 |
Today we can employ a growing repertoire of lens modifications and fitting strategies to maneuver scleral lenses around conjunctival and scleral obstacles. This case highlights a patient with a pair of conjunctival obstacles and provides a step-by-step approach to achieving a comfortable, healthy lens fit in similar patients.
The Case
A 69-year-old female was referred for a scleral lens fitting. She had a history of high frequency, bilateral filamentary keratitis recalcitrant to topical management. The disease was highly asymmetric, with the left eye experiencing more frequent and numerous filaments than the right. Scleral lenses are becoming more regularly indicated to help manage ocular surface disease.
The patient preferred to be fit with a scleral lens in her left eye and continue with topical management in her right due to her hesitation toward handling scleral lenses and her guarded optimism for success based on previous failures with therapy.
The patient’s uncorrected visual acuities were 20/20 OU. She had clear lids and lashes, a clear cornea and a deep and quiet anterior chamber. I noted centered posterior chamber intraocular lenses with open capsules OU. She also had a clear conjunctiva OD; however, I observed a multi-lobulated, flesh-toned lesion inferior nasal to the limbus in her left eye. The referring cornea specialist had determined these lesions to be nonmalignant and was reluctant to remove them, citing the risk for exacerbation of ocular surface disease following ocular surface surgery.
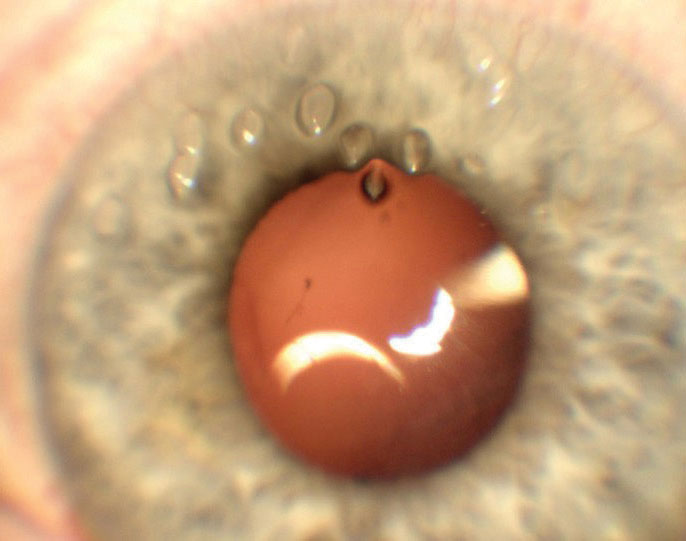 |
| Imaging of the superior cornea shows several visible filaments. |
Diagnostic Fitting
I used a 15.80mm Custom Stable Elite lens (Valley Contax) to perform a diagnostic fitting. I selected this diameter to provide complete corneal coverage while minimizing interaction with the patient’s conjunctival obstacles. This lens features a toric scleral zone to offer optimal stability, centration and comfort.1,2 The lens was -2.00/43.00/15.80 OS with standard limbal and scleral zones of +5 (flat)/-2 (steep).
An over-refraction of +4.25D yielded 20/20 vision. After settling, the central clearance was 200μm with a limbal clearance of 25μm and scleral alignment 360°. The lens was positioned with the flat meridian along the vertical meridian. The edge of the lens was in contact with the conjunctival nodules. Due to being semi-mobile, the nodules were displaced nasally by the lens edge, creating blanching of the surrounding tissue. Based on the multi-lobulated nature, width and height of the conjunctival nodules, I chose to proceed with an edge notch.
Notch Design
The design of a lens notch is often enhanced by clinical experience and intuition; however, following a few guiding principles can significantly improve your chance of success. First, measure the distance of the lesion from the limbus to help determine how far into the lens the scleral notch should extend. Second, measure the widest portion of the lesion expected to interact with the lens edge. For our patient, the nodules were located 1.50mm outside of the limbus and measured 4.00mm at their widest point.
To determine the depth of the lens notch, first subtract the horizontal visible iris diameter (HVID) from the diameter of the lens and divide the resulting number by two. Upon subtracting the patient’s HVID (11.80mm) from the lens diameter (15.80mm) and cutting the number in half, I found that her lens coverage, or expected distance the lens would extend beyond the limbus, was 2.00mm.
Next, subtract the distance the lesion is located from the limbus from the lens coverage (2.00mm-1.50mm) to find the notch depth (0.50mm). Based on the diagnostic fitting, this starting point can be modified as needed. If significant decentration is unavoidable, you may need to adjust the depth of the notch accordingly.
To compensate for the curved shape of a notch while avoiding larger obstacles, additional depth may be needed. In this case, the width of the lesion was relatively large at 4.00mm, so I added an additional 0.25mm to my notch depth to avoid interacting with the entire width of the nodules. I have found that adding 0.50mm to 1.00mm allows for optimal avoidance of the lesion.
