 |
It can be easy to get lost in the customization options available with scleral lenses. While most help create healthy and comfortable lenses, front toric vision correction stands out from the rest. Sometimes, it can be the difference between a satisfied patient and a loyal patient.
The Case
A 73-year-old female presented for a second opinion on her contact lens correction. The patient’s chief complaint was poor visual quality in her right eye due to glare and ghosting. She was diagnosed with Salzmann’s nodular corneal degeneration 15 years earlier and has been wearing corneal gas permeable (GP) lenses for over 40 years. She was refit with a piggyback lens system three years earlier to improve the centration of her lenses. Lately, however, she has been experiencing frustration as a result of her visual symptoms. She was interested in any contact lens option that would improve visual quality.
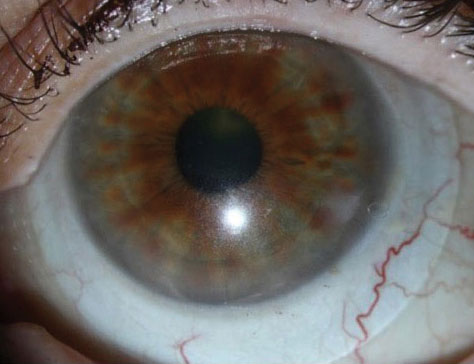
Slit-lamp examination revealed superior nasal, elevated gray-blue nodules consistent with her corneal degeneration diagnosis. The ocular surface was otherwise unremarkable.
The patient’s GP lenses were highly decentered inferior temporal in both eyes. The superior nasal nodules appeared to play a role in decentration, as they displaced the lenses inferior and temporal in both eyes. Acuities were measured at 20/40 OU. A +0.50 spherical over-refraction improved vision to 20/30 OU, and a sphero-cylindrical over-refraction improved it to 20/20 OU. It was unclear if lens decentration, flexure or true residual astigmatism was resulting in the toric over-refraction.
Although the patient had potential for improved vision based on the results of the over-refraction, the current piggyback lens design made this unlikely for two reasons. First, decentration would continue to be a major limiting factor as the nodules displaced the lens. Even with piggybacking, the current centration was not adequate. This decentration was likely contributing to the glare symptoms as her pupil approached the limits of her optic zone. In addition, if true residual astigmatism were present, a front toric corneal design would be difficult to stabilize due to the superior corneal nodules displacing the lens inferiorly. It also has unpredictable rotational stability, as the lens edge contacts the corneal nodules with each blink.
After reviewing possible approaches, a scleral lens was the best option. This would provide the opportunity for GP optics, centration independent of corneal anatomy, a larger optic zone to limit interaction with mydriasis in low lighting and the opportunity to incorporate a stable front toric correction if needed.
 |
| The flat meridian “O” is rotated 30 degrees to the left, and the front cylinder vertical reference is at 6 o’clock OS. Click image to enlarge. |
Diagnostic Fitting
The diagnostic lens chosen for both the right and left eyes was the Custom Stable Elite (Valley Contax) -2.00D/45.00D/16.8mm with standard limbal and scleral zones [+6 (flat)/-4 (steep)].
Following 30 minutes of settling, central clearance OD was 250µm with approximately 75µm of clearance over the most elevated corneal nodule located in the mid-peripheral cornea, and the limbal clearance was roughly 25µm in all quadrants. The scleral zone displayed mild edge lift along the flat meridian (this design uses two laser-marked “Os” to indicate the flat meridian) with alignment along the steep meridian.
The flat meridian was rotated 25 degrees to the right using the horizontal meridian as a reference. The left eye displayed 200µm centrally with 50µm of clearance over the most elevated corneal nodule located in the superior-nasal peripheral cornea. The limbal clearance was full at roughly 25µm in all quadrants. The scleral zone displayed moderate edge lift along the flat meridian with alignment along the steep meridian. The flat meridian was rotated 30 degrees to the left. Both lenses were well centered.
A spherical over-refraction of +1.50 OD and +1.25 OS improved vision to 20/30+ OD and OS and 20/30+2 OU. A sphero-cylindrical over-refraction yielded +1.75-0.75x050 OD and +1.50-0.75x130 OS. This resulted in acuities of 20/20 OU. Over-keratometry was performed with a spherical result, ruling out lens flexure as the potential cause of the cylindrical over-refraction.
