Once you realize you are dealing with an irregular cornea, how do you feel? Scared? Excited? Nervous? Perhaps all of the above?
If you’re an eye care practitioner who is energized by the challenge of improving vision for patients who cannot see well with spectacles, then you might already be familiar with some of the lenses in our arsenal.
On the other hand, if you are a little more hesitant or are looking to expand your options for irregular cornea patients, here is a primer on the examination information you should be gathering and the lens options worth considering.
Exam Data
Examining any patient with an irregular cornea starts with obtaining an extensive case history. While it’s important to understand a patient’s current complaints in detail, it also benefits us to know their past ocular surgical procedures and contact lens wear history.
With regards to a patient’s complaints, assessing their level of blur, halos, glare, flare and difficulties with night vision can uncover telling information.
Using tomographic or topographic maps can assist in evaluating the tear film and the cornea’s front and back surface characteristics.
After a careful manifest refraction, consider whether the patient is experiencing any anisometropia, aniseikonia or both with spectacles, as this will bolster your case for prescribing medically necessary correction with contact lenses.
Ocular dryness history should also be explored, preferably with a validated questionnaire that can be repeated at subsequent office visits to evaluate any changes in signs and symptoms over time.
A quick inquiry into the patient’s vocation and hobbies can automatically steer your evaluation toward certain lens designs. For example, a truck driver may require a gas permeable (GP) lens for best acuity while driving. A retired patient, though, may desire a part-time wear option where acuity may not be as crucial for a successful outcome.
A critical look at a patient’s dexterity, hygiene and potential for lens handling limitations can help you determine whether to include or exclude certain lens modalities from the start or recommend additional assistance. For example, an elderly patient with rheumatoid arthritis may not be able to manipulate their fingers to apply and remove a lens as easily. A patient with a tremor may not be able to steady their hands long enough to handle a lens. To help, assistive devices exist that can come in handy when patient handling on insertion or removal presents a challenge.
Your initial physical examination of a patient should include measuring best-corrected acuity (if the patient currently wears spectacles or contact lenses), a pinhole acuity, if indicated, and uncorrected visual acuity (usually taken after any entering lenses are assessed). Following a fresh manifest refraction, you will have another measure of best-corrected spectacle acuity.
Contact lens patients should have a pair of backup spectacles in case they ever find themselves in a situation where they cannot wear their lenses, especially so they do not feel tempted to over-wear them.
Patients will often express a desire for a backup pair of spectacles if given the option, even if their vision is not as crisp as it is with their contact lenses. If the patient has a high amount of anisometropia in their manifest refraction, it might be useful to trial frame the result obtained and cut the sphere, cylinder powers or both down until you achieve the best balance of tolerable anisometropia and best visual acuity.
Other entering data to consider when choosing a contact lens modality include: pupil size, horizontal visible iris diameter, vertical fissure width, corneal status (e.g., ectasia, scarring, transplant status, sutures, dystrophy, ocular surface disease, endothelial cell count), lens status (e.g., cataract, intraocular lens, aphakic), conjunctival abnormalities (e.g., pinguecula, pterygium, conjunctivochalasis) and lid abnormalities (e.g., ptosis, dermatochalasis, rosacea, meibomian gland dysfunction). Pay careful attention to the best-corrected visual acuity and any comorbidities, such as retinal abnormalities, glaucoma or previous ocular surgeries (e.g., glaucoma bleb or tube), which can also inform the fitting process moving forward.
