 |  |
Eye care professionals battle contact lens discomfort (CLD) management on a daily basis. According to one survey about discontinuation of contact lens wear, 45% of those surveyed dropped out of wear within the first year, and 47% cited discomfort as the primary reason for dropping out.1 Studies show that nearly 15% to 30% of contact lens wearers drop out each year.1-3 One of the most significant factors in CLD is dry eye, as approximately 50% of contact lens wearers report experiencing dry eye symptoms at least occasionally.4 This issue occurs with both soft and gas permeable lenses alike.
Due to its multifactorial nature, we have no cure-all for CLD, and even with today’s technological advancements, CLD remains a leading cause of dropout in contact lens wearers. Ultimately, if CLD is not diagnosed and managed early, a patient may drop out of contact lenses permanently.
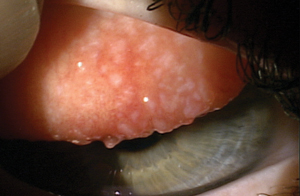 |
| Giant papillary conjunctivitis in a GP lens wearer. |
What is CLD?
According to the Tear Film and Ocular Surface Society (TFOS), CLD is “a condition characterized by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.”5 Clinically, CLD is usually determined by levels of end-of-day discomfort and dryness.5
TFOS further describes CLD as a distinctive five-step progression. It begins when patients start to struggle with symptoms such as physical awareness and visual disturbance. Consequently, patients reduce their comfortable wear time. As the lenses become more uncomfortable, patients begin reducing their total wear time. Next, patients may temporarily discontinue contact lens wear. For example, patients who used to wear contact lenses everyday for extended periods of time start to take breaks between wear. Finally, when comfort is no longer achievable, patients permanently discontinue lens wear. Given this progression, it is important to identify the factors that play a role in the earlier stages of discomfort to develop appropriate management strategies.
CLD Causes
For gas permeable (GP) lenses, clinicians should consider factors such as environmental allergies, poor contact lens fit, poor contact lens edge profile, contact lens solutions, surface deposits and poor surface wettability when deciding how to manage and treat discomfort. Sometimes, the underlying problem is unclear, and several treatments may be warranted to eliminate CLD. Here is a brief overview of some common causes of GP lens discomfort and treatment methods:
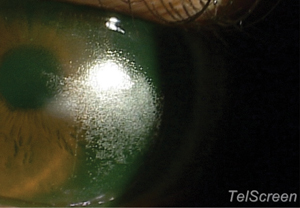 |
| Heavy lipid deposits on the scleral lens in an MGD patient. |
Environmental allergies. Giant papillary conjunctivitis (GPC) can occur with contact lens wear alone, but it can also be exacerbated with environmental allergies. If not treated, papillae can jeopardize success with contact lens wear. GPC can affect contact lens positioning due to lid interaction with the contact lens, creating a less-stable, high-riding contact lens.
When treating allergies in contact lens wearers, first consider switching to a preservative-free, peroxide-based lens solution or an alcohol-based cleaner to help minimize allergens on lens surface. Also, consider prescribing an antihistamine/mast cell stabilizer to be used on a daily basis. Preservative-free artificial tears should be applied every few hours to reduce exposure to allergens. Cold compresses can also be used to reduce symptoms. In severe cases, a topical steroid may be necessary to treat the condition. The severity level varies among patients, so several treatments may be necessary to eliminate CLD entirely.
