A patient walks into the clinic desiring to try scleral lenses for the first time, or when evaluating a new patient you determine it’s the best approach and recommend this design. After some time spent with the diagnostic fitting set, you find the perfect lens for them. Congratulations! Now it’s time to teach the patient how to care for their lenses and send them on their way, right? Wrong! Fitting a patient with a scleral lens for the first time can be an exciting experience for both the practitioner and patient. However, even more than soft lens wearers, scleral lens patients require thorough training and practitioner follow-up care to ensure wearing success.
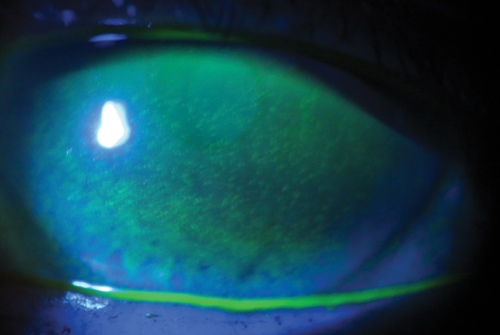 | |
Diffuse corneal staining due to a patient filling his scleral lens with a generic multipurpose solution containing preservatives instead of a preservative-free saline. |
Battle Plans
During the scleral lens dispensing visit, I first insert the patient’s lenses and allow them to settle on the ocular surface for 20 minutes before assessing vision and lens fit. The waiting time is essential to properly evaluate the fit of the lens after it has settled into the conjunctiva. Evaluating the lens too soon will yield inaccurate findings such as central clearance, edge alignment and overrefraction. I usually let the patient relax in the waiting room and see another patient while their lenses are settling.
If the fit is acceptable, the patient proceeds to their scleral lens training session. Scleral lenses are applied and removed differently than soft contacts and even corneal gas permeable lenses, so it is essential that all new wearers be provided with appropriate training. This can either be achieved through individual means or using online resources. For example, a free video on sclerallens.org reviews the basics of scleral lens care. All new scleral lens patients in my practice watch this video before their lens care lesson. In addition to providing training, this video also serves to further highlight the benefits of scleral lenses, helping to overcome any remaining reservations regarding wear.
At the contact lens lesson, the patient is shown tools and techniques for proper lens insertion and removal. Typically, they attempt lens removal first, as the lens is most often already in the eye. A mirror is first placed on the desk so the patient can view their eye and the surrounding periphery with a straight gaze. At this point, different scleral lens plungers can be used based on practitioner and patient preference: I prefer the non-vented small DMV plunger, for example.
When removing the lens for the first time, place a small drop of saline solution on the plunger and adhere the tool directly to the lens, making sure it is located towards the edge of the lens and not directly in the center. Once the plunger is firmly attached, twist and pull it at a tangential angle to remove the lens. A scleral lens that is fit properly will not be difficult to remove; however, if a large amount of suction occurs when attempting to remove the lens, the fit should be re-evaluated.
 | |
Scleral lens training can include informative videos, paperwork and brochures. | |
 | |
| Give patients a variety of methods to insert their scleral lenses to help maximize success. |
Be sure to inform patients that as they continue to wear their lenses more (i.e., for longer periods of time), they may become more challenging to remove due to the lens settling that occurs on the conjunctiva. This is to be expected, and should not result in any serious issues. Patients fit with small diameter scleral lenses may be able to remove the lens with their eyelids instead of the DMV plunger; however, only a few of my patients have had success with this method.
Once the patient has demonstrated adequate removal technique, it’s time to teach them proper lens insertion. I typically ask my patients to remove their lenses from the case and rinse them with nonpreserved saline. Then, they can place the lens on an insertion device, such as a large plunger, O-ring, EZI scleral lens inserter or tripod with fingers. The lens is then filled to the brim with nonpreserved saline and the mirror is placed on the table. Tucking their chin to their chest so their nose points to the floor, the patient should open the eyelids with one hand and place the lens directly onto the eye, then release their eyelids and, subsequently, the insertion device. Scleral lens insertion is typically more difficult than removal, so consider demonstrating a variety of insertion techniques to the patient.
Following lens removal education, lens care is reviewed. Scleral lenses can be cleaned with approved GP lens cleaners like multipurpose solutions; most of my scleral lens patients use a hydrogen peroxide system. Following the lens care lesson, patients are provide with a scleral lens “goodie bag” containing a sample of their selected care system, several insertion and removal devices, vials of nonpreserved saline and a prescription, written step-by-step care instructions and a scleral lens brochure (gpli.info provides up to 100 to practitioners for free). I ask them to trial their lenses for a week, record any issues and return for a follow-up appointment.
