Scleral lenses have opened up a new realm of possibilities to provide patients with improved vision correction and relief for dryness, so it’s no surprise practitioner interest is booming.1 Likewise, interest in gas permeable (GP) lenses is burgeoning, as contact lens experts are looking to expand their repertoires.1
As a result of the scleral and GP lens explosion, technology has evolved to improve specialty lens fitting. For practitioners looking to get started with scleral and GP lenses, it is especially important to know what options are out there. Here is a review of today’s scleral and GP lens fitting technology and how it can make a difference in your practice.
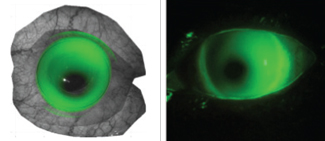
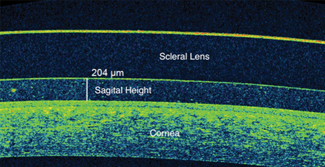 |
| Fig. 1. Corneal vault and limbal clearance can help practitioners ensure that the lens isn’t touching the cornea and an adequate end of vault remains after the lens has settled. |
OCT Imaging
When it comes time to fit and assess lenses, optical coherence topography (OCT) can be a powerful tool. To achieve a proper fit, scleral lenses must vault the entire cornea and limbus region. As such, accurate corneal diameter is imperative to determine the correct size of the lens. Using an OCT, practitioners can see this and the vault of a lens relative to the cornea to help ensure there is no touch and an adequate vault remains after the lens has settled. The limbal clearance zone can also be evaluated for adequate lift (Figure 1).
The desired sagittal height of a scleral lens can also be measured using anterior segment OCT. For a 15mm diameter scleral lens, the desired sagittal height is calculated by measuring the sagittal height of the cornea at the 10mm chord and adding 2,350μm (2,000μm for the average height of cornea from the 10mm to 15mm chord and 350μm of desired tear film vault above the cornea) (Figure 2).2 For each 1mm increase in size of the scleral lens, practitioners should add 150μm.2
Another important OCT imaging capability is assessment of the edge profile of a scleral lens. A flat edge that creates lift or a steep edge that digs into the sclera can cause many problems for the wearer. A flat lens edge can create discomfort, lid awareness, fogging and debris build up under the lens, while a steep edge can cause compression, blanching of vessels, redness and discomfort. With quadrant-specific designs, practitioners can evaluate the lens edge design and make changes with toric peripheral curves as needed (Figure 3).
Corneal Topographers
While OCT imaging is an effective tool in its own right, corneal topographers also have some tricks up their sleeves. For one, many corneal topographers have a built-in contact lens module that allows practitioners to design GP lenses or scleral lenses, thus reducing chair time with fitting sets.
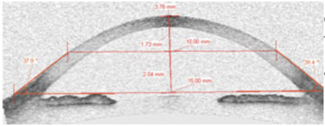 |
| Fig. 2. The desired sagittal height of a scleral lens can be measured using an OCT, shown here, or a corneal topographer. Image: Randy Kojima, OD |
The sMap3D (Visionary Optics) is one corneal topographer that stitches together a series of three images—up gaze, straight gaze and down gaze—to create a scleral elevation map and provide a complete picture of the cornea and sclera. It is designed with two cameras and one light source to give three independent triangulations over a 22mm field of view, including the superior sclera and inferior sclera. It is also the only topographer that provides a 360° view of the scleral shape.2
Before imaging with the sMap3D, practitioners should instill fluorescein into the patient’s eye and lift the top lid while the patient pulls down the lower lid. This will provide the widest view of the cornea, sclera and limbus without any obstruction.2
After topographic evaluation, the practitioner can place a diagnostic lens on the eye to get an accurate over-refraction. Practitioners send this information, along with the maps, to the company to have it custom design a lens for that eye. The practitioner also has the option to change any parameter to alter the design of the lens and see how it will fit on the eye. The sMap3D’s accompanying software is designed to allow for virtual fitting to demonstrate how the custom-designed lens fits on the stitched 3D maps of the cornea and sclera. Practitioners can also see a sodium fluorescein pattern simulation, and any parameter can be adjusted to provide the best fit prior to ordering.
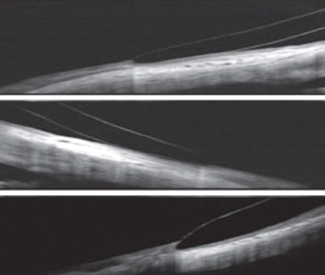 |
| Fig. 3. Here are some OCT image examples. At top, good edge alignment. In the middle, a flat edge lifting off of the conjunctiva. At bottom, a steep edge digging into the conjunctiva. Photos: Jason Jedlika, OD |
In the past, scleral toricity has been difficult to measure when fitting lenses. With the sMap3D topographer, however, practitioners can figure out the requirements for toric peripheral curves, as well as how to reduce the amount of toricity, edge design complications and flexure stemming from a spherical lens put on a toric sclera.
