|
While specialty contact lenses in the infant and toddler populations present unique challenges to even the most adept fitters, they also offer incredible, life-changing potential. The value of mastering fitting techniques in these patients is indisputable. This case focuses on an infant with corneal scarring and traumatic aphakia, and provides rationale and fitting advice for pediatric specialty lens use.
The Case
A 13-month-old female was referred for a contact lens fitting by her cornea specialist. She had sustained a penetrating corneal injury in the right eye approximately three months earlier, resulting in central perforation and a traumatic cataract. At presentation, she was aphakic and had an elevated, 4.00mm linear scar extending across the central cornea from superior nasal to inferior temporal.
Retinoscopy resulted in +13.00D OD and +1.00D OS. The right eye displayed a high degree of scissoring and an overall dim reflex. The patient was resistant to occlusion of the left eye and became visibly agitated, started crying and was no longer cooperative with patching. Horizontal visible iris diameter (HVID) was 11.00mm.
The patient’s parents quickly understood the visual benefits of contact lenses vs. spectacles for their infant daughter; however, they were concerned about the insertion and removal process and questioned her ability to adapt to lens wear. We explained that the younger the child, the easier the process and the faster the adaptation. As children move out of infancy and into toddler age, contact lens fitting, parent-toddler interaction and contact lens adaptation usually become increasingly more difficult. At times, this may result in the inability to fit contact lenses until much later in adolescence. With this reassurance, the parents elected to proceed with a fitting.
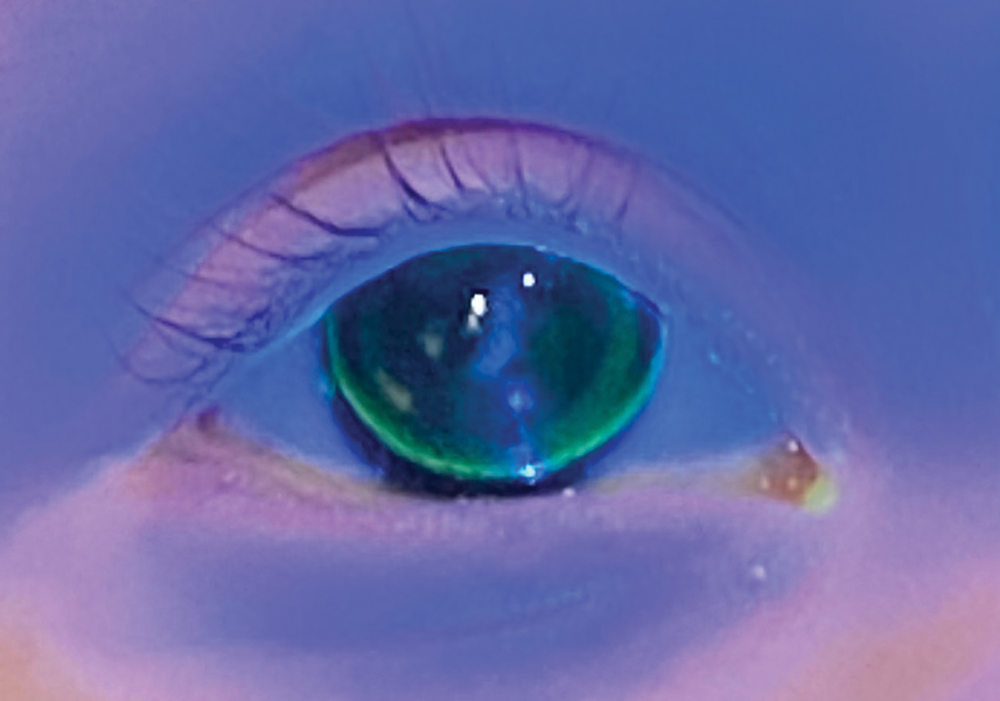 |
| Fig. 1. Note the lack of NaFL centrally in this flat-fitting diagnostic lens. Click image to enlarge. |
Diagnostic Fitting
Due to the presence of both aphakia and corneal irregularity, a gas permeable (GP) lens was selected. As there were no reliable keratometry values to guide base curve selection, a diagnostic lens was prescribed based on diameter and estimated reasonable starting base curve radius (BCR). It was assumed that the central cornea was relatively steep from the retinoscopy value of +13.00D, lower than the +18.00D to +40.00D range typically expected in an infant with aphakia.1 It was therefore assumed the patient had a steep central cornea offsetting, to some degree, the highly hyperopic correction anticipated in pediatric aphakia.
The diagnostic lens selected was +20.00D/6.92mm BCR/10.00mm overall diameter (OAD). A handheld blue light was used to grossly assess the fit. This diagnostic lens decentered superior and temporal, and displayed a lack of sodium fluorescein (NaFL) centrally (Figure 1). This lens was promptly removed and replaced with a steeper one. The parameters of the second lens were +18.50D/6.72mm BCR/10.00mm OAD. The lens was centered on the cornea and displayed a moderate density, green central NaFL pattern consistent with clearance of the central cornea without bubbles. Relative alignment was observed mid-peripherally with a thin line of NaFL at the edge signifying inadequate edge lift. Over-retinoscopy yielded -3.50D. The red reflex was noted as more regular with the GP lens in place.