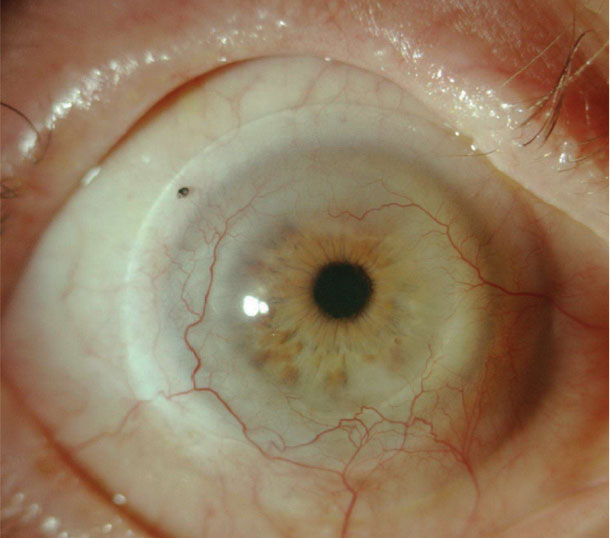 |
This 61-year-old Eastern European male presented with a chemical burn in his right eye after an industrial accident. The patient was only able to achieve a fluctuating 20/50 acuity with a corneal GP lens and was experiencing difficulty with adaptation because he only wore the lens in one eye. Today, he sees 20/25 out of a scleral lens in the right eye. |
If ocular surface disease is present, treating it prior to commencing lens wear is a must; however, patients with severe ocular surface disease, especially in the presence of other irregular corneal findings, often benefit from scleral lens wear to help treat and manage their condition.1,2
For patients with a history of corneal transplant, obtaining a baseline endothelial cell count and a pachymetry value is recommended prior to lens fitting. This will allow you to monitor the health of the graft in the presence of the lens, modify the lens or lens wearing schedule or refer the patient for further surgical intervention if indicated based on changes in the health of the transplant.3,4
Corneas with endothelial cell densities below 1000cells/mm2 are at an increased risk for swelling and decompensation.5 Chronic endothelial decompensation occurs when endothelial cell density is between 400cells/mm2 to 700cells/mm2.5,6 When fitting these patients, consider if the visual benefit of a scleral lens is worth the risk of decompensation or if a lens with a smaller diameter, greater tear exchange and better oxygen transmission would be more beneficial.
Further analyzing the endothelial cell count scan can also help predict the risk associated with a scleral lens; specifically, a coefficient of variation <30% and a hexagonality value >50% bode well for fitting success.7
Pachymetry measurements also assist with assessing endothelial cell function. An increase in pachymetry of more than 20µm to 40µm after scleral lens removal is concerning.7,8 Post-keratoplasty patients fit with scleral lenses require close follow-up to monitor for signs of hypoxia and rejection or failure.
Examining any patient with an irregular cornea starts with obtaining an extensive case history. While it’s important to understand a patient’s current complaints in detail, it also benefits us to know their past ocular surgical procedures and contact lens wear history.
With regards to a patient’s complaints, assessing their level of blur, halos, glare, flare and difficulties with night vision can uncover telling information.
Using tomographic or topographic maps can assist in evaluating the tear film and the cornea’s front and back surface characteristics.
After a careful manifest refraction, consider whether the patient is experiencing any anisometropia, aniseikonia or both with spectacles, as this will bolster your case for prescribing medically necessary correction with contact lenses.
Ocular dryness history should also be explored, preferably with a validated questionnaire that can be repeated at subsequent office visits to evaluate any changes in signs and symptoms over time.
A quick inquiry into the patient’s vocation and hobbies can automatically steer your evaluation toward certain lens designs. For example, a truck driver may require a gas permeable (GP) lens for best acuity while driving. A retired patient, though, may desire a part-time wear option where acuity may not be as crucial for a successful outcome.
A critical look at a patient’s dexterity, hygiene and potential for lens handling limitations can help you determine whether to include or exclude certain lens modalities from the start or recommend additional assistance. For example, an elderly patient with rheumatoid arthritis may not be able to manipulate their fingers to apply and remove a lens as easily. A patient with a tremor may not be able to steady their hands long enough to handle a lens. To help, assistive devices exist that can come in handy when patient handling on insertion or removal presents a challenge.
