You know the scenarios. A patient recently fit with a monthly soft contact lens (CL) is sitting in your chair, complaining of constant redness. And then there’s the veteran two-week wearer who made an urgent appointment due to severe ocular pain, photophobia and discharge, which you suspect could be microbial keratitis. While myriad reasons exist for these symptoms, poor CL care is likely at the top of your list of differentials.
Most of the 45 million contact lens wearers in the United States practice at least some behaviors that put them at risk for serious eye infections, according to a recent report from the CDC.1 One third of lens wearers who responded to the study’s survey recalled never hearing any lens care recommendations from their eye doctor, even though most clinicians reported sharing recommendations always or most of the time.1 So, despite the educational efforts going on in the exam rooms, the importance of lens care isn’t always getting through.
While daily disposable CLs have ushered in a healthier alternative with a care-free routine and reported better compliance, some wearers may still extend their wearing cycles or even sleep in their lenses on occasion, upping their risk of infection.2 Those in monthly and two-week regimens are prone to ocular discomfort, infections or even vision loss if they skimp on proper lens care, storage and disinfection.
“Some of the most common problems happen because patients are trying to save time or money,” says Teresa Narayan, OD, who practices at MedStar Georgetown University Hospital Department of Ophthalmology in Washington DC, and is also an assistant professor at Georgetown University School of Medicine.
Improper contact lens care can lead to complications such as giant papillary conjunctivitis, corneal neovascularization, corneal edema and microbial keratitis, to name a few. “Some of these are more serious than others and many can be treated, but there is a chance of potential permanent vision decrease. I always make sure to educate patients on the risks of contact lens wear and then emphasize that the risks are minimized with proper contact lens care,” Dr. Narayan says.
Here, your colleagues share their five biggest contact lens-related problems and some pearls on how to counter them.
 |
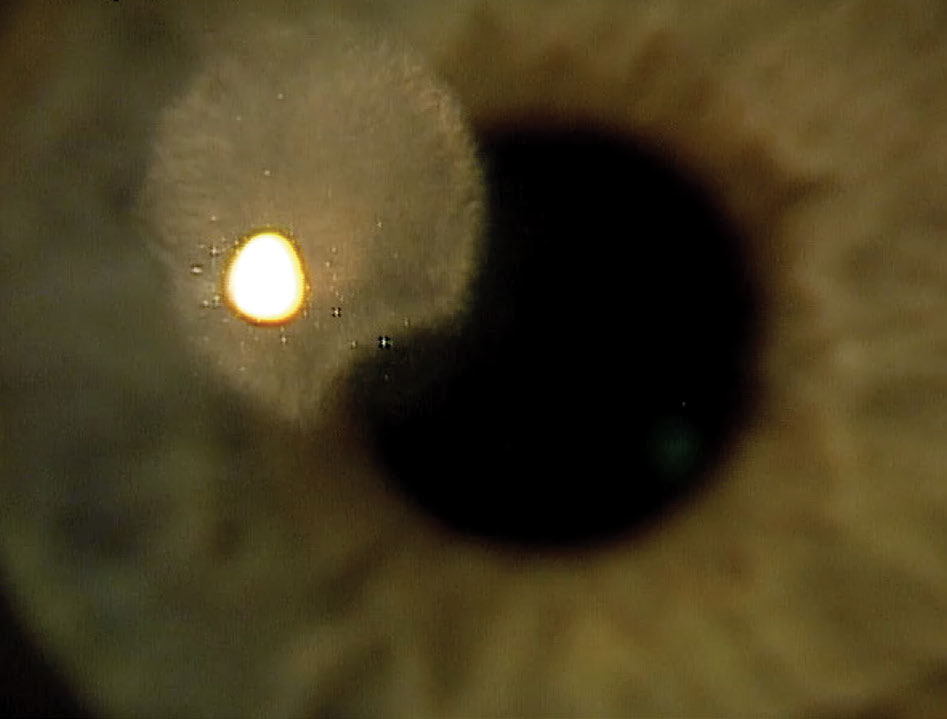
| Patients who ignore proper lens care and handling may find themselves battling a contact lens peripheral ulcer. Photo: Mile Brujic, OD. Click image to enlarge. |
Problem #1: Hygiene Horror Stories
Washing your hands may seem simple enough, but poor hygiene is a common problem in CL wearers that can lead to issues such as microbial keratitis and corneal inflammatory events.3,4
Microbes that can cause infections are auto-inoculated from a person’s fingers, so daily disposable, two-week and monthly wearers need to make sure they are washing their hands prior to lens insertion and removal, says Mile Brujic, OD, who practices at Premier Vision Group in Bowling Green, OH.