As is typical in infant aphakia, a 2.50D to 3.00D myopic endpoint was designed to optimize the patient’s visual development.2 The periphery of the lens was flattened to increase edge lift. The following lens of Menicon Z material was ordered: +15.00D/6.72mm BCR/10.00mm OAD with an axial edge lift flattened from the standard 0.12mm to 0.16mm. In addition, plano polycarbonate over-spectacles were prescribed for full-time wear.
Dispensing
The patient returned for a dispensing visit one week later. The lens was centrally located with mild central clearance without bubbles, mid-peripheral alignment and improved edge lift with a visible band approximately 1.00mm in width. Approximately 0.50mm to 1.00mm of lens movement was visible with blink and normal eye movement. Over-retinoscopy was approximated at -3.00D, consistent with the desired myopic endpoint. The parents were instructed on proper lens care and trained on insertion and removal until they demonstrated proficiency. The lens was dispensed for daytime wear and permitted napping.
Follow-up
The patient returned one week later with her contact lens in place. The parents noted no dislocations with about 12 hours of daily wear. The patient was, for the first time since her injury, cooperative with patching. While patched, she was able to pick up and play with toys within arm’s reach. Lens tolerance had increased rapidly over the first two to three days. At this point, the patient demonstrated no eye-rubbing, redness or excess tearing with the lens in place following a five- to 10-minute period of active distraction by her parents. The lens fit and ocular health were unchanged from the dispensing. Continued success and adaptation were noted at her subsequent follow-up one month later.
Discussion
Three primary options exist for correcting ametropia in infants with contact lenses: corneal GP lenses, silicone elastomer lenses and custom soft lenses. While each lens option is feasible in infant management, GPs tend to be the preferred choice. Benefits include ease of handling, nearly unlimited physical and visual customization and a relatively low infection risk.3 In addition, for children with corneal scarring, these lenses provide optimal vision correction by masking anterior corneal irregularity.
We can explain the rationale behind our fitting patterns with the lifestyle, vision requirements and anatomy of an infant. These patients are highly active, requiring a lens that provides excellent stability. Larger corneal lenses typically offer this through improved centration and decreased movement. These patients also nap daily. Using materials that allow adequate oxygen flow while napping is essential to minimize lens insertion and removal during the day.
Vision correction depends on the indication for lens wear. If the patient is phakic, full distance correction with an equalized stimulus for accommodation is the goal. If the patient is bilaterally or unilaterally aphakic, a 3.00D myopic refractive endpoint should be the target. This will place the child’s far point near 33.00cm, allowing the child to develop vision and visual motor skills within their typical viewing and playing range. Polycarbonate over-spectacles are advised.
Infant eyes typically have steeper corneas and smaller HVIDs compared with adults.4 As a result, GPs with a relatively steep BCR are common in this patient population. Consistent with the fitting strategy used in the Infant Aphakia Treatment Study, I target the central curvature at approximately 1.00D to 1.50D steeper than the keratometry value, commonly siding on the smaller end of this spectrum due to my preference for larger corneal lenses.5
As keratometry is often not feasible or reliable in this age group, a bracketed fitting strategy is recommended. This entails using GPs to estimate the corneal curvature by identifying a BCR that displays touch over the central cornea and the next closest BCR that displays clearance. It can then be assumed that the corneal curvature lies between the two points.
In this patient, a lens with a BCR of 6.92mm/48.75D displayed touch and a lens with a BCR of 6.72mm/50.25D displayed clearance. It can therefore be assumed the corneal curvature was between 48.75D and 50.25D. We ended up ordering the 50.25D BCR lens, as it displayed adequate centration and clearance and had no bubble formation. Continuing with this example, if the 50.25D lens displayed excess clearance with bubble formation, the fitter would know to order a lens with a BCR with less than 50.25D but more than 48.75D. As noted previously, corneal lenses with a large diameter are commonly preferred due to their stability and centration. “Larger” in this situation is a relative term, as the diameter relies on the HVID. A reasonable starting point is 1.50mm to 1.00mm smaller than the HVID, commonly resulting in diameters ranging from 9.50mm to 11.00mm.
The importance of providing a clear image for visual development at a young age is inarguable. While there are several options for vision correction in infants and toddlers, none rival the versatility of corneal GP lenses. With nearly unlimited parameters and an excellent safety profile, this modality is the standard in pediatric contact lens fitting.
| 1. McQuaid K, Young TL. Rigid gas permeable contact lens changes in the aphakic infant. CLAO J. 1998;24(1):36-40. 2. Moore BD. Optometric management of congenital cataracts. J Am Optom Assoc. 1994;65(10):719-24. 3. Keay L, Edwards K, Naduvilath T, et al. Factors affecting the morbidity of contact lens-related microbial keratitis: a population study. Invest Ophthalmol Vis Sci. 2006;47(10):4302-8. 4. Borish IM. Clinical Refraction. 3rd ed. Chicago, IL: Professional Press; 1975: 61-74. 5. Lambert SR, Buckley EG, Drews-Botsch C, et al. The infant aphakia treatment study: design and clinical measures at enrollment. Arch Ophthalmol. 2010;128(1):21-7. |