A 63-year-old female presented in the clinic for an eye exam for the first time in five years with a best-corrected visual acuity of 20/40 OD and 20/30 OS, with glare disability of 20/80 OU. She reported decreased vision in both eyes and noted she often has difficulty driving at night along with a dry feeling and occasional burning. The patient admitted she uses an unknown brand of eye drops to lubricate her eyes, which provides her with some temporary relief; however, she also stated concern that her symptoms were getting worse.
Following an examination, the patient was educated about chronic dry eye from decreased tear production and increased tear evaporation from meibomian gland dysfunction—the cause of her burning and dryness symptoms. The patient was also informed of the different surgical options and intraocular lens choices available for cataract treatment. The two, it turns out, go hand in hand. Cataract patients need a full dry eye workup to achieve the best possible outcome.
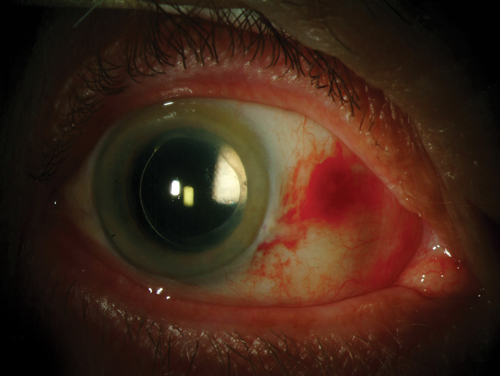 | |
| Subconjunctival hemorrhage after cataract surgery. Photo: Christine W. Sindt, OD |
Examining the Cataract
Considered the most common cause of vision loss in patients over 40, cataract formation has been linked to a number of factors including exposure to ultraviolet radiation from sunlight and other sources, diabetes, hypertension, obesity, smoking and the use of certain medications.1-5 Cataracts can be subdivided into three types based on location: nuclear—the most common type—affects the middle of the lens, while cortical is located in the center of the lens and subcapsular affects the back. Subcapsular cataracts typically progress more quickly than the other two. Each type has different risk factors that contribute to its development, and each must be handled differently.6
Regardless of cataract type, however, many patients develop similar postoperative complications due to untreated ocular surface disease and residual refractive error, even as small as 0.50D.7,8 Uncontrolled ocular disease may lead to residual refractive errors of as much as 1.0D to 2.0D due to its effect on preoperative calculations, which can lead to incorrect toric IOL power or axis placement.9 Research has shown ocular surface disease can also limit the accuracy of preoperative testing like topography and biometry.10-12
So, why do so many patients end up with postoperative residual refractive error? Are the available technology options in fact limited for treating refractive error in our cataract patients? This article will review several corneal and ocular surface considerations to help practitioners successfully manage cataract surgery patients.
Lids and Lashes
The first step to take when a patient presents for a cataract consultation is to perform a full ocular exam from the front to the back of the eye to identify any possible conditions that may limit visual outcome. Begin by looking at the external ocular adnexa. Look for any redness of the face or periorbital area, rhinophyma or other classic signs of rosacea. Finding signs of rosacea can alert you to more advanced meibomian gland dysfunction. Perform a gross examination of the periorbital anatomy to identify any lid dermatochalasis that might cause functional limitations on vision. If the patient has droopy eyelids or dermatachalasis, vision can be limited from these functional problems that can decrease the visual field.
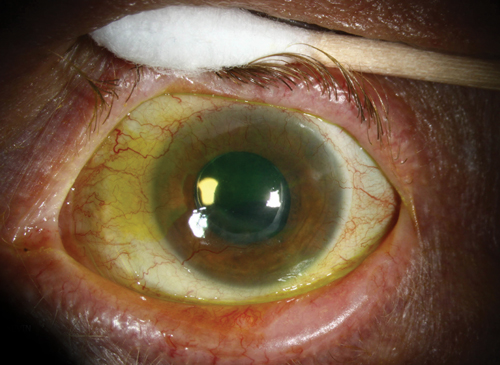 | |
| Pseudophakia and severe dry eye from Graft-versus-host disease. Photo: Christine W. Sindt, OD |
After examining the ocular adnexa, focus on the lids. Demodex is an often ignored and untreated problem that can cause ocular surface issues and other chronic symptoms of itching, irritation and discomfort. This can compound dry eye symptoms that can be made worse after surgery, as patients are often using three to four preserved topical eye drops. If a diagnosis of Demodex is confirmed by plucking a few eyelashes and viewing them under magnification with a microscope, there are a variety of treatment options available today, including commercially prepared kits for in-office administration. Many prescription and OTC treatment options offer a wide range of efficacy against severe and mild cases of Demodex. Lid scrubs and other cleaners contain various combinations of tea tree oil preparations and other active therapeutic ingredients.