Your initial physical examination of a patient should include measuring best-corrected acuity (if the patient currently wears spectacles or contact lenses), a pinhole acuity, if indicated, and uncorrected visual acuity (usually taken after any entering lenses are assessed). Following a fresh manifest refraction, you will have another measure of best-corrected spectacle acuity.
Contact lens patients should have a pair of backup spectacles in case they ever find themselves in a situation where they cannot wear their lenses, especially so they do not feel tempted to over-wear them.
Patients will often express a desire for a backup pair of spectacles if given the option, even if their vision is not as crisp as it is with their contact lenses. If the patient has a high amount of anisometropia in their manifest refraction, it might be useful to trial frame the result obtained and cut the sphere, cylinder powers or both down until you achieve the best balance of tolerable anisometropia and best visual acuity.
Other entering data to consider when choosing a contact lens modality include: pupil size, horizontal visible iris diameter, vertical fissure width, corneal status (e.g., ectasia, scarring, transplant status, sutures, dystrophy, ocular surface disease, endothelial cell count), lens status (e.g., cataract, intraocular lens, aphakic), conjunctival abnormalities (e.g., pinguecula, pterygium, conjunctivochalasis) and lid abnormalities (e.g., ptosis, dermatochalasis, rosacea, meibomian gland dysfunction). Pay careful attention to the best-corrected visual acuity and any comorbidities, such as retinal abnormalities, glaucoma or previous ocular surgeries (e.g., glaucoma bleb or tube), which can also inform the fitting process moving forward.
If ocular surface disease is present, treating it prior to commencing lens wear is a must; however, patients with severe ocular surface disease, especially in the presence of other irregular corneal findings, often benefit from scleral lens wear to help treat and manage their condition.1,2
For patients with a history of corneal transplant, obtaining a baseline endothelial cell count and a pachymetry value is recommended prior to lens fitting. This will allow you to monitor the health of the graft in the presence of the lens, modify the lens or lens wearing schedule or refer the patient for further surgical intervention if indicated based on changes in the health of the transplant.3,4
Corneas with endothelial cell densities below 1000cells/mm2 are at an increased risk for swelling and decompensation.5 Chronic endothelial decompensation occurs when endothelial cell density is between 400cells/mm2 to 700cells/mm2.5,6 When fitting these patients, consider if the visual benefit of a scleral lens is worth the risk of decompensation or if a lens with a smaller diameter, greater tear exchange and better oxygen transmission would be more beneficial.
Further analyzing the endothelial cell count scan can also help predict the risk associated with a scleral lens; specifically, a coefficient of variation <30% and a hexagonality value >50% bode well for fitting success.7
Pachymetry measurements also assist with assessing endothelial cell function. An increase in pachymetry of more than 20µm to 40µm after scleral lens removal is concerning.7,8 Post-keratoplasty patients fit with scleral lenses require close follow-up to monitor for signs of hypoxia and rejection or failure.
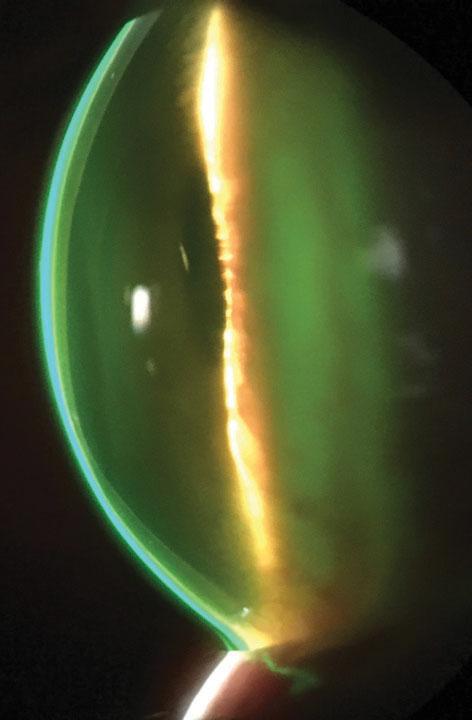 |
Fluorescein pattern of a scleral lens on an eye with keratoconus. Photo by John Gelles, OD |
Lens Options
Sometimes the contact lens solution for an irregular cornea is as simple as a soft sphere or toric lens that you likely already have in a trial lens set in your office. This is an easy and straightforward fix for a patient’s reduced vision. These lenses have planned short-interval replacement schedules and, if lost, ripped or torn, can easily be switched out for a new lens.
