Corneal crosslinking (CXL) has gained widespread clinical acceptance since April 2016 when the FDA approved the Avedro KXL system, which slows or halts progressive keratoconus. Today, CXL is the standard of care for progressive keratoconus, and many medical insurances cover the procedure.1 However, most keratoconus patients still require specialty contact lenses for the best visual results post-CXL. Recently, there has been talk that CXL may make it easier to prescribe contact lenses for keratoconus.
Although the primary goal of CXL is disease stability, the procedure can also reduce corneal curvature and surface irregularity. According to data submitted to the FDA, the maximum keratometry value in the CXL treatment group decreased by 1.6D from baseline to one year.2 With a flatter cornea after the procedure, it seems intuitive that contact lens practitioners would find it easier to prescribe contact lenses. Is there peer-reviewed literature to support this claim, though? Here, we take a closer look.
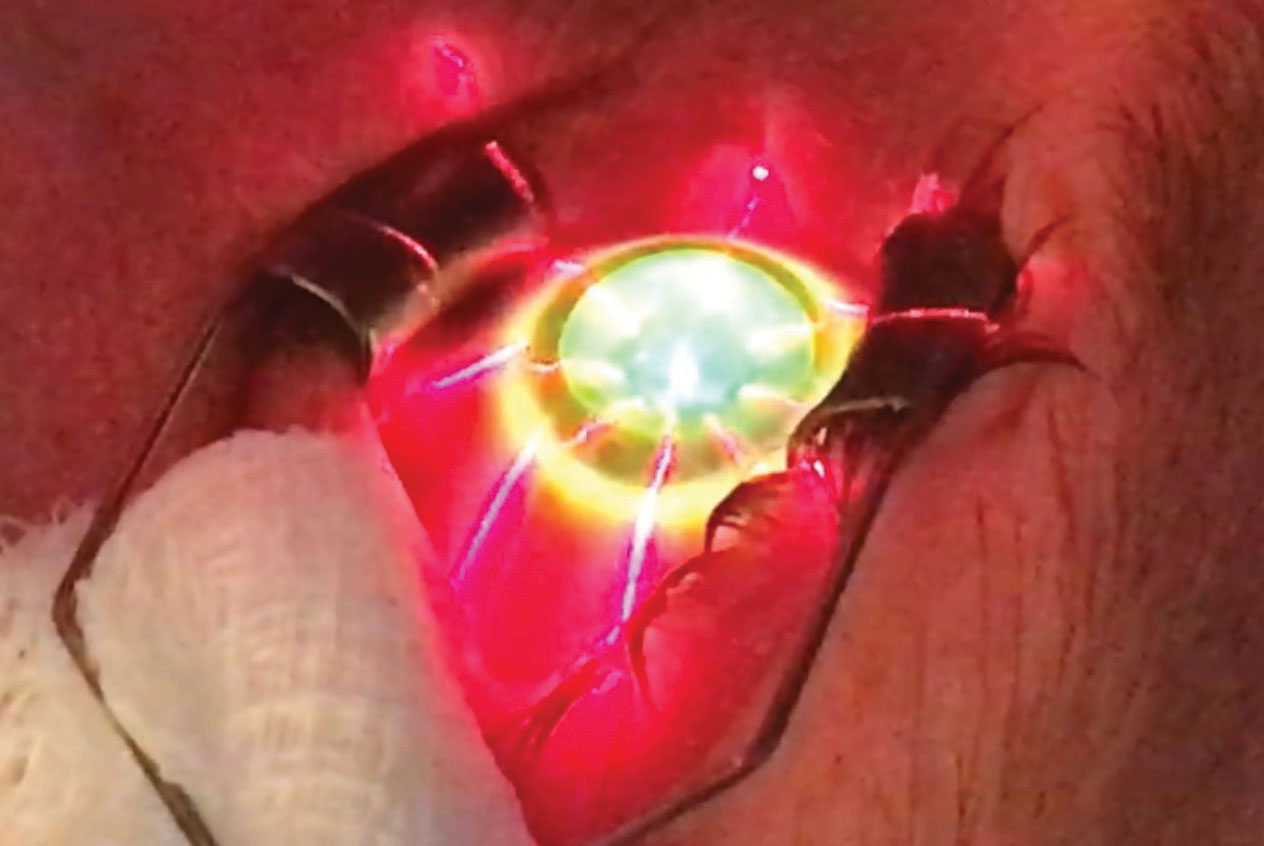 |
| This patient is undergoing CXL. Photo: John Gelles, OD. Click image to enlarge. |
CXL and Lens Tolerance
General descriptions of contact lens prescribing after CXL underscore the importance of visual restoration following the surgery.3,4 CXL temporarily reduces corneal sensitivity for about six months, after which point sensitivity levels return to their preoperative levels.5 In a study using confocal microscopy, we can see that the sub-basal nerve plexus was not visible in 90% of patients at one month postoperative but that corneal innervation nearly restored to preoperative levels by six months.5 These results corroborate the findings of an earlier study investigating accelerated CXL, which also found that the sub-basal nerve fiber density was reduced following CXL.6 However, it notes that the density measurements did not reach preoperative values until 12 months post-op.6
From this literature, we can conclude that it is likely that the reduced corneal sensation after CXL enhances contact lens tolerance during the first six months after the procedure.