Dry Eye. Researchers attribute dry eye symptoms in contact lens wearers to a diminished aqueous or mucin layer of the tear film, changes in tear protein concentration and altered meibomian gland structure or function, to name only a few.6 Studies show lens wear is associated with adverse changes in meibomian gland morphology as well as the condition of the lid margin and meibum.6 Contact lens-related dry eye may also be explained by increased tear film thinning, leading to greater tear evaporation and increased tear film osmolality.4 This suggests that contact lenses negatively affect meibomian glands and are partly responsible for dry eye symptoms.6
For patients with meibomian gland dysfunction (MGD), warm compresses and a more stringent eyelid hygiene regimen using a foam lid cleanser or hypochlorous acid are usually the first steps, along with omega supplements. A cycle of doxycycline or azithromycin may be used in more advanced cases of MGD due to their anti-inflammatory properties.7 Occasionally, an antibiotic eye drop, a low-dose topical steroid drop or an antibiotic-steroid combination drop may be used in conjunction with an inflammatory modulator such as Restasis (cyclosporine 0.05%, Allergan) or Xiidra (lifitegrast 5%, Shire). Punctal plugs may be used in patients where treatment with supplements, artificial tears or prescription eye drops fails to relieve dry eye symptoms. Deciding whether to use dissolvable collagen plugs or semi-permanent silicone plugs is left to the discretion of the eye care provider.
But when the patient still complains of discomfort after treatment with antibiotics, topicals, artificial tears/ointments and punctal plugs, a scleral contact lens may be the ideal solution.
Initially thought to be reserved for patients with irregular corneas or severe ocular surface disease, scleral lenses also can be a viable option for patients suffering from dry eye discomfort in their soft or corneal GP lenses. Scleral lenses can be more comfortable than soft lenses due to the fluid reservoir under the lens and the lack of lens surface dehydration.8 They are essentially moisture chambers on the eye that also give superior rigid lens optics.
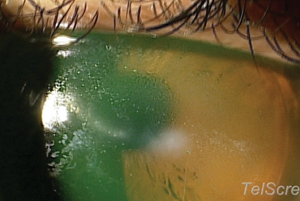 |
| More lipid deposits on the scleral lens surface in an MGD patient. |
Surface deposits and poor wettability. Often, a patient’s GP lens will fit well and feel comfortable, but poor surface wettability or heavy lipid deposits still occur. Excessive lipids in the tear film create a foggy, hydrophobic surface, which in turn leads to poor visual comfort. Alcohol-based cleaners or intensive protein cleaners such as Progent (Menicon) can help eliminate surface deposits. For patients who have had no success with various lens solutions, have been prescribed an eyelid hygiene regimen and have been warned not to use hand lotions prior to insertion of GP lenses, practitioners can consider a new lens coating to meet each patient’s needs.
According to Tangible Science, its new Hydra-PEG lens coating is designed to create a highly wettable and lubricious surface, with increased surface water retention due to its high water content (90%).9 This polyethylene glycol-based polymer can be permanently bonded to the surfaces of both soft and GP lenses, and is currently available for Contamac materials provided by several GP lens manufacturers. It also helps to reduce protein and lipid deposits on lens surface.9
CLD is both common and difficult to manage, in part because of its multifactorial nature. Without a tried-and-true treatment, it is important to consider a step-wise approach in diagnosing, managing and treating CLD to provide continued success with contact lens wear.5
1. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Intern Contact Lens Clinic. 1999;26:157-161.
2. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthal Physiol Opt. 2002;22:516-527.
3. Rumpakis J. New data on contact lens dropouts: an international perspective. Review of Optmetry. 2010;147(1):37-42.
4. Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. Apr 2006;47(4):1319-1328.
5. Nichols JJ, Willcox MD, Bron AJ, et al. The TFOS international workshop on contact cens discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54:TFOS7-TFOS13.
6. Arita R, Fukuoka S, Morishige N. Meibomian gland dysfunction and contact lens discomfort. Eye Contact Lens. Jan 2017;43(1):17-22.
7. Yoo SE, Lee DC, Chang MH. The effect of low-dose doxycycline therapy in chronic meibomian gland dysfunction. KJO. Dec 2005;19(4):258-263.
8. Jones L, May C, Nazar L, Simpson T. In vitro evaluation of the dehydration characteristics of silicone hydrogel and conventional hydrogel contact lens materials. Cont Lens Anterior Eye. Sep 2002;25(3):147-156.
9. Tangible Science. 2017. Available at: www.tangiblescience.com. Accessed March 31, 2017.