Blepharitis is another common complication—up to 59% of patients undergoing cataract surgery present with this disease.13 Classified as either anterior or posterior and chronic or acute, the disease can lead to an array of complications. In the case of cataract patients, anterior blepharitis in particular must be treated prior to surgery by having the patient clean the eyelid margin with prescribed lid hygiene scrubs, foams or cleansers. This decreases the load of bacteria around the lids and reduces the chance of postoperative endophthalmitis. Signs and symptoms of staphylococcal blepharitis—the most common type of anterior blepharitis seen in practice—include lid irritation, scurf, erythema, loss of lashes, crusting and matting with lid debris and red irritated eyelids. Patients with chronic staphylococcal blepharitis are also at increased risk for hordeolum and staphylococcal blepharoconjunctivitis.
As with any lid disease, good lid hygiene is critical to successfully managing staphylococcal blepharitis; I typically prescribe lid cleansing products that contain hypochlorous acid BID for two weeks, then QD as symptoms improve prior to cataract surgery.
Presentations of more severe or chronic staphylococcal blepharitis are typically characterized by some eyelid inflammation. Treatment for these cases involves use of topical antibiotics like topical azithromycin, and/or topical antibiotic/steroid combinations, or both, in addition to lid hygiene regimens. Infectious staphylococcus should be treated with an antibiotic ophthalmic ointment or drop to prevent continued issues. The inclusion of a steroid—as in the case of combination drugs—can also help decrease inflammation resulting from the infection.
Oral medications such as doxycycline dosed at 50mg BID PO or a dose pack of oral azithromycin tapered over five days can be used to treat chronic staphylococcal blepharitis. A comparison of the safety and efficacy of these two in the treatment of patients with meibomian gland dysfunction who had failed to respond to prior conservative management found both drugs improved signs and symptoms significantly, with one caveat: ocular surface staining and bulbar conjunctival redness were significantly better in the azithromycin group, suggesting it may lead to a better overall clinical response with shorter treatment duration.14
Ocular Surface
Both aqueous-deficient dry eye and evaporative dry eye caused by meibomian gland dysfunction must be treated prior to surgery to prevent complications from ocular surface disease. Typically, I feel most dry eye patients present with both types, and so are treated concurrently. A study looked at the prevalence of these two forms of dry eye and found 49% of patients had evaporative dry eye disease, 14% had aqueous deficient and 35% had both forms.15
Dry Eye in Cataract Patients: Prevalent and Pervasive
Not only does this segment of patients have a higher percentage of clinically significant dryness and meibomian gland dysfunction, but these two chronic diseases are often ignored and not properly diagnosed and treated. |
Common management approaches begin with a baseline palliative treatment using artificial tears. If meibomian gland dysfunction and evaporative dry eye are the primary issues, lipid-based artificial tears can be used to supplement the lipid layer, which is often depleted or even missing entirely. For aqueous-deficient dry eye, artificial tears can provide relief. These can be used four times a day; however, if application is needed more frequently due to continued patient symptoms, more viscous tears or nonpreserved artificial tears can also be used. More viscous tears have a longer residence time, offering longer periods of symptomatic relief. Patients with lagophthalmus and incomplete nocturnal lid closure can also be prescribed nighttime ointments, sleep goggles and humidifiers to help with dryness.
