A Deeper Look at DEWS II Making the Diagnosis with TFOS DEWS II |
Over the last two decades, a substantial number of new contact lens (CL) materials and lens care solutions have come onto the market. Despite these advancements, symptoms of discomfort and dryness persist in lens wearers, particularly at the end of the day. Studies estimate that 50% of all lens wearers continue to complain of dryness and discomfort at the end of the day, and 25% to 30% of all wearers will cease lens wear at some point, either temporarily or permanently.1-4
To address the issue of contact lens discomfort (CLD), in 2013 the Tear Film and Ocular Surface Society (TFOS) published a series of papers to better understand CLD and determine factors that may help alleviate its negative effects. Among the topics discussed in the report is the impact of CL materials, care systems and design on CLD.5 For most practitioners, addressing lens material and solution choices for CLD patients may seem like an obvious way to help. Many studies show this can be beneficial and provide a solution to the associated discomfort and, in many cases, reduced wearing time. However, to effectively manage CLD, there is another factor that must always be considered—the patient.6,7 It is important to remember that even the best material-solution combination will not work well if the patient’s ocular surface is compromised.
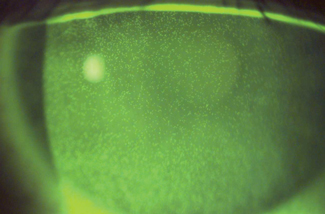 |
| Here is an example of solution-induced corneal staining. This can be reduced by pre-application of a CMC-based artificial lubricant. |
Some potential patient and ocular surface factors associated with CLD include: female sex, younger age, poor tear film quality and quantity, seasonal allergies, systemic medications such as oral contraceptives and isotretinoin, diet, hydration, alcohol use, smoking, compliance with lens replacement and care systems and bulbar conjunctival and corneal staining.4,6,7
Last summer, TFOS introduced their second Dry Eye Workshop (DEWS II) report. While the report discusses dry eye disease (DED) in non-contact lens wearers, its management and therapy section can help practitioners better manage CL patients who remain symptomatic despite lens material and care system optimization.5
Here are some key takeaways from DEWS II that can guide our CLD management in clinical practice, as well as some evidence-based pearls not included in DEWS II.
Ocular Lubricants
CL wear rapidly destabilizes the already thin tear film. A typical CL is around 100µm thick, while the average tear film is 5µm to 7µm thick. As such, contact lens wear causes a rapid tear film break-up that typically occurs after six to seven seconds, at best, over the lens. In symptomatic CL wearers, the break-up is often even more rapid.8,9
The DEWS II management and therapy report covers many different formulations of ocular lubricants.5 While many are not indicated for use with CLs in situ, they can be used pre- and post-lens insertion to improve the ocular surface and enhance the tear film.10
In another study, use of a microemulsion of mineral oil and a polar phospholipid surfactant as a CL rewetting agent over the lens resulted in improved comfort, reduced corneal staining and reduced lid wiper epitheliopathy.11 The pre-application of a lubricant containing carboxymethylcellulose (CMC) can reduce solution-induced corneal staining, and a CMC-based lubricant can improve the initial comfort of a daily disposable CL compared with application directly from the blister-pack.12,13 Thus, it appears that the concomitant use of lubricants (typically instilled pre-lens insertion and post-lens removal) can be beneficial in managing various complications associated with CL wear.
One key point to remember when applying topical drops with contact lenses is that the latter take up any preservatives, so any drops containing benzalkonium chloride should be avoided.14 Drops that are preserved with newer, high molecular weight preservatives and oxidative preservatives are safe to use with soft lenses, and if concerns arise, using the drops with daily disposable lenses will limit lens uptake and release.
