practice environment for contemporary eye care practitioners (ECPs)—which emphasizes low reimbursements and ever-increasing numbers of patients—makes it difficult to find the time to focus on corneal reshaping. But with myopia on the rise, it’s time we use all of our tools.
I feel ortho-k is the best possible treatment for eligible patients; using the human cornea in its new-engineered shape to limit the progression of myopia has proven hugely successful in my practice. Here are 10 tips to help you successfully integrate ortho-k into yours.
1. Know the Risks and Benefits
Over 80% of orthokeratology fits on adolescents are for myopia control.4 Yet, ECPs are still reluctant to embrace the procedure, possibly because there are few procedures with a higher perceived risk than fitting adolescents with ortho-k. Risk aversion may inform some of this reticence, but a further understanding of the benefits of the procedure proves to overshadow the potential risks such as microbial keratitis, corneal abrasions, central corneal staining, lens binding and tear film instability. The FDA is willing to consider even a 30% reduction in myopia resulting from use of a medical device as clinically significant; orthokeratology—with close to a 50% reduction—serves as the gold standard.
Safety concerns tend to be based more in perception than fact. There are scores of studies showcasing the safety of this procedure.5-8 Out of the 5,000+ ortho-k lenses I’ve fit in the last 25 years, I’ve only had one incident of microbial keratitis. Early diagnosis and treatment, combined with effective antibiotic therapy, kept this patient’s microbial keratitis episode from causing vision loss. My longest wearing ortho-k patient just passed year 25, and his seven diopters of myopia at age seven hasn’t changed. Many of my patients are in year 15 to 20 and still wearing lenses safely. While we have had our share of corneal abrasions and superficial punctate keratitis, these have been easily remedied and haven’t negated the many benefits ortho-k has provided to my patients.
Even spherical aberration, initially thought to be a negative side effect of ortho-k, actually offers many positives when it comes to advanced custom ortho-k lens design. For example, by manipulating the positive asphericity in ortho-k designs, along with reducing the size of the treatment zone, you increase the elevation of the reverse curve, resulting in an increase in spherical aberration with more effective myopia control. Introducing a negative asphericity, however, can help increase add power while also manipulating spherical aberration.
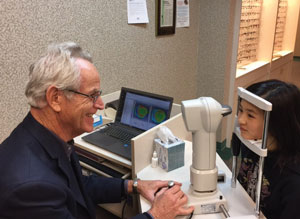
2. Consult and Examine
In my office, we ask that patients attend a free consultation before making an appointment for an ortho-k evaluation. It is crucial that parents accompany any adolescent patients. Often, I find the parents do little to explain ortho-k to their children because they don’t understand it themselves, and the consultation ensures both the parent and the patient are educated properly. During the consultation we answer questions and provide literature on the procedure while also gathering information about a patient’s eligibility. It’s also the perfect time to evaluate first impressions of the maturity level of an adolescent patient. Finally, after reviewing the risks and benefits, you should have parents, and the child if he or she is old enough, sign off on all the key points of an informed consent.
During the initial examination to determine suitability, clinicians must thoroughly rule out all complicating conditions. For example, the presence of any corneal pathology (such as keratoconus) is a contraindication. Practice extra caution when considering cases with irregular, limbus-to-limbus or against-the-rule astigmatism or decentered corneal caps—particularly if you are new to ortho-k. Factors such as dry eye should always be dealt with prior to fitting.
It is extremely important, especially when treating the pediatric population, that your staff knows how to gather this pertinent clinical information so the appointment can be flagged if they note complicating factors.
 |
| Topography needs to be near perfect to ensure a proper fit. |
Following the initial examination is the actual ortho-k evaluation. This should begin with topography, which is the standard-of-care for ortho-k. The baseline topography will remain the reference for a patient’s fitting throughout their lifetime of ortho-k use, so it needs to be performed with great precision, and it’s imperative to take more than one topography reading. It’s not uncommon to need 10 or more readings on a patient per eye to arrive at an accurate assessment of the cornea prior to fitting, considering corneal topographers using a Placido disc are often inaccurate and provide different results each time a map is taken. It can be challenging to know which one of those 10 is the one to use as the reference. In my practice, I take an auto-k reading and match that to the topographies I have taken until I find the closest one to the topography reading. Avoid using topographies with missing data points or irregularities caused by tear pooling or lid infringement.
Topography provides valuable information on the cornea itself, including the much-needed eccentricity; however, be wary of a topographer’s accuracy. Besides pre-fit data, the evaluating treatment progress is one of its greatest benefits. All of the necessary information you need for evaluating the fit is at your fingertips, including axial, tangential, refractive, elevation and difference maps. Axial maps determine the radius of curvature at each particular point, which is helpful in determining the refractive change. Axial maps are also good for determining the type, shape and position of any corneal astigmatism. Tangential maps are best used for lens positioning in ortho-k, while refractive maps speak to the quality of vision. Subtractive or difference maps are ideal for showing the overnight change after ortho-k.
