 |
Typically, patients with significant lenticular astigmatism are not the best candidates for non-toric rigid gas permeable lenses (RGPs).1 However, RGPs are often ideal for patients with keratoconus—leaving the clinician with some tough decisions when it comes to fitting contact lenses for patients with both conditions. A recent keratoconus patient with significant lenticular astigmatism highlights the challenges—and the rewards—of working through the problem with the patient and fellow clinicians.
The Case
A 69-year-old male with keratoconus presented with complaints that his glasses, fit four weeks prior, were not working for him. He said he felt a pulling sensation while wearing the glasses and his vision was blurry. He stated that he would like to avoid contact lenses due to past issues with insertion and removal.
His presenting prescription was -2.25 +6.75x001 OD and -0.25 +4.00x011 OS. Visual acuities (VAs) were 20/30- OD and 20/25+ OS. A manifest refraction of +0.75 +4.25x005 provided a VA of 20/20- OD, while -3.75 +8.00x003 gave him a VA of 20/25+ OS. The prescription was trial framed on the patient, and although his vision was clearer, he said the prescription gave him diplopia at both distance and near, making mobility difficult.
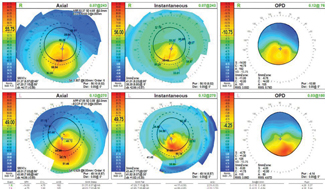 |
| Fig. 1. The patient’s corneal topography shows that the inferior central cones are steeper OD than OS. |
Slit lamp exam revealed 1+ inspissated meibomian glands and central corneal thinning OU, while the anterior chamber was deep and quiet OU. The iris was normal with 1+ nuclear sclerosis OU. Intraocular pressures were 12mm Hg OD and 11mm Hg OS. Topographical imaging revealed central corneal steepening of 51.37/47.2D OD and 48.01/43.95D OS (Figure 1).
After a long discussion of the corrective options, the patient decided to try contact lenses again, given the glasses provided no improvement.
Initial Fit
Due to the inferior broadness of the cone, I started the diagnostic fitting with large-diameter intralimbal RGPs. A 7.34 base curve (BC)/-6.00/11.2 diameter lens was placed on the patient’s right eye. Although the central fit was slightly flat and the peripheral edge had insufficient edge clearance, the lens exhibited good movement and centration. A spherical over-refraction of +1.50 caused monocular blur and vision of 20/50. Cylindrical over-refraction of -1.25 +2.75x078 provided a VA of 20/25 with no distortion.
For the left eye, I chose a 7.42/-6.00/11.2 lens. On eye, it exhibited light apical touch, an aligned peripheral edge, and was well centered with good movement. The over-refraction was +2.50 20/25-, and the patient complained of blur. The vision cleared with a plano +1.75x120 20/25 sphero-cylindrical over-refraction. The prescription was placed in trial frame over the contact lenses and the patient felt comfortable and his vision was clear. Autokeratometry was performed over the RGPs to determine if the lenses were flexing, which could also be a cause of residual astigmatism. No flexure was noted.
The right lens was slightly steepened to vault the cone, and the peripheral curves were widened and flattened. More minus power was added to compensate for the change in BC. The left lens parameters were kept the same as the diagnostic lens with the only change being the over-refraction. The following lens order was placed:
- OD: 7.11/-8.25/11.2; P1 0.4/9, P2 0.4/10.5, P3 0.4/10.5
- OS: 7.42/-6.00/11.2; P1 0.5/9, P2 0.5/11.75
A glasses prescription was also dispensed to be worn over the contact lenses to correct the residual astigmatism:
- OD: plano +2.75x075 (VA of 20/30)
- OS: plano +1.75x125 (VA of 20/25)
Week One
The patient presented for dispensing with no changes. He put the lenses on and reported immediate diplopia even with the spectacle correction. The patient was advised to wear the prescription for an hour a day to see if the diplopia would improve.
Week Two
The following week, the patient presented with complaints that he could not adjust to the new prescription, even after wearing the combination one hour a day. His vision was blurry without the glasses over the contacts, and the glasses gave him double vision. The patient was referred to his cornea specialist for a cataract consult, in the hopes that removing the right eye cataract would eliminate the lenticular astigmatism and the need for glasses to correct the residual astigmatism.
Post-procedure
The surgeon agreed with the plan and performed the operation one month later. The surgeon placed a spherical intraocular lens in the patient’s right eye. The patient presented two weeks after surgery to take measurements for a lens OD. A 7.34/-6.00/11.2 diagnostic lens was placed on the patient’s right eye. The over-refraction was +10.50 sphere, bringing the patient to 20/20.
The left eye corrected to 20/25- with a spherical over-refraction. The patient had slight double vision with this lens, but we decided to not prescribe glasses to correct the residual cylinder in his left eye because of his past intolerance.
The following lenses were ordered with the right lens adjusted slightly steeper to vault the cone:
- OD: 7.11/+4.50/11.2; P1 0.4/9, P2 0.4/10.5, P3 0.4/10.5
- OS: 7.42/-2.25/11.2; P1 0.5/9, P2 0.5/11.75
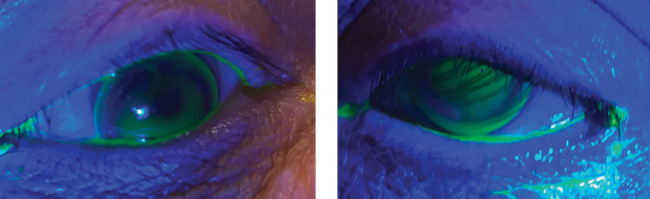 |
| Fig. 2. These images show the RGP lenses on the right and left eyes. You will note the good centration with light apical touch. |
Final Follow Up
The patient returned for his dispensing appointment, and once the lenses were inserted, he reported no binocular diplopia. Vision was 20/20 OD, 20/25- OS. The lenses exhibited light apical touch OU with good centration and movement. The patient was sent home to try the lenses with +2.50 readers.
He returned one week later with a positive report. His vision was slightly doubled in the left eye when he covered one eye, but he didn’t notice it when both eyes were open. He was quite happy with the final contact lens prescription and the vision it provided.
Discussion
Residual astigmatism is defined as the astigmatic refractive error still present after a lens is placed on the cornea.2-4 This can be very difficult to manage in patients with keratoconus. It often precludes patients from wearing RGPs; yet, soft lenses may not mask the irregular corneal astigmatism in patients with keratoconus. In this case, removing the lenticular astigmatism by way of lens replacement led to a successful outcome. If the residual astigmatism was still present after cataract surgery, the surgeon had plans to replace the cornea.
Finding the source of the residual astigmatism is the key to management. Autokeratometry or topography should be performed over the contact lenses to determine if the cylinder is induced by lens flexure. If the residual astigmatism is truly physiological, it can be corrected by spectacles or contact lenses that incorporate front surface astigmatism.
In addition, rotational stability is often a challenge when fitting RGPs. In cases where front surface toric RGPs and spectacles fail, cataract surgery can often address lenticular astigmatism, such as in this case.
1. Hom M, Bruce A. Keratoconus. A manual of contact lens prescribing and fitting. 3rd edition. Missouri; Butterworth-Heinemann; 2006:503-44. |