Based on these results, the following lenses were ordered: -0.25-0.75x025 (25-degree right rotation)/45.00D/16.8mm/limbal clearance zone: standard/scleral landing zone: +4 (flat)/-2 (steep) OD and -0.50-0.75x160 (30-degree left rotation)/45.00D/16.8mm/limbal clearance zone: standard/scleral landing zone: +2 (flat)/-2 (steep) OS.
Both lenses were modified in the flat meridian of the scleral zone to compensate for edge lift, while the steep meridians were left standard. The over-refraction axis was adjusted to compensate for lens rotation.
Dispensing
The patient returned one week later. As is typical in our office, the patient’s lenses were inserted, and she was given approximately 30 minutes for them to settle.
Upon entering the exam room, the patient said, “I have one word for you—‘Wow!’” She went on to comment that she couldn’t recall the last time her vision felt so crisp and clear. Her acuities were 20/20 OU with a plano over-refraction in both eyes. The central fit of both lenses was consistent with the diagnostic fit. The flat meridian markings were rotated to the same degree as they were in the diagnostic fitting. Within this lens design, an additional vertical laser mark was placed at the anticipated 6 o’clock position for a simple axis check. The patient was educated on all pertinent wear and care instructions.
Follow-up
The patient returned a week later having worn her lenses for seven hours. She praised her visual quality, reporting excellent initial and lasting comfort and vision with a daily average wear time of 12 hours. In addition, she had noticed a reduction in glare while driving at night. Her acuities were 20/20 OU, and her central clearances were 200µm and 150µm in the right and left eyes, respectively. Roughly 25µm of clearance over the most elevated nodules, full limbal clearance and scleral alignment was observed in both eyes. Rotation was consistent with previous measures.
The patient returned for her one-month follow-up with continued clarity and comfort. The fit was unchanged, and her ocular surface tolerated lens wear well.
Discussion
Scleral lenses offer excellent stability on the eye. With this stability comes the ability to incorporate front toric vision correction with predictable rotational stability.
Front toric scleral lenses can be stabilized through prism ballasting and toric scleral shape. When a front toric correction is added to a lens with a symmetrical scleral zone design, the lens must be balanced using prism ballasting to minimize lens rotation. The amount of recommended ballasting varies based on lens design. The ballast can be increased if unstable rotation is observed; however, keep gravity and oxygen availability in mind.
With the ballast adding weight to the inferior portion of the lens, inferior decentration can be problematic when excess amounts of prism are incorporated. In addition, the thickness of the inferior lens can present challenges with oxygen availability to the inferior cornea. Use the least amount of ballast to stabilize the lens and high- to hyper-Dk materials.
A more favorable situation arises when scleral toricity can be used to stabilize the lens. When toric scleral zones are appropriate, the interaction between the toricity in the shape of the lens and the toricity of the sclera creates rotational stability. This allows for stability without the added weight or thickness. A diagnostic set with standard toricity is extremely helpful in determining the lens power to order. By carefully measuring the rotation of the diagnostic lens, the over-refraction axis can be properly compensated.
Considering the right eye of the patient in this case, the diagnostic lens was rotated 25 degrees to the right; thus, the axis of the over-refraction was modified from 50 degrees to 25 degrees. Note that this compensation is performed on the over-refraction, not the manifest refraction. We anticipate the ordered lens will rotate the same amount of degrees as the diagnostic lens. If this is the case, the axis will align as intended. Some scleral lens designs provide additional rotation assessment lens markings to ensure that the predicted rotation with the diagnostic lens is the observed rotation with the ordered lens.
During the diagnostic fitting process, I always perform both spherical and sphero-cylindrical over-refractions to gauge the patient’s best-corrected acuity and identify meaningful amounts of residual astigmatism (I consider a front toric when residual astigmatism is 0.75 or greater). By addressing meaningful residual astigmatism, we are able to aid our patients in achieving their full visual potential and improving their overall quality of vision and satisfaction with their lenses.


