Steroids have traditionally carried the stigma of potential serious side effects outweighing their benefits more so than any other class of drugs. Optometric and medical education had previously emphasized the negative consequences of steroid use, making many practitioners hesitant to use them unless the situation is dire.
In reality, the anti-inflammatory effects of steroids far outweigh their possible side effects—in fact, some experts believe withholding steroids has caused more harm to patients overall than their occasional consequences. Research has also supported using them earlier and more often, as we now have a better understanding of potential side effects and more drug options tailored to treat specific conditions.
From the eye care professional’s perspective, prevention of vision loss, earlier return to contact lens wear and a reduction in the amount of work or school days missed are all practical benefits to using topical steroids.
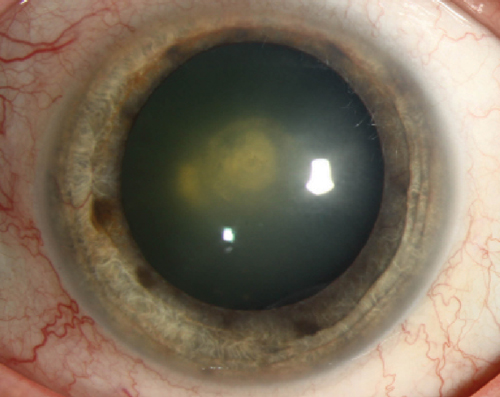 | |
| Fig. 1. Topical steroid use is typically more closely associated with causing an increase in IOP than a posterior subcapsular cataract, shown here. Photo: Christine W. Sindt, OD |
Understanding and Managing Side Effects
Inflammation is the body’s response to a stimulus (e.g., invasive organism) it perceives as offensive. While an effective defense mechanism, the inflammatory process can cause scarring and damage to healthy tissues that surround the infected area. Steroids work by blocking phospholipase A2, thereby blocking both arms of the chemical inflammatory cascade.1 Thus, they not only decrease vasopermeability and reduce edema and redness, they have the added benefit over nonsteroidal anti-inflammatory agents of keeping polymorphonucleocytes, leukotrienes and other blood cells sequestered from the site of inflammation, thereby reducing collateral damage to surrounding healthy tissue.2 However, while efficacious and unique in quelling the deleterious effects of inflammation, they are not without consequences.
The two common ocular side effects associated with steroid use are increased intraocular pressure (IOP) and cataract formation. Topical steroids are generally more associated with an increase in IOP than causing the classic steroid-induced posterior subcapsular cataract (Figure 1); in fact, risk of cataract formation from short-term topical steroid use is considered small. Cataract formation is instead more commonly associated with prolonged use of oral steroids, though advances in modern cataract surgery techniques have made this less of a concern than it was decades ago.
The prevalence of steroid-associated IOP increase ranges between 5% and 33% of the general population depending on the study cited and the definition used.4 Generally, topical steroids can be used for two weeks with minimal effect on IOP.5 After two weeks, IOP can unpredictably rise with no discernable correlation regarding amount or time frame. Thus, the goal of acute topical steroid use is to aggressively eliminate inflammation within the two-week period and then discontinue the drug. If IOP spikes with short-term steroid use, pressure generally returns to baseline two to four weeks after the drug is discontinued.6 With chronic use, the steroid response can occur months to even years later, so patients on long-term steroid therapy—even just one drop per day—should have their IOP checked every three months until the drug is discontinued.
Should IOP increase to the point that treatment is required, glaucoma drugs can treat the problem. Note, healthy discs can tolerate IOP in the high twenties to low thirties for a few weeks without significant compromise. Steroid-induced glaucoma is attributable to increased resistance to outflow at the trabecular meshwork, possibly due to an accumulation of glycosaminoglycans and other substances in this area.7 This decrease in aqueous outflow means that drugs that reduce aqueous production make sense for treating steroid-induced glaucoma.8
Topical beta-blockers such as timolol, levobunolol and metipranolol have long been used to blunt a steroid-associated increase. Topical carbonic anhydrase inhibitors such as Trusopt (dorzolamide 2%, Merck) and Azopt (brinzolamide 1%, Alcon) have been demonstrated to decrease aqueous production and so work well for treating steroid-induced glaucoma. Alpha agonists such as Alphagan P (brimonidine 1%, Allergan) also decrease aqueous production while simultaneously increasing uveoscleral outflow.