The sMap3D’s current limitation is that it cannot be used with all scleral lens designs. At the moment, it is designed for the Europa and the Elara scleral lens designs (Visionary Optics). The company plans to add other designs by the end of the year, however.
Using profilometry technology—a non-contact 3D shape measuring technique—the Eye Surface Profiler (Eaglet-Eye) projects a fringe pattern onto a diffuse target surface and the resulting deformed fringe pattern is captured by a digital camera to be processed into an image. Prior to image capture, two light sources project moiré patterns onto fluorescein in the patient’s eye. Through this process, the Eye Surface Profiler measures more than 350,000 data points over a 20mm diameter of the eye, providing 3D anterior segment height maps of the surface.3 One of its key features is eye asymmetry imaging, allowing practitioners to accurately fit both scleral and GP lenses. Based on the 3D map of the eye and the back-surface designs of particular lenses, the software algorithms will suggest five custom-fit sizes of contact lenses. This reduces chairtime and increases patient comfort.
In the past, scleral toricity has been difficult to measure when fitting lenses. With scleral topographers, however, practitioners can figure out the requirements for toric peripheral curves, the amount of toricity, edge design complications and flexure stemming from a spherical lens.
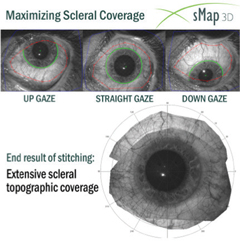 |
| Fig. 4. The sMap3D stitches together up gaze, straight gaze and down gaze images to create a scleral elevation map. Photos: Visionary Optics |
Software for Computer-designed Lenses
Practitioners who prefer to use their own topographers still have options to create detailed scleral and GP lens designs. Here are some software programs currently on the market:
EyeSpace and Scleral EyeSpace (Innovatus Technology) are desktop software platforms created to help practitioners design scleral and GP lenses with their own topographers and fitting sets. The company’s goal is to improve the success rate of the first lens ordered through education about lens parameters and how changing them impacts the fitting relationship of many GP lens designs.
Both programs are compatible with the E300 (Medmont) and Keratograph (Oculus) topographers, and others can be adapted for compatibility upon request. To choose an initial trial lens, practitioners can import data from their topographers into the software, which then guides them through the process. Once all the data has been entered and the software has made its calculations, there is an override option if the presented calculations are not ideal. EyeSpace and Scleral EyeSpace also give practitioners the ability to simulate the created lens on the eye. When practitioners are satisfied, they can order the final lens directly through the software.
Wave and OrthoTool are third-party software programs that provide a GP and scleral lens construction module similar to that of EyeSpace and Scleral EyeSpace. Practitioners can import data from topographers to design custom lenses for their patients.
Corneal-Scleral Prosthetic Molds
For practitioners who prefer to forego imaging, corneal-scleral prosthetic molds can provide a precise fitting experience.
The EyePrintPro (Eyeprint Prosthetics) is a scleral lens shell made from an impression mold of the eye. The impression process allows practitioners to capture the precise curvatures of the ocular surface within one to two microns of accuracy.4 The EyePrintPro is customizable in areas such as spherical and toric optics, unlimited add powers, prism in any direction to reduce diplopia, decentered optics, and rotationally stable optics.4
 |
| Fig. 5. At right, an actual fluorescein pattern through the slit lamp compared to a simulated image from the sMapPro software, at left. Photos: Visionary Optics |
The EyePrintPro is designed to allow practitioners to make lenses into front or back surface multifocal designs with exact visual axis specification to provide ideal multifocal vision for irregular corneas. To adjust for nighttime reduced distance vision associated with enlarged pupils, practitioners can place a peripheral distance correction on the front surface.4
In 1994, the BostonSight Prose (Boston Foundation of Sight) received FDA approval for corneal disorder treatment.5 The lens has a diameter ranging from 15mm to 23mm, a 12mm central optic zone and a 2mm wide transitional zone that vaults the limbus. Its haptic zone has channels that allow for tear exchange at the scleral interface.5
When fitting the BostonSight Prose, practitioners use computer software to create a front and back surface design of second–order continuity.
In 2017, the Boston Foundation of Sight launched a new lens fitting system, the BostonSight Scleral. This 22-lens system was designed based on six years of clinical and scleral anatomy data from approximately 7,000 eyes.6 It is the first scleral lens to provide right and left specific eye designs, as well as the first to have a front surface eccentricity option to improve vision to a higher order.6Other options for this lens system include quadrant-specific toric peripheral curves, front surface toric optics and three different diameters: 18mm, 18.5mm and 19mm. A web-based fitting and online ordering system are also available.6
 |
| Fig. 6. Here is a look at the EyePrintPro’s impression mold system in action. |
GP Lens Coating
After going through the process of designing and fitting the best lens for a patient, the last thing a practitioner wants to deal with is material that wets poorly, deposits quickly or creates irritation. However, appropriate materials, coatings and solutions should always be a focus of the custom lens process for a successful fit.