The final specification is the location on the lens the notch should be placed. When working with a toric scleral landing zone, the location of the notch must be specified in accordance with the lens’s rotation on the eye. Each lens manufacturer may advise a point of reference for this measurement. For the lens design used in this case, the reference points are the flat meridian markings. I used my slit beam to measure the degrees from the reference points to where I wanted the middle of the notch to be. The lab then uses that information to design the rest of the notch.
Based on my fitting and pre-fitting measurements, I ordered the following lens: +4.50/43.00/15.80 OS with standard limbal and scleral zones [+5 (flat)/-2 (steep)] with a notch 0.75mmx5.00mm centered 50° counterclockwise.
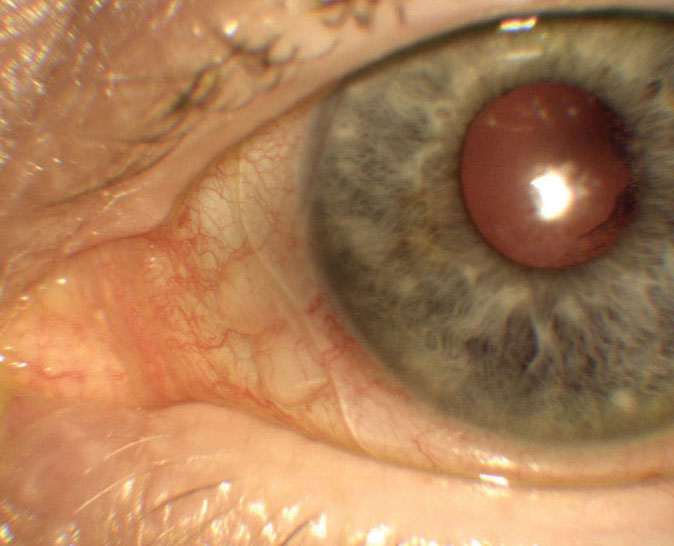 |
| Imaging displays appropriate notch size and location. |
Original Dispensing
The patient returned three days later with new onset severe pain in the left eye, foreign body sensation, tearing and photophobia. Her slit lamp exam revealed 20 superior filaments. I removed the filaments without complication and sent the patient home in a soft bandage contact lens with antibiotic coverage.
Dispensing Redo
The patient came back three days later with complete resolution of her previous symptoms. Following removal of the bandage lens, the cornea was deemed intact and the patient ready for dispensing. Upon insertion, the scleral notch abutted the conjunctival lesions without displacing them. The remainder of the fit was consistent with the diagnostic fitting. Based on the patient’s propensity for rapid filament formation, I advised her to gradually increase lens usage from eight to 10 hours of daily wear on the day of dispensing to 12 to 16 hours of daily wear.
Follow-up
The patient returned to the clinic a week later having already worn the lens for six hours at the time of her visit. She reported excellent comfort and denied any new surface complications. The lens fit was unchanged from dispensing aside from an anticipated decrease in central clearance from 200μm to 150μm.
The patient had continued comfort in her scleral lens without any recurrences of her filamentary keratitis in her left eye throughout the following month. Her cornea and conjunctival tissue supported the lens well with no adverse signs noted.
Discussion
Three primary strategies exist to address conjunctival obstacles in patients requiring scleral lenses. Occasionally, we can employ a small-diameter lens that lands between the lesion and the limbus. By selecting a smaller lens, we may be able to avoid interacting with the lesion entirely. When this is not feasible, we are left deciding between an edge vault and a notch. Vaults allow for a controlled area of the lens to be lifted up and over conjunctival obstacles without having to remove a portion of the lens. They are designed to land in alignment with the conjunctival tissue and distribute weight evenly over the lesion. Vaults are created by the lathe during lens fabrication, allowing for a higher degree of precision and specification. This, however, also limits their size and depth, according to the limitations of modern lathing systems.
Unlike vaults, notches are created with hand-held tools. This inherently trades the specificity of a vault for more flexibility in size and depth. Notches are excellent for wider lesions, non-uniform or multi-lobulated lesions and lesions of greater height. In addition, tissues that are more prone to rapid change or are thinner and more delicate (i.e., filtering blebs, shallow-filtering tube coverage) may benefit from the complete avoidance of interaction offered by a notch.
While these fitting strategies often take on a trial and error approach, the severity and rapidity of filament formation in this patient reminds us that time is of the essence in patients with severe ocular surface disease. By following a few fundamental steps, we can get our patients the lenses they need as quickly and efficiently as possible and increase our likelihood of success.
1. Visser ES, Van der Linden BJ, Otten HM, et al. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013;90(10):1078-85. 2. Visser ES, Visser R, van Lier HJ, et al. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007;33(1):21-5. |


