 |
Even Adolf Fick himself, who created the first scleral contact lens in 1888, would be surprised by the longevity of his creation. Composed of blown glass, Fick’s lenses and those that followed enjoyed relatively limited popularity due to difficulties with manufacturing and poor oxygen transmission.1 Materials improvements weren’t enough to keep the design from being eclipsed by corneal-fitted lenses, first gas permeables and then hydrogels.
However, the intractable symptoms experienced by patients with ocular surface disease and their persistent inability to comfortably wear contact lenses—coupled with developments in computer-aided design—has led these specialty lenses to regain popularity in more recent years.2 Sclerals are most commonly indicated for correction of irregular astigmatism in corneal conditions like keratoconus, or following surgical procedures like penetrating keratoplasty.
Fitting the Lens
The appropriate fit for a scleral contact lens is comprised of complete vault of the cornea, clearance of the limbus and alignment with the sclera, with little to no blanching of the conjunctival blood vessels. Vault, or corneal clearance, is defined as the space between the back surface of the scleral lens and the front surface of the cornea.8 Practitioners can use diagnostic lenses when trial fitting a patient; additionally, they can employ optical section slit beam or anterior segment optical coherence tomography (OCT) to assist.
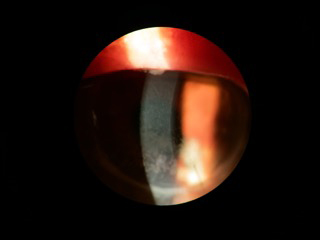 | |
| Fig. 1. Exposure keratopathy patient secondary to incomplete eyelid closure. | |
 | |
| Fig. 2. Central vault displayed using optical section slit beam. |
With the former, corneal clearance is determined via comparison of the known center thickness of the contact lens with the thickness of the post-lens tear fluid reservoir. Instilling fluorescein into the lens chamber may make assessment easier.
OCT, by contrast, employs a cross-sectional view of the cornea and scleral lens to generate a clear measurement of central vault. This minimizes the amount of subjective influence on vault assessment to provide a more precise measurement. OCT-guided fitting is especially useful for troubleshooting cases in which a patient may be experiencing discomfort, but the underlying cause is not evident during a slit lamp examination. For example, if a patient is complaining of rebound redness and soreness following a day of lens wear, but no conjunctival blanching is observed, the lens may be fitting tighter than expected; this can be determined using OCT to assess the degree of lens settling.
Scleral contact lenses can be differentiated based on the overall diameter or location of lens bearing on the eye. Most recently, sclerals have been divided into two groups: corneo-scleral and full scleral. A corneo-scleral GP lens (12.5mm to 15.0mm in diameter) shares bearing on the cornea and the sclera. This is in contrast to a full scleral in which the entire lens bearing is on the sclera. The full scleral group can be further divided into mini-scleral (15.0mm to 18.0mm in diameter) and large scleral (18.0mm to 25.0mm in diameter).12 In comparison to corneal GP lenses, scleral lenses have minimal tear exchange, a thick tear layer and increased lens thickness. It is important to use materials with Dk values of 100 or more to increase oxygen transmissibility.10
Scleral lenses settle into the conjunctiva over a period of time, resulting in a reduction of corneal clearance by 100µm to 150µm. It is necessary to take this into account when evaluating the lens on the eye to ensure there is enough corneal clearance for the patient. In a study evaluating changes in over-refraction after settling, there was no significant change in over-refraction.9 Therefore, visual acuity is not affected following lens settling.9 Though the amount of corneal vault prescribed varies, a minimum of 100µm to 400µm of sagittal depth post-settling is recommended to avoid complications such as apical touch of contact lens on cornea, hypoxia and corneal edema. Some larger diameter scleral lenses may even require up to 500µm of clearance for a proper fit. For patients with ocular surface disease in particular, a greater sagittal depth is typically best. Larger diameter scleral lenses also allow for more hydration of the complete ocular surface area.10
Practitioners should remain aware that the aforementioned rule may not always be the case. A study that attempted to establish an average central corneal vault at which dry eye patients were successful in scleral lenses did find the average vault for successful patients was 380µm, with a standard deviation of 110µm. However, the range of successful vaults in the study led researchers to conclude that precision in central vault was not important in scleral contact lenses for a successful fit over a compromised ocular surface. They also determined there was no correlation between vault and corneal curvature or vault and visual acuity. Patients with as low as 220µm and up to 600µm of central vault were able to achieve a visual acuity of 20/20.8 Ultimately, it is up to practitioners to determine what is best for each patient.