Researchers evaluated 20 eyes of 14 patients with keratoconus who underwent CXL and reported improved rigid gas permeable (RGP) fitting relationships and subjective patient comfort.7 Among their findings, they note that all patients reported acceptable fits, with 20% experiencing an increase in near-ideal fit and 65% an improvement in subjective comfort with an eight-hour-longer duration of comfortable contact lens wear.7 While subjectivity exists with what constitutes an improved RGP fitting relationship, the observed improvement in subjective patient comfort could be due to the relative hypoesthesia of the cornea following CXL.
A review paper on CXL recently mentioned an unpublished study reporting on contact lens tolerance in a small prospective randomized clinical trial of 10 subjects (eight keratoconus, two ectasia) who underwent CXL.8 Participants were prescribed a hybrid contact lens three months post-op.8 Prior to CXL, 62.5% of the keratoconus patients (5/8) claimed partial or good lens tolerance, whereas 90% of all patients (9/10) reported satisfactory lens tolerance at the conclusion of the study.8 The authors state that, despite the limited sample size and the singular lens design, these findings might show early evidence of improved contact lens tolerance in post-CXL patients.8
Upon looking closer at the previous two studies, several things are evident. The practitioner’s skill level may contribute to improved fitting relationships, patient comfort and lens tolerance. It is unclear in either study if the same practitioner prescribed contact lenses to the participants before and after CXL. If the patients’ original lenses were prescribed by a less-experienced practitioner who handed the reins off to a more skilled practitioner after CXL, it would not be surprising to find better fitting relationships and lens satisfaction. In the latter study, there is no control for the lens design prior to CXL. These patients could have preoperatively worn a poorly fit RGP lens and postoperatively been prescribed a well fit hybrid lens and experienced improvement simply due to changes in the lens type or fitting relationship, not CXL. Overall, the sample sizes in both studies are too small to draw a reliable, accurate conclusion.
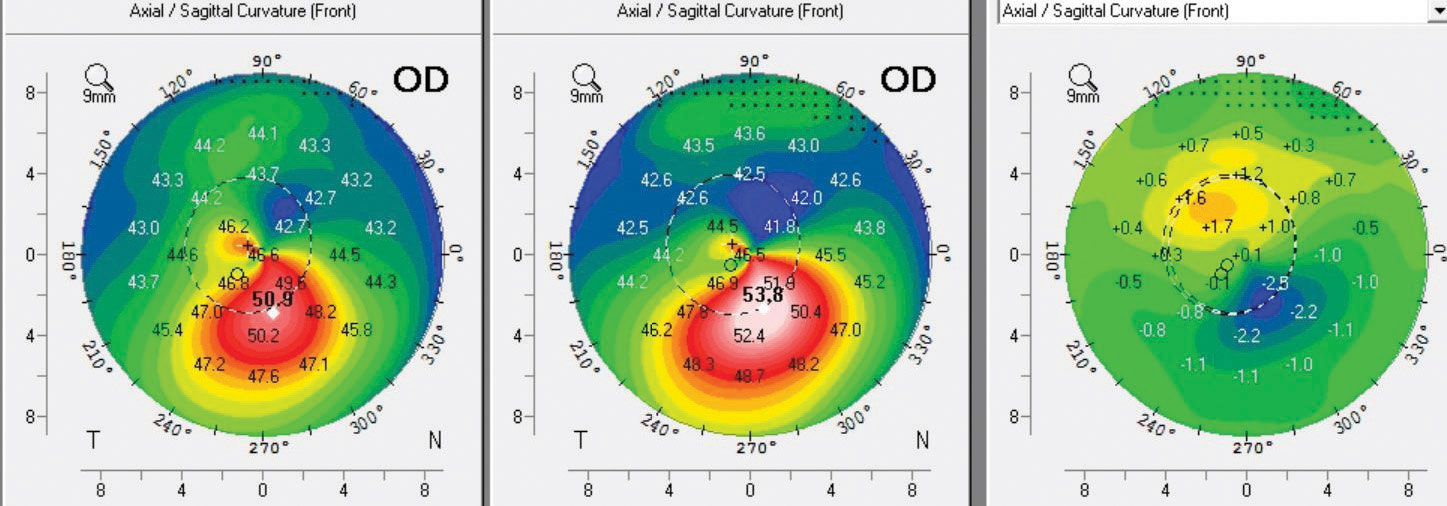 |
| The left map was taken six months post-op, the center map was taken pre-op and the right map is the difference or subtractive map showing 2.5D of Kmax flattening. Note the superior steepening and the inferior flattening over the cone, which represents normalization of the corneal shape. This patient had a robust response to CXL. Photo: John Gelles, OD. Click image to enlarge. |
CXL and Lens Prescribing
