We love our contact lenses. They improve our vision and looks while also helping us win on the athletic field. But we also hate our contact lenses, especially when they cause ocular irritation. Successful contact lens wear is multifactorial, and one of the leading factors is lens wettability. End-of-day discomfort and ocular dryness are the main causes of contact lens dropout, with up to one-third of contact lens wearers discontinuing wear secondary to these common complaints.1,2
The association of ocular dryness and contact lens discomfort has been frequently reported in the literature.1,3,4 As the most common complaint in contact lens wearers, dryness affects between 50% and 70% of wearers—most likely due to the physical interaction between the ocular surface (the tear film specifically) and the contact lens.5-7
Research shows a dysfunctional tear film is associated with complaints of ocular discomfort and dryness in contact lens patients, which in turn leads to reduced wear time, increased chair time and, ultimately, contact lens discontinuation. When these symptoms arise, often our first move is to immediately switch a patient’s contact lens modality or change contact lens solutions; however, addressing the ocular surface and unstable tear film first may improve contact lens retention and overall comfort. Let’s take a closer look at the tear film, how contact lenses affect it and how to keep our contact lens patients comfortable in their lenses.
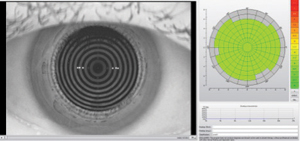 |
| This Oculus Keratograph 5M tear film quality color map demonstrates an overall even tear film centrally, with an average noninvasive tear break-up time of over 17 seconds. |
Keep the Tear Film Intact and Stable
Tear film stability and appropriate pre- and post-lens tear exchange characteristics are necessary for all contact lens wear, whether it is soft, gas permeable (GP) or specialty contact lenses.8 Factors that contribute to how well the tear film spreads over the contact lens surface include: surface tension gradients, the tear film-contact lens surface interface, tear film quality, tear film stability, gravity and the presence of deposits on the lens surface.9 Gradual surface deposition of proteins and lipids over time also contributes to decreased lens wettability and optical quality.
In particular, the stability of the tear film is related to the lipid layer’s ability to prevent evaporation from the ocular surface. A thicker lipid layer decreases evaporation rates and increases the period between blinks.10 For example, studies show patients with meibomian gland dysfunction have increased levels of cholesteryl esters (CE) and decreased levels of wax esters (WE) in their meibum, contributing to blocked glands and an unstable tear film.11 Another study looked at the effects of these tear lipid parameters in contact lens wearers and found a higher proportion of WE to CE lipids is associated with improved tear film quality and stability after eight hours of contact lens wear.12
In addition, corneal glycocalyx, which is formed by mucins secreted by epithelial cells, provides a hydrophilic barrier to minimize friction from blinking and stabilize the tear film in both contact lens wearers and non-wearers.13,14 However, contact lenses can also disrupt the corneal glycocalyx, as research shows hydrogel contact lenses gradually show a reduction in surface hydrophilicity over time, creating a hydrophobic surface.15 Hydrophobic contact lens surfaces cause more spontaneous dewetting and break up of the tear film compared with hydrophilic contact lens surfaces, further contributing to discomfort and dryness.
According to the Tear Film and Ocular Surface Society’s International Workshop on Contact Lens Discomfort, tear film stability is strongly associated with comfort and contact lens wear.16 Research shows contact lens wearers with reduced tear break-up times and tear volumes are more susceptible to lens-wear discomfort and, ultimately, contact lens intolerance.16,17
 |
| LipiView interferometry can provide objective measurement of lipid layer thickness, as well as real-time video of blink mechanics. Photo: Scott Hauswirth, OD |
Evaluate The Tear Film
According to research, contact lens wear disrupts the lipid layer, decreases the tear break-up time and increases tear evaporation and tear film thinning compared with patients who do not wear lenses.18-21 Thus, evaluating the tear film, its stability and how it interacts with the contact lens surface is essential to a contact lens practice.18-21
We should start by looking at contact lens surface wettability, which estimates the combined relationship of the soft contact lens surface dewetting and tear film spread.22,23 Other commonly assessed tear film measures include tear break-up time, noninvasive tear break-up time, tear film thickness and stability, tear meniscus height, Schirmer’s testing, phenol red thread testing, interferometry, on-eye contact angle, aberrometry, lipid layer interference patterns and optical coherence tomography.22
Although many clinicians use sodium fluorescein to measure tear break-up time, it is readily taken up within the matrix of the lens. Secondary to this, we can now use non-invasive measures of tear film break-up such as tear film reflection with placido disc images through corneal topography systems. New software systems, such as the Keratograph (Oculus) and the Tear Stability Analysis System (Tomey), can measure tear break-up time and quality, as well as tear film stability.