If a patient needs powers outside the available parameters, or if the patient has a larger or smaller horizontal visible iris diameter than average, a custom soft design may be indicated.
Many custom soft lens designs are available in quarterly replacement schedules, and some are available on a monthly replacement basis. These fits are straightforward, and key characteristics include lens coverage, centration and movement. Timely follow-up visits can confirm the lenses are being used properly and the fit is not causing any harm to the eye.
In lenses with quarterly or longer replacement cycles, a hydrogen peroxide-based solution may provide better deposit resistance and a more comfortable, preservative-free lens wearing experience.
If the vision achieved with standard soft contact lens designs is not acceptable, it may be because the corneal irregularity is too great. In this case, a specialty lens design for the irregular cornea may be necessary. Designs of this type are available for both prolate ectasias and oblate post-surgical corneal profiles. They generally correct vision in one of two ways, either by increasing center thickness to mask irregular astigmatism or by using aspheric designs to limit aberrations.
The lenses can have center thickness values ranging from 0.4mm to 0.6mm to accommodate corneal irregularity, although newer “thin” designs are closer to 0.2mm in thickness. These thin designs can even out tear distribution underneath the soft lens with better draping to improve peripheral fit and are more ideal for low cone, pellucid, post-graft and post-surgical cases due to their increased oxygen transmissibility.9
Various irregular cornea soft lens designs may also incorporate toricity to help with any residual astigmatism present in the over-refraction. These lenses are available in traditional hydrogel materials and latheable silicone hydrogel material to increase oxygen transmissibility and reduce the risk of hypoxia and neovascularization. They are great options for mild to moderate irregularity and for patients hesitant to try a GP lens.10
It is important to set visual acuity expectations with patients prior to trying these designs, as acuity may not be as good as that achieved with corneal GP designs (although sometimes it is just as good, if not better).
In the office, perform a careful over-refraction and pay attention to lens cylinder axis and any rotation that may be present on the diagnostic lens to ensure the best visual outcome. Some specialty soft lens designs are fit with the assistance of sodium fluorescein that has a high molecular weight; however, with the current difficulty in sourcing such fluorescein, make sure you return to the laboratory’s specific fitting guide for the particular lens you’re working with, as some of the lens fitting characteristics and troubleshooting options are unique to each design.
In patients with corneal irregularity, a corneal GP lens design is often the easiest and most cost-effective way to achieve optimal visual acuity. Indeed, in patients with a post-transplant eye, it may also be the most physiologically favorable design if fit properly to facilitate good tear exchange and oxygen transmissibility.
If you’re fitting a specialty GP lens design for the irregular cornea, the steep keratometry reading is often a good starting point; however, the best strategy is to follow the manufacturer’s fitting guide and use the sodium fluorescein pattern and over-refraction to guide the fitting process.
Many designs have unique characteristics that allow you to independently flatten or steepen different areas of the lens to achieve the optimal fit. Acquiring slit lamp photos, videos or both and calling a laboratory consultant can also help alleviate potential doubts and answer questions so that you can continue on your way.