The ortho-k evaluation is also a good time to discuss other considerations such as haloes and adaptation for moderate-to-high myopia. Haloes in younger patients usually aren’t an issue, particularly after explaining how they are integral to the myopia control effect. The change from the prolate to oblate surface created after ortho-k causes haloes as it defines a new myopic image shell on the peripheral retina. Still, it’s helpful to know how sensitive patients are to slightly blurry visual effects such as haloes at distance.
Education is a key to success, so make sure parents and patients understand these myopia-controlling devices are not intended to give the ultimate in fine distance acuity but rather are a method of reducing myopia progression.
Prior to fitting any lenses, discuss how the patient’s accommodative system may need help with vision training during treatment. This is especially true with newer custom designed lenses that address the lack of peripheral defocus in patients with low myopia by creating more demand and a resulting moderately high hyperopia after lens removal during treatment (>1D).
4. Sign a Contract
If at this point all looks well and all parties involved opt for ortho-k, prepare a contract and go through it with the patient and parent before having them sign it. The contract should address all expectations and contingencies. Possible side effects need to be covered, and suitable alternatives addressed. Lastly, payment expectations should also be included. Always remember when structuring your fees for this procedure to allow an extra margin in your final fees to account for additional lenses or extra time needed to achieve the necessary precision. This is especially important for myopia control, where the initial lens selection may fail to deliver a satisfactory result.
 |
| The accumulation of ortho-k trial sets over the last 20 years. |
5. Check the Cornea
When performing ortho-k, it’s imperative to consider factors such corneal volume: the more volume you have the easier it is to move tissue, even with higher myopia. Be wary of small, flat corneas due to low volume, as they can test your fitting abilities, even in low prescriptions. Extremely flat corneas can also pose a challenge, especially in higher prescriptions. For example, 34.00D is about as flat as you can expect after ortho-k, so a 6D myope with a flat K of 39.00D may be out of reach. Remember, over 40 microns of elevation difference between steep and flat meridians usually means a toric alignment zone with its increased complexity.
Eccentricity of the cornea is extremely important to know to help you determine how much flattening to expect on the cornea as you move towards the periphery and whether a five curve or higher design is warranted due to that change. Familiarize yourself with your topographer’s intricacies and margins of error, as most will either over or understate the “e” value. When possible, also evaluate the “e” value with other methods such as a trial lens fitting. This is done by determining the best fluorescein pattern available underneath that trial lens. Ortho-k designs are accurate to perhaps 5μm, and the human eye can pick up a difference in patterns of roughly 10μm to 15μm, permitting an accurate assessment of corneal eccentricity and best-fit profile.
When taking topographies on children, take note that they tend to be more fearful and fidgety during examinations. If you are unable to acquire that “perfect” topography reading, it may be best to send the child home with eye drops to practice keeping their eyes open and inform the parents of the need for a precise topography. Have the child open their eyes wide as they instill the drops. Often on return visits, they are more relaxed, giving you a better opportunity to document their topography.
6. Be Ready for Fittings
The next step is fitting and ordering the lenses. The most popular methods for doing this are empirically, through trial lens fitting or custom design. Many ECPs forgo trial lenses and order an empirical or custom topographic design as “trial” lenses. In 80% of cases, they will work effectively and require minimal, if any, changes.7 Even though I have diagnostic data to help fit a patient, I often feel a trial fitting is much more accurate, as it provides additional information that helps me customize each fit. For instance, I can evaluate possible lid interactions such as overly tight lids.
When you are ready to trial fit, be sure to have the necessary time and space for ortho-k patients by providing a reclining chair so they can lay down with eyes closed for at least 15 minutes. This is much more valuable than open-eye assessment for lens fit and treatment. A mere 20 minutes of wear will often correct significant levels of myopia and astigmatism.
Many practitioners instill a drop of topical anesthetic before lens insertion to aid a young patient’s adaptation.
With many different trial set diameters at my disposal, I can nail covering 95% of corneal surface, which is necessary for best results.9
 |
| Clinicians should evaluate the orthokeratology fit at the slit lamp before dispensing. |
7. Dispense and Follow
When the lenses have arrived and passed inspection, bring the patient into the office and insert the lenses to make sure they fit well. If the patient and parent are satisfied, educate them on safe insertion, removal and care. If the patient is under eight years of age, it’s likely the parents will need to step in and provide support here, which may mean all of the insertion, removal and care. Allow enough time in your schedule for this process and, again, make sure this time is reflected in your fee structure.
Once you have dispensed the lenses, active follow up is necessary. In my practice, we see the patient the next day and then again in one month. Further follow-up visits are scheduled at three-month intervals. If it’s a higher amount of myopia or other factors such as high astigmatism are present, we ask patients to come in for follow-up appointments at two weeks as well. We also schedule the following year’s lens replacements and evaluations during the initial year.
I replace lenses for a child yearly because I personally believe that will provide the healthiest and safest outcomes, given children cannot legally take responsibility for their decisions, particularly when it comes to lens care.