“A lack of hand washing is far and away the most common problem I see,” adds Andrew Fischer, OD, of Professional Eyecare Associates in Jasper, IN. “We have sinks in every room, and for a majority of my contact lens patients, I find that I have to remind them to wash their hands before removing the lenses. If they aren’t washing in the office, you can bet they aren’t washing at home.”
To counter this, at every visit—whether the patient is a new wearer or has been in lenses for 20 years—Dr. Fischer does a quick review of key hygiene tips, including the importance of washing hands, replacing cases, not sleeping in lenses not designed to be slept in and avoiding contact with water. Dr. Fischer also gives patients a “Contact Lens Do’s and Don’ts” handout after the contact lens evaluation as a helpful reminder (Table 1).
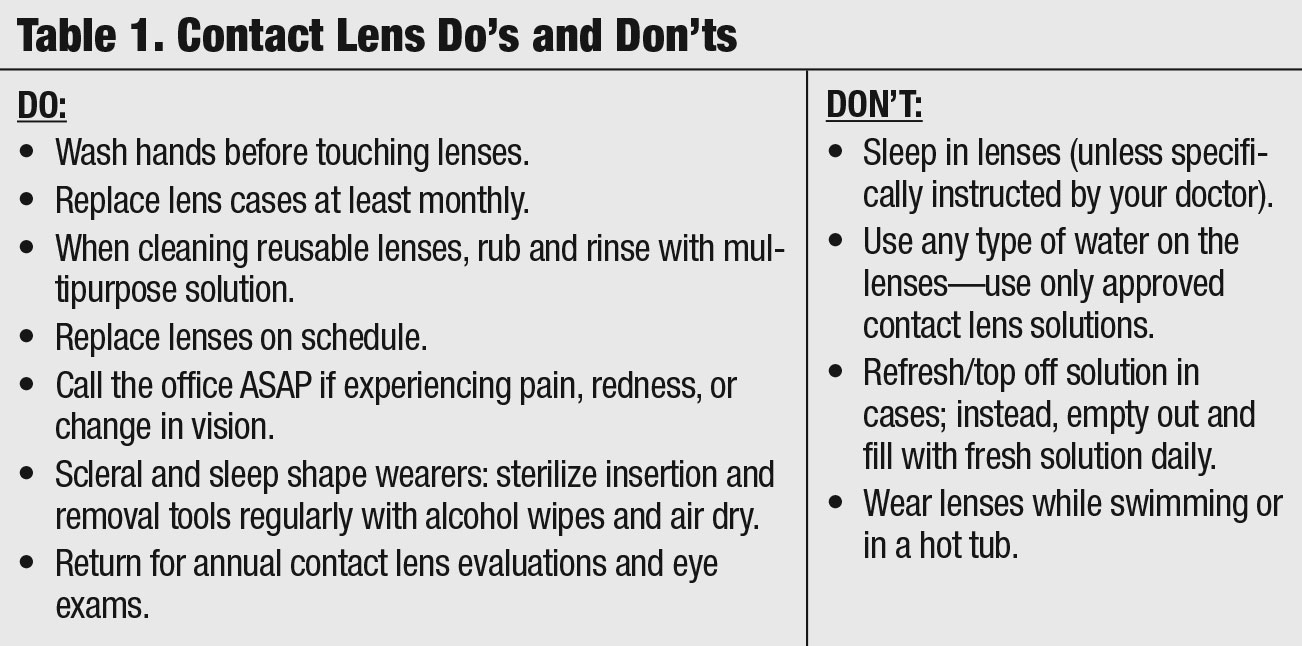 |
| Table 1. Contact Lens Do's and Don'ts. Click table to enlarge. |
Problem #2: Creepy Lens Cases
At Cascadia Eye in the Seattle, WA, area, Steven Turpin, OD, finds that infrequent case replacement is the issue he sees the most. During application and removal training, the patient is usually focused on getting the lenses on and off, and they forget about case replacement, he says. “People often come into the office with their lenses in a case that looks like its been dropped in the mud before they walked in. There was even a patient that came in with his lenses in a case used in the old thermal disinfection units from the ’80s,” Dr. Turpin says. “That’s one reason we generally recommend peroxide products as our primary lens care system. Once the neutralizing disc wears out, patients have to change their case.”