For years, discomfort has been the number one reason for contact lens discontinuation.7 However, preventing discomfort recently got easier. Hydra-PEG (Tangible Science), a polyethylene glycol-based polymer mixture coating that can be applied to hydrogel, silicone hydrogel, GP and hybrid lenses, has effectively improved wettability, lens surface water retention, lubricity, tear break-up time, patient comfort and overall wear time while minimizing friction, protein and lipid deposition, lens fogging and lens irritation.6,8
Hydra-PEG is compatible with most multipurpose and peroxide-based cleaning solutions, but water and alcohol-based cleaners should be avoided. Because it bonds permanently to the contact lens surface, Hydra-PEG is a permanent coating. It will become thinner with cleaning, but the base layer will remain intact even after a year of cleaning.6 It may be a beneficial option for patients who have had trouble maintaining comfort and lens wettability, or those who simply want less irritation from dryness and deposits.
Wavefront-guided Sclerals
Custom wavefront technology is often used with refractive surgeries, glasses and contact lenses. It was recently the subject of a study that evaluated the level of higher-order aberration (HOA) correction that is possible with wavefront-guided scleral lenses in keratoconic patients.9 The study concluded that wavefront-guided scleral lenses are capable of compensating for the harmful effects of HOA and can provide visual image quality equivalent to that of normal eyes.9 The ability to produce these lenses and how they will compare with non-ectatic eyes still need to be investigated, however.9
For almost a decade, Greg Gemoules, OD, creator of the LaserFit Scleral Lens System, has been developing his own software to create customized wavefront-guided scleral lenses that eliminate HOAs.10 His LaserFit system uses anterior segment OCT images from the Visante (Zeiss) and wavefront data from the iTrace (Tracey Technologies) aberrometer to design lenses. The lens design is then sent to the Truform Optics Lab, where fabrication takes place. This technology aims to reduce or eliminate HOA issues, including ghosting, smearing of images, halos, glare and both monocular and binocular diplopia.
Custom lens fitting technologies have dramatically changed over the last decade. Now, with the right technology, practitioners can ensure their patients experience faster fits, less chair time and better visual outcomes.
Dr. Pal runs a specialty contact lens and dry eye practice in Toronto. She is the vice chair of the AOA Contact Lens and Cornea Section Council, a member of the Women’s Advisory Board for Alcon and a speaker for Allergan’s dry eye faculty in Canada. She is a consultant for Allergan, Alcon, Bausch + Lomb, CooperVision, Johnson & Johnson Vision Care and Menicon, as well as a facilitator of the STAPLE lens fitting workshops.
1. Bennett ES. GP annual report 2016. Contact Lens Spectrum. October 1, 2016. www.clspectrum.com/issues/2016/october-2016/gp-annual-report-2016-(1). Accessed July 20, 2017.
2. Jedlicka J. Critical measurement to improve scleral lens fitting. Review of Optometry. Sept 2015. www.reviewofoptometry.com/ce/critical-ocular-measurements-to-improve. Accessed July 20, 2017.
3. Caroline PJ, Andre MP. Contact lens case reports: understanding corneal and scleral shape. Contact Lens Spectrum. Jan 1, 2015. www.clspectrum.com/issues/2015/january-2015/contact-lens-case-reports. Accessed July 20, 2017.
4. Barnett M. Multifocal Scleral Lenses. Contact Lens Spectrum. Dec 1, 2015. www.acculens.com/pdf/article-mulitfocal-sclerals.pdf. Accessed July 20, 2017.
5. Carrasquillo K, Barnett M. Scleral Lens Applications in Unique. Contact Lens Spectrum. February 1, 2014. www.acculens.com/pdf/article-scleral-lens-applications-in-unique-populations.pdf. Accessed July 20, 2017.
6. BostonSight® Introduces Innovative Scleral Lens Fitting System. Boston Foundation for Sight. January 25, 2017. static.ow.ly/docs/PressRelease-%20Intro-BostonSightSCLERAL_final_5P1m.pdf. Accessed August 18, 2017.
7. Rumpakis J. New data on contact lens dropouts: an international perspective. Review of Optometry. January 15, 2010. www.reviewofoptometry.com/article/new-data-on-contact-lens-dropouts-an-international-perspective. Accessed July 20, 2017.
8. Sindt CW. The great silicone cover up. Review of Cornea and Contact Lens. April 15, 2015. www.reviewofcontactlenses.com/content/d/technology/c/53979/. Accessed July 20, 2017.
9. Marsack JD, Ravikumar A, Nguyen C, et al. Wavefront-guided scleral lens correction in keratoconus. Optom Vis Sci. 2014 Oct;91(10):1221-30.
10. Gilhawley C. Custom made scleral lenses attract clients from around the world. Invision. March 31, 2016. invisionmag.com/best-of-the-best/1773-best-of-the-best-fit-for-success.html. Accessed July 20, 2017.