Following Up
Each practitioner has their own follow-up schedule that varies depending on patient condition, complexity of the case and experience level. For example, when I first began fitting scleral lens patients, I would ask them to return once a month for the first six months so I could evaluate both corneal health and lens fit. Now, however, I am more comfortable allowing longer intervals of time in between appointments, though if the patient has a more severe condition like Stevens-Johnson syndrome, I will ask them to return on a more regular basis to evaluate ocular health.
Be sure to ask your patients which lens care system they are using and what they are filling their lenses with at each follow-up appointment. Some patients try to cut corners by using regular multipurpose solution, neutralized hydrogen peroxide or even plain tap water to fill their lenses. Also, make sure to evaluate the lens fit at the beginning of the appointment, before it is removed for closer examination of the ocular surface. Examining the scleral lens on the eye is critical to identifying any wettability issues or evidence of scratches or deposits.
Additionally, assess central clearance, limbal clearance and edge alignment prior to lens removal. Conjunctival prolapse may also be visible during follow up appointments. Scheduling these visits later in the day can also help with gaining a true assessment of how the lens is interacting with the eye, as viewing the lens after it has been worn for several hours can leave room for identifying possible problems before the patient becomes symptomatic.
During all follow-up visits, we examine OCT images of central clearance and edge alignment, along with vision and slit lamp evaluation. One trick is to “paint” the front surface of the lens with sodium fluorescein, then evaluate it with a slit lamp to see if any of the chemical seeps underneath the lens edge. If you see sodium fluorescein in the tear chamber of the lens, you can assume there is adequate tear exchange throughout the day. No presence of the fluorescein may mean adjustments to the lens fit are necessary.
Additionally, when attempting to decide whether a toric peripheral curve may be needed, keep this in mind: as the lens settles throughout the day, it sits on the flat meridians of the sclera (mostly at 3 o’clock and 9 o’clock). When you see a patient after they have been wearing their scleral lenses for a few hours, you may notice blanching at the edges of the flatter meridian. The patient may also complain that their eyes become red or sore after wearing the lens for a few hours. Such a patient could benefit from a toric peripheral curve system.
Always remove the scleral lens during the follow-up appointments. The condition of the patient’s cornea and conjunctiva can give the practitioner valuable data about the success of the lens, but only if these areas are visible. For example, if staining is observed in one portion of the cornea, it is possible that the lens is touching in that area, but not in others. In this case, the fit will need to be adjusted to achieve proper vault.
If there is a ring of staining around the limbus, it’s likely that the lens is settling onto the limbus during the day; as such, the limbal curves of the lens will need to be altered. Steepening the limbal curves helps the lens vault over the mid-peripheral/limbal area to gain extra clearance. Some lens designs can alter the limbal area without affecting other areas of the lens fit, while others will need to alter the entire lens design when making a small change. Understanding how the lens works is critical because each manufacturer is different. If you observe diffuse superficial keratitis, there is a good chance that the patient is not rinsing their lenses prior to insertion, or is using a contraindicated filling solution. If any of these situations are observed, the practitioner must identify the necessary treatments and other relevant factors. A patient with glaucoma or a corneal transplant may need more frequent monitoring than a high astigmat, for example. As you fit more scleral lenses and see more patients for follow-up, you will likely develop your own rhythm.
Parting Words
Direct the patient to only use the prescribed products given to them during the scleral lens lesson. If they want to change products for any reason, it is imperative that they contact you to discuss these decisions, as use of an incorrect care system or filling solution can damage the eye, the lens or both. For example, preservative-free saline is the only liquid that should be used to fill the bowl of a scleral lens. Many patients may experience a strange feeling on the eye for the first few weeks of wear, especially if they are first-time wearers, as the ocular surface gets used to the new lens.
Drawing up a scleral lens contract with the patient is advisable before beginning the fitting and training process. Outlining all fees associated with the lenses can assist the patient with understanding what they are paying for. Be sure to include a clause stating what happens if the lenses do not work (i.e., do they receive any money back?) This is up to the practitioner to decide based on what they feel is fair. Also, review responses to other scenarios such as lens damage or loss.
Having a system in place for your scleral lens wearers can help with their success tremendously. Proper education prior to regular lens wear can save you from unnecessary phone calls or extraneous patient visits, and your patients from complications down the road. Additionally, investing time and energy into scleral lens education can help you further gain patient trust and respect, potentially leading to more referrals. Everyone loves to feel special, and helping patients feel cared for can create patient loyalty and a great relationship with their eye care practitioner.
Dr. Woo graduated with honors from the Southern California College of Optometry and completed a cornea and contact lens residency in St. Louis, Missouri. She is a fellow of the American Academy of Optometry and a fellow and treasurer of the Scleral Lens Society. She enjoys lecturing around the world on the topic of contact lenses and anterior segment diseases. Dr. Woo practices at Havasu Eye Center in Arizona.