A recent study in Contact Lens & Anterior Eye found storage cases and mobile phones of 63 contact lens-wearing university students were highly contaminated with pathogenic bacteria.5 The investigation found the highest level of contamination was detected in CL storage cases where 18 (52%) bacterial isolates were detected.5 Another study of 2,267 patients that looked at contact lenses and infectious keratitis reported the most important risk factors in the non-daily disposable lens groups were lens cleaning solutions and the failure to renew lens cases.2 Other researchers found 47% of patients said they never replaced their lens cases or only did so if their doctor gave them a new one during their annual visit.6
At Dr. Brujic’s practice, he has all CL patients bring in both their lens cases and solutions during the exam. “I’m still shocked at some of the conditions these patients place medical devices in. The lenses sit all day long on the patients’ eyes, and at night, they store them in these horrific cases.” When Dr. Brujic sees this, he throws the case in the garbage. “I tell the patient, ‘you won’t be using that case anymore, and make sure you clean or replace it every three months.’”
 |
| These non-infectious infiltrates are a tell-tale sign that the patient needs to be re-educated on proper lens care. Photo: Mile Brujic, OD. Click image to enlarge. |
Problem #3: Terrifying Tales of Solutions
Contact lens solutions are another real-world issue, and this is heightened if patients opt for generic products not recommended by their doctor.
CL solution sensitivity can be problematic for some patients, and it’s hard to pinpoint and treat the problem if the person is switching between solutions, especially with some of the generic ones, Dr. Narayan says. The biggest danger is saline solution and patients confusing it with a multipurpose solution, she adds.
“I’ve seen patients with cases of preventable microbial keratitis
because they were using a plain saline that they thought was a cleaning/disinfection solution. If appropriate, I try to recommend two brands of specific contact lens solutions that would work for them and their lenses. I specify two because that way if the store doesn’t have one, or if it’s too expensive, they can get the other option rather than a generic or use saline or water,” she says.
Generic or “cheap” solutions aren’t inherently problematic, but issues can certainly arise, Dr. Turpin adds. If a patient is solely concerned with cost, they will often pick up the first bottle that says it can be used with contacts, which is often just saline solution. “This is always why we ask for specific brands of solution so we can confirm they are using something that keeps the nasty bugs away,” Dr. Turpin says.
With generics, problems usually crop up suddenly because these brands will often alter formulation without changing any of the labeling, he adds. “A patient may be using a generic successfully for a number of years and suddenly have a reaction to it. For this reason, I recommend name brand multipurpose solutions to ensure product consistency,” Dr. Turpin says.
The most common issue Dr. Fischer encounters with generic multipurpose solutions is solution toxicity resulting in fine, diffuse punctate keratitis. “In the same brand of generic solution, additives and preservatives can change from one month to another, so if a patient has a sensitivity to one of the ingredients, it is impossible to always avoid it.”
For patients who are symptomatic and have signs of an allergic reaction, Dr. Turpin will suggest trying a different solution or switching to a daily disposable lens. “We tend to pitch dailies initially because it removes a variable. We don’t have to guess at which solution to try next. We just get rid of solutions all together. That said, if patients are resistant to move into a daily modality, we always recommend a peroxide solution first if they are currently using a multipurpose.”
If a patient is using peroxide, and Dr. Turpin suspects it is causing a problem—high plus or minus patients may not have full neutralization of the peroxide due to lens thickness and experience stinging from the remaining peroxide—he recommends sticking to a name brand multipurpose solution.
Dr. Narayan routinely recommends hydrogen peroxide solutions, which she says are a great alternative, especially if someone has a history of solution sensitivity. Those with allergies and dry eye can really benefit, she adds. The system also seems to help deep clean lenses for those with a history of contact lens build-up and deposits. For peroxide solutions, it’s important to educate patients on the appropriate length of soak time, never rinsing with the solution directly and replacing the case as recommended, she says. “I haven’t experienced any patient having a complication with a peroxide solution if the usage instructions are followed properly.”
However, Crystal Brimer, OD, owner of Focus Eye Care and creator of The Dry Eye Institute in Wilmington, NC, still sees patients who’ve used peroxide-based cleansers directly on the eye or before lens insertion, which has the potential to cause significant corneal toxicity and keratitis. “We see both corneal staining and infiltrates that may or may not be induced partly from CL solution. I immediately ask what they’re using and change it in those cases, and more so switch them to daily disposables and avoid the cleaning regimen altogether,” she says.
Another solution issue: patients will often “hoard” supplies, even after the expiration date, Dr. Brujic says. Since he asks his CL patients to bring in their solutions during the evaluation, if he sees any expired bottles, he’ll throw them away. “I tell the patient why I am throwing it away and explain why I make a specific suggestion for a solution. Sometimes, it’s as simple as saying, ‘The contact lenses you’re wearing are the highest level of lenses available and this solution works best with them.’”
 |
| Infectious ulcers such as this one are a possible complication for patients who don’t replace their contact lens cases in a timely manner. Photo: Mile Brujic, OD. Click image to enlarge. |
Problem #4: The Non-rubbers
For patients in reusable lens modalities, few rub their lenses prior to placing them in their case for overnight storage, Dr. Fischer says.