Another technique to assess tear film stability is interferometry, in which we can record the time between blinks and the first disruption in the lipid layer. For example, the LipiView (TearScience) system uses interferometry to measure the thickness of the lipid layer for half the tear film over the cornea at a time.
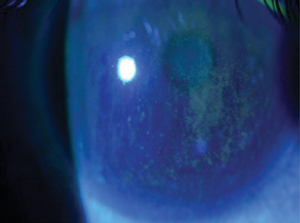
 |
| This image shows poor surface wetting of a contact lens due to unstable lipid layer and incomplete blink. |
Choose the Right Products
Once we have a clear picture of the patient’s ocular surface and the factors contributing to contact lens discomfort, we can treat any underlying etiologies such as dry eye disease or allergy to improve comfort. Only then can we turn to different contact lens modalities and materials to ensure the most comfortable lens wearing experience.
Care product solutions. The interaction of certain contact lens solutions with contact lens materials can play a significant role in ocular comfort and dryness.24,25 As such, recommending the proper solution to minimize negative adverse events such as toxicity and microbial keratitis is extremely important. We should also remember to educate patients who tend to accumulate deposits on their contact lenses about the importance of rubbing and rinsing their lenses or instruct them to use a peroxide-based solution system. Keep in mind that hydrogel lenses attract more proteins while silicone hydrogel lenses attract more lipids.26 A recommendation of more frequent lens replacement, which minimizes or even eliminates the need for solution, may also improve the patient’s overall ocular comfort in this situation.
Modalities. Replacing the lens more often is one way to combat contact lens discomfort and reduced wettability. Research shows contact lenses that are replaced more frequently, such as daily disposable lenses, enhance subjective comfort compared with those replaced less frequently.23,27
Materials. Concerning contact lens materials, the newer silicone hydrogel materials allow more oxygen to pass through the lens, which should improve tear film and ocular surface stability compared with hydrogel materials, as a higher Dk/t decreases central corneal swelling and maintains normal corneal homeostasis.28 Despite this, research has yet to show that silicone hydrogel lenses significantly improve ocular comfort or decrease incidence of microbial keratitis compared with hydrogel contact lenses.29
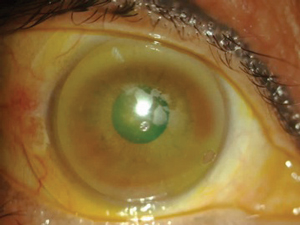
 |
| Clinical findings of poor tear film stability and corneal staining caused by severe dry eye and meibomian dysfunction. |
Manufacturers have attempted to address end-of-day discomfort and dryness in both soft and GP lenses by adding a moisture agent to the lens matrix or a coating to the lens surface. However, results have varied based on the lenses used and patients’ individual ocular surface characteristics. For example, patients who experience dryness or discomfort associated with lens wear or moderate-to-heavy lens deposition may benefit from the recently FDA-approved Tangible Hydra-PEG (Contamac), a 90% water polyethylene glycol-based polymer mixture that is permanently bonded to both surfaces of the contact lens. This may be applied to soft, GP, scleral and hybrid lenses.
Even when fitting patients in a silicone hydrogel lens, we have much to consider, as the lens material can differ significantly from one manufacturer to another. In one study, three different silicone hydrogel lenses were evaluated for clinical performance over the course of a 16-hour day.17 Results showed Dailies Total1 (delefilcon A, Alcon) lenses had a longer noninvasive tear break-up time than Clariti (falcon II-3, CooperVision) and 1-Day Acuvue TruEye (narafilcon A, Johnson & Johnson Vision) lenses. This may play a significant role in protecting the ocular surface for patients presenting with signs and symptoms of dry eye. Dailies Total1 lenses also demonstrated less corneal staining after 16 hours of wear than the other two lenses.17 All three lenses demonstrated similar comfort, vision, contrast visual acuity, quality of vision and limbal redness, although all of these factors decreased throughout the day.17 With all of the great lens options available, it is important to listen to patient feedback as well as look at the ocular surface to make the appropriate lens recommendation.
Evaluating and managing the tear film is not a new concept in clinical practice. However, improving the tear film will lead to increased contact lens wear time and retention, reduced chair time and increased referral network. We can always change a patient’s contact lens solution, their lens material or their lens modality. But above all else, consider the tear film and ocular surface wetting.
Dr. Harthan is an associate professor at the Illinois College of Optometry and chief of the Cornea Center for Clinical Excellence at the Illinois Eye Institute. She lectures, publishes and participates in research on OSD and contact lenses.