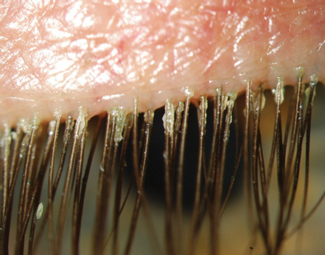 |
| Demodex blepharitis in a rigid gas permeable contact lens wearer suffering from long-term discomfort. |
Punctal Occlusion
This therapeutic approach, particularly in conjunction with other therapies, is valuable in the management of DED in non-lens wearers.5 However, relatively few studies investigate the impact of punctal occlusion on CLD and in those few studies, the data is somewhat equivocal, suggesting that there may be better options to improve CLD than plugging the puncta.15-17
Lid Hygiene
It has been well established that lid conditions such as blepharitis and the overabundance of Demodex impact the ocular surface. The tear film changes that occur with these conditions will inevitably impact CL wearers and likely result in CLD. However, while many studies investigate the impact of lid hygiene on improving symptoms and signs of DED in non-lens wearers, little research exists on the impact of blepharitis or Demodex management in improving symptoms of discomfort in CL wearers. Of note, some studies suggest that the presence of Demodex is greater in CL wearers, symptomatic CL wearers have more demodex and the presence of Demodex results in a greater chance of CL dropout and discontinuation.18-20 Given these points, management of both blepharitis and Demodex in CL wearers would be appropriate. Options here include lid hygiene wipes, topical antibiotics, topical ivermectin cream, oral ivermectin and various tea-tree oil preparations.5,21
Meibomian Gland Dysfunction
The association between CLD and meibomian gland dysfunction (MGD) is well known, and the positive impact of MGD treatment on improved comfort in CL wearers was first demonstrated more than 30 years ago.22 Additionally, several studies have proposed that CL wear results in increased MGD prevalence.23-26 As such, practitioners should carefully evaluate patients with CLD for MGD. If it turns out a patient does have MGD, a suitable treatment plan should be initiated.
Mechanical cleaning of the meibomian glands in cases of MGD includes forceful expression with or without heat, physical expression with heat using in-office devices such as LipiFlow (Tear Science), intense pulsed light (IPL), intraductal probing and debridement scaling of the lid margin.5 A recent paper demonstrated an increase in mean comfortable CL wear time of approximately four hours per day in patients with MGD with a single vectored thermal pulsation treatment.34 The most widely prescribed form of MGD management includes the application of warm compresses to the lids. However, studies show a wide variety of methods to apply heat to the eyelids, with no standard method recommended.27-31Because the methods used vary markedly in temperature achieved, care needs to be taken to ensure that the lids are appropriately warmed to obtain a therapeutic effect of >40°C.31-33 While several studies demonstrate the benefits of IPL, lid margin debridement scaling and device-assisted heating of the lids in the management of DED, to date there is a significant lack of studies investigating their use in the management of CLD, and more research is needed on this concept.5
 |
| MGD in a contact lens wearer with reduced CL comfort. |
Anti-inflammatories
Many studies confirm that DED is associated with an inflammatory process on the ocular surface, as evidenced by several review papers and acknowledged in the most recent DEWS II definition of DED.35-40 Of note, one study proposes that CL wear actually induces a low-grade inflammation through the presence of the lens.41 The management and therapy report describes several ways to manage this localized inflammation, including a wide variety of topical and systemic medications.5 While the use of multiple types of anti-inflammatory drugs are reported in the management of corneal infiltrates, microbial keratitis, corneal abrasions and various types of ocular surface disease and in cases of CL-induced disease (sometimes with the concurrent use of bandage lenses), few studies have been published that have investigated the impact of anti-inflammatory drugs on CLD. The use of cyclosporine 0.05% emulsion in the management of CLD was proven to be successful in one study but ineffective in another.42,43 One study did show that a four-week treatment with topical azithromycin ophthalmic solution was well tolerated and resulted in a significant improvement in comfortable CL wear time in patients with CLD.44
Dietary modifications
Much data now exists on the role of increased water intake, reduced caffeine and other dietary modifications that can impact DED.5 Of these, the greatest amount of data exists on the beneficial role of essential fatty acids, most notably the appropriate balance of omega-3 and omega-6 intake.5,38,45-49 Essential fatty acids have a broad range of systemic anti-inflammatory effects, including inhibiting the production of several pro-inflammatory cytokines—such as interleukin (IL)-1, IL-2 and tumor necrosis factor alpha—and preventing T-lymphocyte proliferation, which have been implicated in the pathogenesis of DED.5 In addition, they have beneficial effects on meibomian gland lipids.5,50 Several studies have demonstrated the benefit of appropriate dietary supplement intake on enhancing CL comfort in patients with dryness symptoms.51-54
The TFOS DEWS II management and therapy report makes it clear that management of ocular surface disease is of great value in the battle to reduce symptoms and signs of CLD. As such, practitioners need to look beyond lens material and care regimen. A careful assessment of the ocular surface could lead to increased CL success and reduced CL dropout rates.
Dr. Jones is a university research chair and professor at the University of Waterloo School of Optometry & Vision Science and director of the Centre for Ocular Research & Education.
1. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93-9. |