Additionally, combination drugs such as Combigan (brimonidine 0.2% and timolol 0.5%, Allergan) and Simbrinza (brinzolamide 1% and brimonidine 0.2%, Alcon) work well for steroid-induced glaucoma and provide the convenience of less drop instillation. Prostaglandins are also known to lower IOP in steroid-induced glaucoma by increasing uveoscleral outflow; however, they also carry a small possibility of increasing ocular inflammation.9
 | |
| Fig. 2. Topical steroids may increase risk of infection due to their suppression of the ocular immune system, but can be safely combined with antibiotics. Photo: Christine W. Sindt, OD |
Another concern regarding topical steroids is that their suppression of the ocular immune system may increase risk of infection (Figure 2). Topical antibiotics have improved tremendously as well over the years. Topical fourth-generation fluoroquinolones like Zymaxid (gatifloxacin 0.5%, Allergan) Moxeza (moxifloxacin 0.5%, Alcon) and Besivance (besifloxacin 0.6%, Bausch + Lomb) are well-equipped to provide broad-spectrum coverage against many kinds of bacteria and should be used concurrently with steroids for prophylaxis if potential infection is a concern.
Picking the Right Drug
As a result of recent research, we practitioners now have more drug options available to us than ever before. Prednisolone acetate 1% (Pred Forte, Allergan; Econopred, Alcon) remains the gold standard to which all other topical steroid preparations are compared. It is a good a choice for moderate to severe inflammation and it continues to be used postoperatively in many ocular surgical procedures.
So-called soft steroids offer an extra margin of safety for long-term topical steroid use or for patients with a known risk of steroid response. A “soft” drug is a biologically active compound with a predictable inactivation to a nontoxic substance after achieving its therapeutic role.10 Lotemax (loteprednol 0.5%, Bausch + Lomb) is structurally similar to prednisolone but rapidly undergoes hydrolysis in the anterior chamber to an inactive derivative. While its efficacy may be a little less than prednisolone acetate 1%, it is less likely to increase IOP.11
A weaker version of loteprednol in a 0.2% formulation (Alrex, Bausch + Lomb) is available for treating seasonal allergic conjunctivitis. Vexol (rimexolone 1%, Alcon) is another soft steroid with efficacy approaching prednisolone acetate 1% but with a lower steroid response rate.12 It has a higher steroid receptor binding affinity and is rapidly degraded to inactive metabolites.
If out-of-pocket cost to the patient is a concern, note that many fluorometholone-based steroids are now available generically. These agents also have reduced steroid-induced IOP elevation response. Fluorometholone alcohol 0.1% (FML, Allergan) is effective for mild ocular surface inflammation, while fluorometholone acetate 0.1% (Flarex, Alcon) has better ocular penetration and is appropriate for moderate inflammation.5
Durezol (difluprednate 0.05%, Alcon) is currently the most potent steroid available.13 Originally developed in Japan as a dermatologic preparation, it has been reformulated as an ophthalmic emulsion. The molecule is specially designed to offer both better penetration and higher anti-inflammatory activity, giving it the same anti-inflammatory ability as prednisolone acetate 1% at half the dosing. With its tremendous anti-inflammatory properties, however, have come some reports of significant IOP response.14
Steroids and Ocular Conditions
Topical steroids aren’t just for uveitis any more. The development of safer drugs with new formulations has led to a reevaluation of the appropriateness of a steroid for many ocular conditions where they were once contraindicated. For example, steroids are now considered appropriate to alleviate symptoms of dry eye on a short-term basis, and are commonly used as immediate discomfort relief while waiting for longer-term treatments like Restasis (cyclosporine ophthalmic emulsion, Allergan), punctal plugs and advanced lubricants to work.15
Topical steroids can also be used in cases when a patient’s symptoms may be temporarily exacerbated. A soft steroid with a lower incidence of steroid response such as Lotemax gel BID to QID (depending on severity) can be used to reduce symptoms during the initial one-month startup of Restasis, or BID to QID for a week or two if symptoms particularly flare up.
Steroids are also considered beneficial when treating conditions that involve lid inflammation, such as posterior blepharitis. This is because while topical antibiotics help reduce associated bacteria, the patient typically does not feel improvement until lid inflammation is controlled.16 Zylet (Bausch + Lomb), which combines the antibiotic tobramycin with loteprednol, is a good choice for this condition. Tobradex ST (Alcon), which combines tobramycin and dexamethasone with xanthum gum, is another good choice because this unique formulation leads to longer surface contact time between the medication and the lids.
Once considered an absolute contraindication, topical steroids have now also been studied in the treatment of corneal ulcers. The Steroids for Corneal Ulcer Trial (SCUT) randomized patients to receive prednisolone sodium phosphate 1% or placebo in addition to moxifloxacin.17 The primary endpoint measured was best spectacle-corrected visual acuity at three months after enrollment. Results at this time indicated that while the steroid had no significant effect on overall acuity outcome, there was no apparent increased risk of corneal perforation and no major safety concerns were identified. Further analysis of their subgroups revealed a slight improvement in visual acuity outcome for large central ulcers with steroid treatment, and led to the recommendation that steroids should be avoided for Nocardia, Mycobacterium and fungal infection.