Managing OSD
Many practitioners have begun to use scleral lenses to manage different ocular surface diseases—including keratoconjuctivitis sicca, graft-vs.-host disease, cicatrizing conjunctivitis, neurotrophic keratopathy, exposure keratopathy and limbal stem cell deficiency—in place of extensive artificial tear, topical cyclosporine, punctal occlusion or topical corticosteroid use.3-6 Scleral lens therapy may also bypass the need for more aggressive surgical interventions like tarsorrphaphy, conjunctival flap or amniotic membrane grafting.6
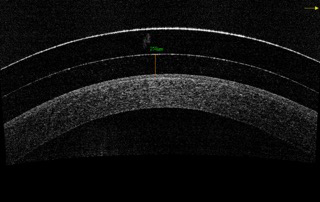 | |
| Fig. 3. Central vault displayed using OCT. |
Patients suffering from ocular surface disease who may be good candidates for scleral lens wear often display symptoms related to ocular pain, visual disturbance and tear film instability.7 The continued hydration and protection provided by these lenses both improves visual acuity and provides lasting comfort. A retrospective study in which 212 subjects were fit with scleral lenses to evaluate the success of long-term therapy found that goals of better visual acuity, comfort, ocular surface protection and resolution of keratopathy were achieved in all but two subjects. Researchers noted the participants had attempted an average of 3.2 other forms of intervention prior to scleral lens wear; they concluded that commercially available scleral lenses are suitable for the management of moderate to severe ocular surface disease.6
Tips for Allergies
Ocular allergies affect up to 30% of the general population and have been shown to result in tear film instability.11 In patients suffering from allergies, scleral lenses can pose more of a problem as the allergens remain in the lens reservoir for prolonged periods of time due to minimal tear exchange underneath the lens. Though little has been published on this topic, from personal experience scleral lens wear with allergies requires more maintenance to avoid bulbar injection and itchy, irritated eyes. A common issue with allergies is the development of a biofilm on the front and back surface of the contact lens. This not only affects the quality of vision but can also lead to lens discomfort. Usually, patients remove their lenses, clean the front and back surface to remove any biofilm or debris buildup and replenish the lens with non-preserved saline multiple times throughout the day.
Use of a prescription strength antihistamine and mast-cell stabilizer combination drop is recommended prior to the application of scleral lenses. The use of non-preserved artificial tears several times throughout the day may be necessary. Adding a few drops of a non-preserved artificial tear with higher viscosity into the lens reservoir may help slow tear exchange.
Giant papillary conjunctivitis (GPC) may occur with scleral lens wear due to mechanical irritation of the lid with potential lens surface debris buildup. GPC can also cause excessive debris issues on the surface of the lens and affect wettability. In patients with allergies, it is best to use a peroxide care system for overnight cleaning. Peroxide systems are neutral and safe to the eye and provide adequate disinfection. Special large cases made specifically for scleral lenses are available for those requiring peroxide cleaning.10
There are numerous scleral lens products available already, with continued improvements in design and function being made daily. Scleral lenses now provide practitioners with a tool to better manage patients who suffer from ocular surface disease and help them regain clear and comfortable vision.
1. Mandell R. Contact Lens Practice. 4th ed. Sprinfield, Ill., Thomas; 1988.
2. Jacobs DS. Update on scleral lenses. Curr Opin Ophthalmol. 2008 Jul;19(4):298-301.
3. Weyns M, Koppen C, Tassignon MJ. Scleral contact lenses as an alternative to tarsorrhaphy for the long-term management of combined exposure and neurotrophic keratopathy. Cornea. 2013 Mar;32(3):359-361.
4. Grey F, Carley F, Biswas S, Tromans C. Scleral contact lens management of bilateral exposure and neurotrophic keratopathy. Cont Lens Anterior Eye. 2012 Dec;35(6):288-291.
5. Schornack MM. Limbal stem cell disease: management with scleral lenses. Clin Exp Optom. 2011 Nov;94(6):592-4.
6. Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology. 2014 Jul;121(7):1398-1405.
7. Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opin Ophthalmol. 2015 Jul;26(4):319-24.
8. Sonsino J, Mathe DS. Central vault in dry eye patients successfully wearing scleral lens. Optom Vis Sci. Sep 2013;90(9):e248-251; discussion 1030.
9. S. Britton CB, Yeung D, Haines L, Sorbara L. Changes in over-refraction after scleral lens settling. Waterloo, Ontario, Canada: School of Optometry & Vision Science, University of Waterloo.
10. van der Worp E SS. A Guide to Scleral Lens Fitting: College of Optometry, Pacific University. 2010.
11. Fujishima H, Toda I, Shimazaki J, Tsubota K. Allergic conjunctivitis and dry eye. Br J Ophthalmol. 1996 Nov;80(11):994-997.
12. Kauffman MJ, Gilmartin CA, Bennett ES, Bassi CJ. A comparison of the short-term settling of three scleral lens designs. Optom Vis Sci. 2014 Dec;91(12):1462-1466.