To be clear, asking whether CXL makes it is easier to prescribe contact lenses is different from asking whether CXL increases patient contact lens tolerance. We are currently lacking published data assessing the ease of prescribing contact lenses after CXL. In future studies, contact lens practitioners could be surveyed on the average chair time and number of visits required to obtain a final contact lens Rx. Until then, however, we cannot definitively answer this question.
Despite scleral contact lenses—which completely vault the cornea surface—growing in popularity, it is unknown whether CXL enhances their tolerability. With more time and attention appointed to lens haptic to scleral alignment rather than corneal alignment, it seems unlikely that CXL would impact scleral lens prescribing. However, a recent case study used a profilometer—an ocular surface topographer—to show that CXL for keratoconus altered the scleral shape.9 Keep in mind that this is simply one case that raises more questions about the global ocular shape effects of CXL.
Linking It Together
The claim that CXL makes it easier for a clinician to prescribe contact lenses appears unfounded, at least for the time being. This isn’t to overshadow the fact that CXL may improve contact lens tolerance, possibly by causing short-term corneal hypoesthesia. Until compelling evidence comes forth to suggest otherwise, the primary rationale for undergoing CXL should be to stabilize disease progression.
Dr. Chou owns ReVision Optometry, a referral center for treating keratoconus and prescribing scleral contact lenses in San Diego, CA.
Dr. Gelles is the director of the specialty contact lens division at the Cornea and Laser Eye Institute (CLEI) and the CLEI Center for Keratoconus in Teaneck, NJ.
1. Avedro. Is cross-linking covered by insurance? www.livingwithkeratoconus.com/is-cross-linking-right-for-me/is-cross-linking-covered-by-insurance/. Accessed March 13, 2019. 2. Hersh PS, Stulting RD, Muller D, et al. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017;124(9):1259-70. 3. Severinsky B. Contact lens use after corneal crosslinking. RCCL. 2016;153(5):28-32. 4. Michaud L, Breton L. Contact lens fitting post-corneal cross-linking. Contact Lens Spectrum. 2018. 5. Ünlü M, Yüksel E, Bilgihan K. Effect of corneal cross-linking on contact lens tolerance in keratoconus. Clin Exp Optom. 2017;100(4):369-74. 6. Ozgurhan EB, Celik U, Bozhurt E, et al. Evaluation of subbasal nerve morphology and corneal sensation after accelerated corneal collagen cross-linking treatment on keratoconus. Curr Eye Res. 2015;40(5):484-9. 7. Singh K, Bhattacharyya M, Arora R, et al. Alterations in contact lens fitting parameters following cross-linking in keratoconus patients of Indian ethnicity. Int Ophthalmol. 2018;38(4):1521-30. 8. Chang CY, Hersh PS. Corneal collagen cross-linking: a review of 1-year outcomes. Eye Contact Lens. 2014;40(6):345-52. 9. DeNaeyer G, Sanders D. Collagen crosslinking for keratoconus can change scleral shape. J Cont Lens Res Sci. 2018;2(1):e15-21. |