For clinically significant dry eye, immunosuppressive topical drops like cyclosporine 0.05% BID and ester-based steroids used short-term can be used to relieve inflammation. Studies have suggested nutritional supplements such as EPA, DHA, GLA, omega-3 and omega-6 may also reduce inflammation, increase tear production and improve meibomian gland secretions. Use of lid scrubs and lid massage after application of heat with eye masks may also improve secretion from the meibomian glands. Meibomian gland expression and meibomian gland probing are other therapeutic options for more advanced gland obstruction. Topical antibiotics, steroids and combination topical drops and ointments can be efficacious in treating meibomian gland dysfunction.
New IOLs
The newest generation of multifocal IOLs approved for use in the United States aim to achieve good distance, intermediate and near vision while decreasing glare and halos. This is done by altering the lens design, including the optics, of earlier multifocal IOLs.
Keep An Eye Out
There are also several complications that can arise following surgery. These include:
|
Reducing the number of diffractive rings decreases the add power. This reduces the diffractive or refractive surface area, allowing less light scatter to decrease glare and halos. Aspheric IOLs also allow for better mesopic contrast sensitivity for better vision at night and improved distance vision. Even though the add powers are decreased, the lower add multifocal IOLs are said to actually deliver better near and intermediate vision than the higher add IOLs while decreasing symptomatic glare and halos.
Cataract surgery has evolved to now be a refractive procedure, giving our patients more options than ever before. The current treatment options are safe, accurate and can treat all types of refractive errors. Staying abreast of the latest advancements is essential to being a part of the co-management process.
Dr. Johnston practices at Georgia Eye Partners in Atlanta, GA, where he serves as the clinical director and residency director. He focuses on ocular surface disease and has experience in comanaging cataract and refractive surgery patients.
1. Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011 Jul;37(4):246-9.
2. Obrosova IG, Chung SS, Kador PF. Diabetic cataracts: mechanisms and management. Diabetes Metab Res Rev. 2010 Mar;26(3):172-80.
3. Glynn RJ, Christen W, Manson JE, et al. Body mass index. An independent predictor of cataract. Arch Ophthalmol. 1995;113:1131-7.
4. Ye J, He J, Wang C, et al. Smoking and risk of age-related cataract: a meta-analysis. Invest Ophthalmol Vis Sci. 2012 Jun 22:53(7):3885-95.
5. Urban RC Jr, Cotlier E. Corticosteroid-induced cataracts. Surv Opthalmol. 1986 Sep-Oct;31(2):102-10.
6. Foster PJ, Wong TY, Machin D, et al. Risk factors for nuclear, cortical and posterior subcapsular cataracts in the Chinese population of Singapore: the Tanjong Pagar Survey. Br J Opthalmol. 2003;87:1112-20.
7. Roberts CW, Elie ER. Dry eye symptoms following cataract surgery. Insight. 2007 Jan-Mar;32(1):14-21.
8. Alio JL, Abdelghany AA, Fernandez-Buenaga R. Management of residual refractive error after cataract surgery. Curr Opin Opthalmol. 2014 Jul:25(4):291-7.
9. Tu E. Cornea Day, ASCRS 2011.
10. Kim P, Plugfelder S, Slomovic A. Top 5 pearls to consider when implanting advanced-technology IOLs in patients with ocular surface disease. Int Ophthalmol Clin. 2012;52(2):51–8.
11. Goldberg D. Preoperative evaluation of patients before cataract and refractive surgery. Int Ophthalmol Clin. 2011;51(2):97–107.
12. Ram J, Gupta A, Brar G, et al. Outcomes of phacoemulsification in patients with dry eye. J Cataract Refract Surg. 2002;28(8):1386–9.
13. Luchs J, Buznego C,Trattler W. Prevalence of blepharitis in patients scheduled for routine cataract surgery. Poster presented at: ASCRS Symposium on Cataract, IOL and Refractive Surgery. April 11, 2010;Boston, MA.
14. Mohsen BK, Fazel AJ, Kiavash V, et al. Oral azithromycin versus doxycycline in meibomian gland dysfunction: a randomized double masked open label clinical trial. Br J Opthalmol. 2015 Feb;99(2):199-204.
15. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012 May;31(5):472-8.
16. Trattler W, Goldberg D, Reilly C. Incidence of concomitant cataract and dry eye: prospective health assessment of cataract patients. Presented at: Wold Cornea Congress; April 8, 2010;Boston, MA.