8. Adjust Accordingly
Effective myopia control requires A-scans to determine axial length before and during treatment. You should take a new measurement every year. These readings, along with any changes in the over-refraction with ortho-k lenses at six and 12 months after initial fitting, will either confirm successful myopia control or lead to a new treatment strategy.
Modifications such as increasing the Jessen factor, using newer designs relying on six or more curves or using eccentricity in the base curve can lead to a greater elevation of the reverse curve and better myopic defocus in the periphery. The Jessen factor is the amount of lens flattening over and above the patient’s current prescription needs, which allows the eye to remain free from myopia, even after all-day wear. Research shows increasing the Jessen factor and reducing the treatment zone can create a better myopic image shell in the peripheral retina.10 Simply adding low-dose atropine (0.01%) in addition to ortho-k also may lead to better control without changing the lens.
Management decisions should be based on any changes in the axial length after the beginning of treatment. Even high myopia is within reach—although ortho-k may only get you part of the way there. Correcting at least 4D with corneal reshaping and then the rest with glasses can still reduce myopic progression by at least 50%.11
9. Don’t Stop Too Soon
A common mistake parents make is assuming that, once the riskiest years of myopic progression have passed, their child should switch from ortho-k to daily wear lenses or glasses. This is nearly always the wrong route to take, as many younger patients have no desire to limit their much-improved quality of life by making that switch. Further, in my experience, long-term wear of ortho-k lenses shows no signs of increased risk. I have many patients who have been wearing their ortho-k lenses for more than a decade with no signs of any adverse corneal changes. In fact, their corneas remain pristine even after years of overnight wear.
I consult with my long-term wearers at least once a year on their success with the procedure. When they are ready for LASIK or feel wearing the lenses nightly is impacting their lifestyle, I wash them out of their lenses. This process may take up to six months to accomplish in long-term wearers (>10 years).
10. Watch Your Patients and Practice Grow
Ortho-k can dominate a practice. My specialty practice is now about 80% corneal reshaping, which has translated into a healthy practice. Once you decide to incorporate ortho-k into your practice, be prepared for a younger patient base. At the same time, my younger corneal reshaping patients have proven extremely loyal, and I have a special opportunity to participate with parents in fostering their growth. While kids may be resistant to parental advice, they will often listen to an authority figure such as their ECP. Don’t waste that opportunity.
Taking a proactive role in the myopia epidemic and incorporating ortho-k into your practice can make a positive difference in your young patients’ lives. Controlling myopia progression at age six or seven by just 30% will eliminate 75% of all of high myopia (>5D) cases and the subsequent increased risk of ocular pathology.12 Further, evidence shows ortho-k is impactful on adolescents’ visual performance and binocular function.1 The improvement in quality of life afforded by ortho-k lenses is extremely rewarding to witness.
With myopia rates increasing, it’s time to fully consider all the options at our disposal. As far as I’m concerned, ortho-k is the way of the future. Don’t waste the opportunity to provide this amazing specialty to your pediatric patients. Taking the road less traveled can indeed make all the difference.
Dr. Herzberg has been practicing in Aurora, Ill., for 40 years—25 of which he has specialized in ortho-k. He is co-founder and president of the International Academy of Orthokeratology and Myopia Control and founder and co-president of the American Academy of Orthokeratology and myopia control. He serves as a consultant to the contact lens industry and lectures and writes on the topic of orthokeratology and myopia control around the world.
1. Eiden B. Lets not forget that most of us use two eyes together; Binocular vision implications in corneal reshaping treatment. CL Today Newsletter. December 11, 2016. Available at www.clspectrum.com/newsletters/contact-lenses-today/december-11,-2016. Accessed January 6, 2017.
2. Oh S. Statistical data in the field of orthokeratology and myopia control in the US and the world. Korean Contact Lens Study Society. Korean Ophthalmology Contact Lens Society. Nov 2016;9:79-85.
3. Nichols J. Contact lenses 2015. Contact Lens Spectrum. January 1, 2016. Available at www.clspectrum.com/issues/2016/january-2016/contact-lenses-2015. Accessed January 6, 2017.
4. Kojima R, Caroline P. IQ Scleral Lenses. Presented at Vision By Design 2014., April 24-27; Chicago, Ill.
5. Walline JJ, Rah MJ, Jones LA. The children’s overnight orthokeratology investigation (COOKI) pilot study. Optom Vis Sci. 2004 Jun;81(6):407-13.
6. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005 Jan;30(1):71-80.
7. Davis RL, Eiden SB, Bennett ES, et al. Stabilizing myopia by accelerated reshaping technique (SMART)-study three year outcomes and overview. Adv Ophthalmol Vis Syst. 2015;2(3):00046.
8. Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009 Sep;93(9):1181-5.
9. Global OK-Vision. GOV General Fitting Guide. Available at www.global-ok.com/html/GOVFittingGuide.html. Accessed January 12, 2017.
10. Chan B, Cho P, Mountford J. The validity of the Jessen formula in overnight orthokeratology: a retrospective study. Ophthalmic Physiol Opt. 2008;28(3):265-8.
11. Charm J, Cho P. High myopia–partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90(6):530-9.
12. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42.