Interestingly, additional data collected at 12 months demonstrated further reduction in scar density in a small number of patients enrolled in SCUT. This continued corneal remodeling was accompanied by an improvement in visual acuity, suggesting steroid use earlier in the course of the bacterial ulcer may in fact contribute to eventual improvement in corneal opacity.18
Pearls for Use
We practitioners are fortunate to have so many topical steroids available now. So, don’t rely on one “go-to” drug for all presenting conditions. Pick your drug based on the amount of inflammation you’re treating: mild, moderate or severe. Mild surface inflammation is easily treated with less penetrating drugs such as Alrex or FML, which typically help avoid the steroid response. Moderate inflammation is handled well with Lotemax or Vexol, while Pred Forte or Durezol should be reserved as treatment for severe inflammation. Many generic topical steroids are also now available for patients with financial concerns.
Next, be sure to consider the potential for steroid response. For a treatment period of two weeks or less, the risk of complications is considered minimal for most available drugs. If treating long term, however, consider using drugs with a reduced steroid response, such as Lotemax, Alrex, Vexol or fluorometholone alcohol or acetate.
If IOP rises during a course of steroid therapy, again bear in mind that otherwise unaffected optic discs can withstand IOP in the high 20s or low 30s for a few weeks without significant damage to structure or function. If IOP does become a concern, however, first consider discontinuing the steroid if possible. In cases where inflammation is still present, substituting a soft steroid can help. If the patient's IOP level remains unacceptable, add concurrent glaucoma medications as needed until the steroid is discontinued. Remember, IOP usually returns to baseline two to four weeks after the steroid is discontinued for short-term therapy.
With a contemporary knowledge of our topical steroids, there is no reason to hold back on their use. Our newer formulations are safer, and recent studies have made their side effects more predictable and manageable. Research also supports using them earlier and more often in many ocular conditions. Your patients will thank you.
Dr. Cakanac is a partner in a group optometric practice and clinical staff of a tertiary care ophthalmology practice, both in Pittsburgh, Pennsylvania. He is also a member of the editorial review board for Review of Optometry.
1. Jaanus S and Lesher G. Anti-Inflammatory Drugs. In: Bartlett J and Jaanus S (eds) Clinical Ocular Pharmacology. Boston: Butterworth Heinemann 1995: 308-18.
2. Skorin L. Uses and effects of ocular steroids. Review of Optometry 2002 May:139(5) 85-92.
3. Renfro L, Snow J. Ocular effects of topical and systemic steroids. Dermatol Clin 1992 Jul;10(3):505-12.
4. Sihota R et al. Long-term evaluation of steroid-induced glaucoma due to systemic and ocular steroids. Las Vegas: AAO APO joint meeting 2006: Nov 11-14.
5. Leibowitz H, Kupperman A. Uses of corticosteroids in the treatment of corneal inflammation. In: Leibowitz H (ed) Corneal disorders: clinical diagnosis and management. Philadelphia: WB Saunders 1984; 286-307.
6. Tripathi R et al. Corticosteroids and glaucoma risk. Drugs and Aging 1999, 15(6) 439-50.
7. Sherwood M and Richardson T. Evidence for in vivo phagocytosis by trabecular endothelial cells. Invest Ophthalmol 1958: 59,216.
8. Sowka J and Kabat A. A potent new steroid. Review of Optometry website. 2010: July 15.
9. Scherer Wand Hauber F. Effect of latanoprost on intraoculoar pressure in steroid-induced glaucoma. J Glaucoma 2000 Apr,9(2):179-82.
10. Howes J. Development of soft drugs for ophthalmic use. In: Ocular therapeutic and drug delivery: a multidisciplinary approach. Lancaster: Technomic Publishing, 1996 Aug 122(2):171-82.
11. Whitcup S and Ferris F, Hew corticosteroids for the treatment of ocular inflammation. Am J Ophthalmol 1999 May:127(5) 597-5.
12. Foster S. Topical steroid treatment of ocular inflammation. In: Advances in ocular pharmacology. Ophthalmology Clinics of North America 1997 Sept: 10(3) 389-403.
13. Ngoei E. What’s ahead: controlling inflammation. Eyeworld website 2015: March 11.
14. Birnbaum A et al. Elevation of Intraocular Pressure in Patients with Uveitis Treated With Topical Difluprednate. JAMA Ophthalmology website 2011: May 9.
15. Bowing E and Russell G. Topical steroids and the treatment of dry eye. Review of Cornea and Contact Lens website 2011: Mar 17.
16. Jackson W and Bruce M, “Management of Dysfunctional Tear Syndrome: A Canadian Consensus.” Canadian Journal of Ophthalmology 2009 44(4) 386.
17. Srinivasan M et al. Corticosteroids for bacterial keratitis: the steroids for corneal ulcers trial (SCUT). Arch Ophthalmol 2012 Feb; 130(2) 143-50.
18. McClintic SM, Srinivasan M, Mascarenhas J, et al. Improvement in corneal scarring following bacterial keratitis. Eye (Lond). 2013 Mar;27(3):443-6.


