 |
Fitting scleral lenses is a fairly straightforward task: simply make sure the lens adequately vaults the cornea and limbal region to land on the bulbar conjunctiva. Achieving this, however, is sometimes more difficult in practice.
Most scleral lens designs consist of three primary zones: optical, transition and landing.1 The optical and transition zones provide sagittal depth to the lens for proper vault height, while the third zone—the landing zone—rests gently on the bulbar conjunctiva. This area is also commonly known as the haptics or peripheral curves. Proper alignment of this zone with the sclera is a critical component of a successful scleral lens fit, as any degree of misalignment can negatively impact both comfort and vision. As such, the incorporation of back surface toricity into the landing zone could improve the lens-to-sclera fitting relationship.
Understanding Scleral Shape
Research on the scleral shape of normal eyes has indicated most sclerae to be at least somewhat asymmetric or toric in nature. In the average patient, the nasal sclera is characterized by a flatter curvature, while the temporal sclera typically exhibits steeper curvature.1 The nasal quadrant is also higher in elevation compared with the temporal quadrant.2 This may explain why scleral lenses often decenter inferotemporally, though lid tension and gravity may also contribute.
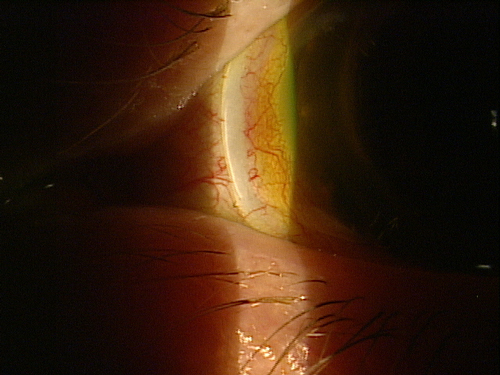 | |
Fig. 1. Tight peripheral curves can cause localized blanching. |
Common estimates suggest 25μm of corneal height differential is equivalent to approximately 1.0D of corneal toricity.3 Extending out to a 15.0mm chord, a similar study found the scleral height difference can range from approximately 50μm to more than 500μm.3 Though this study did not correlate scleral height difference to scleral toricity in diopters, other data suggests the average scleral toricity is approximately 4.0D.2
Improving Peripheral Fit
Recent technological innovations—including three-dimensional imaging and ocular surface impression molding—allow for more accurate empirical fitting. Despite these options, however, the majority of scleral lenses are still fit diagnostically. As such, placement of the diagnostic lens on the eye can be crucial in determining whether the addition of back surface toricity is beneficial.
Excessive compression of the bulbar conjunctiva via an ill-fitting lens can restrict blood flow, causing blanching of the conjunctival vasculature. A circumferential blanching pattern typically indicates the haptics are too steep, requiring modifications to the entire peripheral curve system to adjust the lens fit. Localized blanching in the absence of conjunctival anomalies like pingueculae can be attributed to scleral toricity. The incorporation of back surface toricity may help alleviate localized pressure by flattening the haptics in the flatter meridian.
When localized edge lift is an issue, steeper toric haptics may be a solution. Excessive edge lift can lead to bubbles and accumulation of debris underneath a lens, as well as increased lens awareness. If these characteristics are suspected but not readily apparent, instilling sodium fluorescein and watching for uptake underneath the lens while on the eye can reveal these issues.
 | |
| Fig. 2. Early conjunctival hypertrophy secondary to scleral lens impingement. | |
 | |
| Fig. 3. Instillation of fluorescein over the lens helps reveal mild edge lift in the superior quadrant. |
Back surface toric haptics are typically designed with rotationally stability in mind. Research has shown it takes approximately six seconds for back surface toric scleral lenses to return to their original position following manual on-eye rotation.4 As such, this stability allows for even distribution of weight across the bulbar conjunctiva, resulting in more comfort and a longer wearing time.4,5
What About Vision?
The fluid reservoir underneath a scleral lens neutralizes both normal and irregular corneal astigmatism. If a spherocylindrical overrefraction yields better vision, performing keratometry readings over the lens can be used to help identify any indication of internal astigmatism or lens flexure. Additionally, if the over-keratometry readings are astigmatic, the lens is either decentered or flexing on the eye.
Lens flexure commonly results from the torsional effect of the lens on a toric sclera; as such, the first step often taken to resolving this issue is to increase the center thickness of the lens.6 Though this may ultimately stiffen the lens, it also reduces oxygen transmission and increases the weight of the lens. The inclusion of back surface toric haptics may help reduce this torsional effect by improving lens alignment and centration. Furthermore, reducing the overall diameter may also lessen flexure, since the toricity of the sclera is higher at points further away from the limbus.7
In the case of internal astigmatism resulting from the posterior cornea or crystalline lens, front surface toric power can be added to the lens via double slab-off ballasting.1 Much like soft toric lenses, it is critical for front surface toric sclerals to be rotationally stable. If the lens does rotate, however, the LARS principle (i.e., left: add, right: subtract) that applies to soft lenses can be used to quantify scleral lenses as well. Back surface toric haptics can be used in conjunction with front surface toric power for additional stability and centration.
It’s clear that the growing popularity of scleral lenses is leading to the proliferation of new and better lens designs. Since recent research has indicated the sclera to be asymmetric, designs that incorporate toric haptics into their diagnostic sets may be increasingly valuable. Familiarizing yourself with both back surface toric haptics and front surface toric power will help improve your scleral lens fitting success.
1. van der Worp E. A Guide to Scleral Lens Fitting, Version 2.0 [monograph online]. Forest Grove, OR: Pacific University; 2015. Available from: commons.pacificu.edu/mono/10/.
2. Ritzmann M, Caroline P, Walker M, et al. Understanding scleral shape with the Eaglet Eye Surface Profiler. Scientific Poster presented at the Global Specialty Lens Symposium. Las Vegas. January 2015.
3. Kinoshita B, Morrison S, Caroline P, et al. Corneal toricity and scleral asymmetry…are they related? Scientific Poster presented at the Global Specialty Lens Symposium. Las Vegas. 2016.
4. Visser ES, Visser R, van Lier HJ. Advantages of toric scleral lenses. Optom Vis Sci 2006;83:233–236.
5. Visser ES, Visser R, van Lier HJ, Otten HM. Modern scleral lenses. Part II: patient satisfaction. Eye Contact Lens 2007;33:21Y5.
6. Michaud L. Beyond irregular: scleral lenses for everyday use. Contact Lens Spectrum. 2015. June; 30:30-32,34,36
7. Ritzmann M, Morrison S, Caroline P, et al. Scleral shape and asymmetry as measured by OCT in 78 normal eyes. Scientific Poster presented at the Global Specialty Lens Symposium. Las Vegas. January 2016.