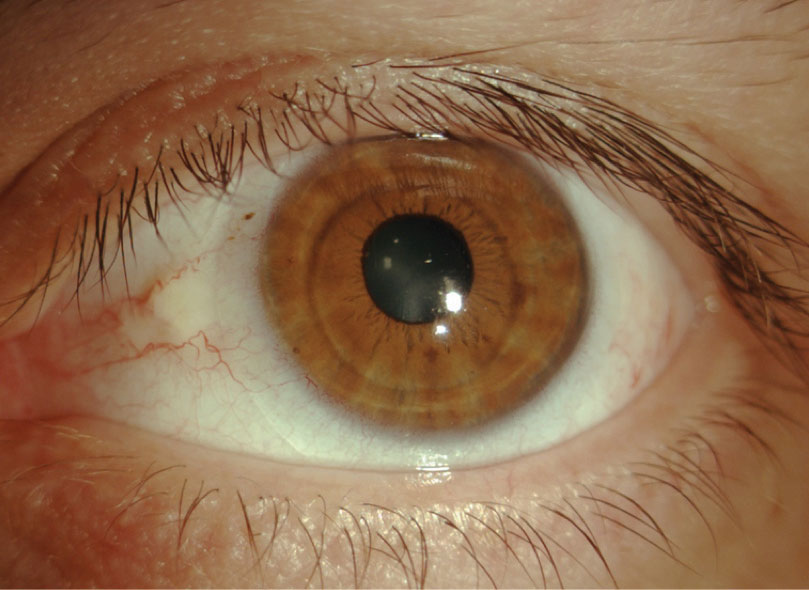 |
A 32-year-old Hispanic male with pellucid marginal degeneration and an elevated pinguecula in each eye presented complaining of visual distortion with his spectacles. He had discontinued GP lens use due to discomfort issues and challenges that arose from using the lenses at his job. Despite achieving 20/25 acuity in a scleral lens with a toric periphery (to avoid compression on the pinguecula), the patient decided he would rather wear a specialty soft lens that gave him 20/30 acuity. |
Piggybacking a GP lens on top of a soft lens is also an option but is sometimes forgotten by fitters. Soft contact lenses can cushion the cornea and improve GP lens stability, centration or both. A piggyback can also be a bridge that keeps a patient in a more cost-effective corneal GP lens design and prevents them from having to transition to hybrid or scleral lenses.
Practitioners should independently assess the fit of each lens (soft and GP) for movement and keep in mind that the soft contact lens clinically only contributes about 20% of its power to the system.11,12
Fitters should also be attentive to the overall oxygen transmissibility of the lens system. For optimal oxygen transmissibility, silicone hydrogel soft lens designs are preferred. It may be cumbersome, however, for patients to have to handle and care for two lenses per eye instead of one. This can be streamlined somewhat with the recommendation of a hydrogen peroxide-based care system and one case for each set of lenses or a daily disposable silicone hydrogel soft lens option.
Hybrid contact lenses have a GP lens center surrounded by a soft lens skirt. These designs provide excellent visual acuity due to the GP center and ensure patient comfort is maintained as the soft lens interacts with the eyelid. These lenses also provide excellent on-eye lens centration and can be purchased with add-on coating to enhance lens wettability and comfort. They generally require less lens vault than a scleral lens and, therefore, can provide enhanced oxygen transmissibility when fit properly with acceptable movement on blink. Hybrid lenses may even allow for more rapid tear exchange than scleral lenses.13
Modern scleral lenses have rapidly risen in popularity over the last decade, and their availability in high Dk GP materials has fueled their use in irregular and regular cornea applications.
These lenses are large enough to tuck under lids and range in size from approximately 13mm to 22mm, providing exceptional comfort for the patient. The addition of toric- or quadrant-specific peripheral curves can help ensure lens stability. Along with this stability comes the ability to include advanced applications, such as multifocal and front toric optics or edge lift options to vault conjunctival irregularities.