Dr. Hom practices in Southern California. He is an award-winning, internationally recognized expert and lecturer in dry eye, contact lenses and allergy. He has written four books and published over 200 papers and peer-reviewed abstracts.
1. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999;26:157-62.
2. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26:168-74.
3. Begley CG, Caffery B, Nichols KK, Chalmers R. Responses of contact lens wearers to a dry eye survey. Optom Vis Sci. 2000;77:40-6.
4. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39:92-8.
5. Dumbleton K, Caffery B, Dogru M, et al. The TFOS international workshop on contact lens discomfort: report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013;54:TFOS20-36.
6. Begley CG, Chalmers RL, Mitchell GL, et al. Characterization of ocular surface symptoms from optometric practices in North America. Cornea. 2001;20:610-8.
7. Stapleton F, Marfurt C, Golebiowski B, et al. The TFOS international workshop on contact lens discomfort: report of the subcommittee on neurobiology. Invest Ophthalmol Vis Sci. 2013;54:TFOS71-97.
8. Stapleton F, Stretton S, Papas E, et al. Silicone hydrogel contact lenses and the ocular surface. Ocul Surf. 2006;4:24-43.
9. Varikooty J, Keir N, Simpson T. Estimating tear film spread and stability through tear hydrodynamics. Optom Vis Sci. 2012;89(8):E1119-24.
10. Craig JP, Tomlinson A. Importance of the lipid layer in human tear film stability and evaporation. Optom Vis Sci. 1997;74:8-13.
11. Bowman RW, Dougherty JM, McCulley JP. Chronic blepharitis and dry eyes. Int Ophthalmol Clin. 1987;27:27-35.
12. Rohit A, Willcox MDP, Brown SHJ, et al. Clinical and biochemical tear lipid parameters in contact lens wearers. Optom Vis Sci. 2014;91:1384-90.
13. Ablamawoicz AF, Nichols JJ. Ocular surface membrane-associated mucins. Ocul Surf. 2016;14:331-41.
14. Markoulli M, Kolanu S. Contact lens wear and dry eye: challenges and solutions. Clinical Optom. 2017;9:41-8.
15. Shirafkan A, Woodward EG, Port MJ, Hull CC. Surface wettability and hydrophilicity of soft contact lens materials, before and after wear. Ophthalmic Physiol Opt. 1995;15:529-32.
16. Craig JP, Willcox MDP, Argueso P, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS123-56.
17. Wolffsohn JS, Mroczkowska S, Hunt OA, et al. Crossover evaluation of silicone hydrogel daily disposable contact lenses. Optom Vis Sci. 2015;92:1063-8.
18. Young G, Efron N. Characteristics of the pre-lens tear film during hydrogel contact lens wear. Ophthalmic Physiol Opt. 1991;11:53-8.
19. Guillon MG, Guillon JP. Hydrogel lens wettability during overnight wear. Ophthalmic Physiol Opt. 1989;9:355-9.
20. Nichols JJ, Mitchell GL, King-Smith PE. Thinning rate of the precorneal and prelens tear film. Invest Ophthalmol Vis Sci. 2005;46:2353-61.
21. Guillon M, Dumbleton KA, Theodoratos P, et al. Association between contact lens discomfort and pre-lens tear film kinetics. Optom Vis Sci. 2016;93:881-91.
22. Haddad M, Morgan PB, Kelly JM. A novel on-eye wettability analyzer for soft contact lenses. Optom Vis Sci. 2011;88:1188-95.
23. Guillon M, Maissa C. Use of silicone hydrogel material for daily wear. Cont Lens Anterior Eye. 2007;30:5-10.
24. Willcox MD, Phillips B, Ozkan J, et al. Interactions of lens care with silicone hydrogel lenses and effect on comfort. Optom Vis Sci. 2010;87:839-46.
25. Campbell R, Kame G, Leach N, et al. Clinical benefits of a new multipurpose disinfecting solution in silicone hydrogel and soft contact lens users. Eye Contact Lens. 2012;38:93-101.
26. Pucker AD, Nichols JJ. Impact of a rinse step on protein removal from silicone hydrogel contact lenses. Optom Vis Sci. 2009;86:943-7.
27. Poggio EC, Abelson M. Complications and symptoms in disposable extended wear lenses compared with conventional soft daily wear and soft extended wear lenses. CLAO J. 1993;19:31-9.
28. Papas EB. The significance of oxygen during contact lens wear. Cont Lens Anterior Eye. 2014;37:394-404.
29. Santodomingo-Rubido J, Barrado-Navascues E, Rubido-Crespo MJ. Ocular surface comfort during the day assessed by instant reporting in different types of contact and non-contact lens wearers. Eye Contact Lens. 2010;36:96-100.