One study found compliance rates in patients who used CL disinfection systems that require rinsing and rubbing were 45% and 69%, respectively, despite the resultant increased risk of biofilms and pathogens, which can cause contact lens-related dry eye.7
Lens deposits from non-rubbing are another issue Dr. Turpin sees in patients who are non-compliant in their lens care. “It is not necessarily a solution issue itself, just a simple misunderstanding in the handling process. Once we remind patients that mechanically rubbing lenses is the best defense, the problem usually resolves quickly,” he says.
To correct handling issues, Dr. Turpin observes patients’ insertion and removal routines in-office, “without trying to be obvious or overbearing for patients to give us a true representation of how they handle their lenses.” He then makes notes of issues and reviews any useful improvements casually at the end of the visit to avoid any sense of accusation or disapproval, he says. “More often than not, compliance is improved at their next visit,” Dr. Turpin says.
 |
| While many CL-related complications can be treated, some could lead to lasting visual effects, such as this stomal scar from a previous ulcer. Photo: Mile Brujic, OD. Click image to enlarge. |
Problem #5: The Topping-Offers & Other Suspects
Many age-old problems are still around, Dr. Brimer says. “But perhaps we hear less about them because the percentage of daily disposable wearers has increased.” Patients still store their lenses without any rubbing or cleaning, and many top off their solution instead of changing it, or don’t even bother to top off. Added to that, some still extend the wearing cycle beyond the indications for their lens modality, she explains.
Some of these bad habits have actually increased over the years as contact lens technology and materials have improved, Dr. Narayan says. Many lenses are quite comfortable, so patients think they don’t need to clean them, it’s okay to stretch the replacement or even sleep in the lenses as long as they still feel fine, she adds.
Prevention always circles back to patient education, for old and new wearers alike. “Don’t assume that a patient is taking proper care of their lenses just because they have been wearing contact lenses for years. Those patients can have some of the worst habits, especially if nothing bad has happened to them. I always make sure to emphasize that nothing bad has happened yet and that they need to practice appropriate contact lens care if they want to continue a lifetime of healthy eyes and good vision,” Dr. Narayan says.
Another tactic Dr. Brujic uses is to remind patients that the subtle symptoms they are complaining about may be due to their non-compliant habits.
“One of the worst things a patient can do is replace their lenses when they feel like they need to be replaced, because at that point, there are often chronic issues occurring that are getting to the point of feeling different to the patient, and that’s a problem because it may be difficult to revert many of those changes,” Dr. Brujic says.
During an exam, if Dr. Brujic notices any signs that indicate contact lens abuse, he’ll take a picture of the findings with anterior segment photography and show it to the patient. “This seems to hit home with most patients, and they generally will start curbing some of their poor hygiene habits.”
In addition to making sure new and existing contact lens patients are following proper care procedures, clinicians shouldn’t overlook those who have avoided lenses because of the perceived hassle or danger, Dr. Narayan suggests. “Now more than ever, contact lenses are a great option for a majority of patients,” she says. “With new technology and a widened range of parameters, especially in daily lenses, patients should be aware that with proper care, risks are minimized and they can enjoy healthy contact lens wear for years to come.”
1. Healthy contact lens behaviors communicated by eye care providers and recalled by patients—United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(32):693-97. 2. Sauer A, Greth M, Letsch J, et al. Contact lenses and infectious keratitis: from a case-control study to a computation of the risk for wearers. Cornea. January 27, 2020. [Epub ahead of print]. 3. Fonn D, Jones L. Hand hygiene is linked to microbial keratitis and corneal inflammatory events. Cont Lens Anterior Eye. 2019;42(2):132-35. 4. Carnt N, Hoffman JJ, Verma S, et al. Acanthamoeba keratitis: confirmation of the UK outbreak and a prospective case-control study identifying contributing risk factors. Br J Ophthalmol. 2018;102(12):1621-28. 5. Waleed AM, Lua’i AI, Wisam S, Sana J. Antimicrobial susceptibility of bacterial isolates from the conjunctiva, storage cases and mobile phones of university students using contact lenses. Cont Lens Anterior Eye. November 10, 2019. [Epub ahead of print]. 6. Robertson DM, Cavanagh HD. Non-compliance with contact lens wear and care practices: a comparative analysis. Optom Vis Sci. 2011;88(12):1402-8. 7. Ramamoorthy P, Nichols JJ. Compliance factors associated with contact lens-related dry eye. Eye Contact Lens. 2014;40(1):17-22. |