When fitting the highly irregular cornea with a scleral lens, limited tear exchange, asymmetric vault over a highly irregular surface and centration are still concerns. Additionally, vision can be compromised as the lens base curve becomes steeper and the underlying tear layer more convex. Switching to an oblate lens design can help reduce lens power and improve vision by reducing distortion. Other fitting challenges, such as conjunctival prolapse, epithelial bogging, midday fogging and limbal bearing, are unique to scleral lens wear and should also be addressed if they arise during the fitting process.14
In patients for whom even a highly customized scleral lens cannot achieve the best vision or physiology, a custom-molded, optically clear prosthetic scleral device may be indicated. Only once a practitioner completes the comprehensive certification process for these lenses are they able to fit patients in their office.15
Impression material is applied to the eye with a specialized tray device to create an impression mold of the cornea and sclera. This mold is then sent to the laboratory, which uses laser-imaging technology to create a contact lens that matches the impression. These lenses include highly customized options, such as prism, multifocal optics, decentered optics and higher-order aberration correction.16
Over the years, practitioners have found new ways to restore visual function to patients in need. As of 2019, there are more contact lens options for the irregular cornea than ever before.
As specialty lens fitting grows in popularity, we not only see life-changing improvements in visual function in our patients but we also see industry growth fueling further innovation and development.
When you’re ready to take the plunge, just remember the variety of lenses you have at your disposal. While the first lens you try might not be the perfect fit, you can achieve success (and avoid complications) with persistence, motivation, trial and error and the guidance of expert laboratory consultants.
Dr. Sicks is an assistant professor at the Illinois College of Optometry and serves as a clinical attending in the Cornea Center for Clinical Excellence at the Illinois Eye Institute. She lectures and participates in research on specialty contact lenses.
| 1. Schornack MM, Pyle J, Patel SV. Scleral lenses in the management of ocular surface disease. Ophthalmology. 2014;121(7):1398-405. 2. Shorter E, Harthan J, Nau CB, et al. Scleral lenses in the management of corneal irregularity and ocular surface disease. Eye Contact Lens. 2018;44(6):372-8. 3. Jackson AJ, Robinson FO, Frazer DG, et al. Corneal guttata: a comparative clinical and specular micrographic study. Eye (Lond). 1999;13(6):737-43. 4. Palay DA, Kangas TA, Stulting RD, et al. The effects of donor age on the outcome of penetrating keratoplasty in adults. Ophthalmology. 1997;104(10):1576-9. 5. Lass JH, Sugar A, Benetz BA, et al. Endothelial cell density to predict endothelial graft failure after penetrating keratoplasty. Arch Ophthalmol. 2010;128(1):63-9. 6. Melles G, Lander F, Rietveld F, et al. A new surgical technique for deep stromal, anterior lamellar keratoplasty. Br J Ophthalmol. 1999;83(3):327-33. 7. Sindt CW. Endothelial cell density: when it becomes a contraindication? AiLES Conference: scleral lens 2.0: from the past, the lens of the future. Rome. June 11, 2018. 8. Barnett M, Johns LK. Contemporary Scleral Lenses: Theory and Application. Vol. 4. Bentham Science Publishers, 2017. 9. Kerasoft Thin. www.kerasoftlens.com/professional/why-choose-thin/. Accessed March 11, 2019. 10. Saraç Ö, Kars ME, Temel B, et al. Clinical evaluation of different types of contact lenses in keratoconus management. Cont Lens Anterior Eye. February 23, 2019. 11. Woo M, Weissman BA. Effective optics of piggyback soft contact lenses. Cont Lens Spectrum. 2011. 12. Michaud L, Brazeau D, Corbeil ME, et al. Contribution of soft lenses of various powers to the optics of a piggy-back system on regular corneas. Cont Lens Anterior Eye. 2013;36(6):318-23. 13. Achenbach P, Bergmanson J, Miller W, et al. Tear exchange beneath a vaulted hybrid contact lens. Cont Lens Anterior Eye. 2018;41(1):S39-40. 14. Walker MK, Bergmanson JP, Miller WL, et al. Complications and fitting challenges associated with scleral contact lenses: a review. Cont Lens Anterior Eye. 2016;39(2):88-96. 15. Eyeprint Prosthetics. www.eyeprintpro.com/. Accessed March 11, 2019. 16. Eyeprint Prosthetics. Case reports. www.eyeprintpro.com/case-reports/. Accessed March 11, 2019. |


