| Abstract This case report illustrates how silicone hydrogel cosmetic lenses can improve the appearance of disfigured eyes while also providing the benefits of disposability, low cost and alleviation of any ocular hypoxia from low Dk hydrogel lens wear. Following the report is a discussion of the treatment’s success and the additional advantages it provides. Keywords: Disfigured eyes, prosthetic lenses, silicone hydrogel, cosmetic contact lenses, ocular hypoxia Introduction Prosthetic contact lenses can improve the appearance of a disfigured eye, whether due to disease, trauma, or congenital disfigurement or defect. However, they also come with some disadvantages, including non-disposability, relatively high cost and the lack of silicone hydrogel material. Clinicians can often overcome these disadvantages by prescribing silicone hydrogel color contact lenses. These contact lenses, normally used to change eye color, can aid disfigured eye appearance with the convenience of disposability without inducing ocular hypoxia. |
History
A 54-year-old female presented without complaints with a history of a perforating corneal infection 18 years earlier in the left eye, which resulted in a cataract extraction with intraocular lens (IOL) implantation, iris reconstruction and penetrating keratoplasty (PK). She habitually wore Freshlook Colorblends contact lenses (Alcon) and used OTC readers for deskwork, but did not own any prescription glasses. Systemic health history was noncontributory, and she denied taking any regular medication. She reported an allergy to Methiolate (thimerosal, Eli Lilly).
Diagnostic Data
The patient’s extraocular motilities and automated screening visual fields were full. No afferent pupillary defect was noted and color vision was normal. Intraocular pressures with noncontact tonometry were 16mm Hg OD and 18mm Hg OS. Automated keratometry was 44.00 at 156/45.00 at 066 OD and 44.00 at 085/47.25 at 175 OS. Manifest refraction was -9.75 -0.50x150 OD yielding 20/20 and -1.25 -3.25x099 OS yielding 20/25+. Accommodative testing yielded a +2.25 near add.
Biomicroscopy showed normal lids and lashes, with moderate conjunctival hyperemia in each eye. The right cornea was unremarkable, while her left cornea showed a clear penetrating corneal graft. Anterior chambers were free of inflammation. Her right iris was normal, but her left iris showed previous traumatic damage with suture loop (Figure 1). The right crystalline lens was clear. A posterior chamber IOL implant in the left eye was centered and free of capsular opacification. Funduscopy showed healthy optic nerves with cup-to-disc ratios of 0.3 and 0.4 with normal maculae, vasculature and retinal peripheries.
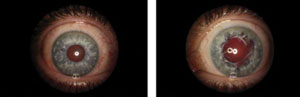 |
| Fig. 1. Generalized conjunctival hyperemia in both eyes after removal of hydrogel cosmetic contact lenses, revealing iris trauma in the left eye with a suture loop. |
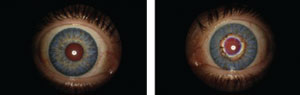 |
| Fig. 2. Improved cosmetic appearance with silicone hydrogel colored contact lenses. |
My clinical impression was status-post PK OS, pseudophakia OS and anisometropia. Due to generalized conjunctival hyperemia, I re-prescribed the patient silicone hydrogel colored contact lenses (Air Optix Colors, Alcon), moving her from a relatively low-Dk hydrogel material, phemfilcon A (Dk/t: 20 at -3.00D) to a higher one in lotrafilcon B (Dk/t: 138 @ -3.00D).1
The lenses had 8.6 base curve and 14.2mm diameter OU with -8.00 DS OD yielding 20/25 and -2.00 DS OS yielding 20/80. Spherical over-refraction was -0.75 DS OD yielding 20/20- and spherical-cylindrical over-refraction was PL-2.25x090 OS yielding 20/25. The patient understood the right lens power was at the parameter limit of -8.00 and that there was residual astigmatism in the left eye.
Progress Visit
At a subsequent progress visit, the patient reported a significant reduction in the conjunctival hyperemia and improved comfort. She was also pleased with the cosmetic concealment of the iris disfigurement (Figure 2). The contact lens prescription was finalized with no further changes and near-variable focus spectacle lenses were prescribed for use over the contacts.
Discussion
Prosthetic contact lenses can improve cosmetic appearance of disfigured eyes, social relationships and quality of life.2,3 Hand-painted lenses are a common treatment option for these patients. My patient, who had previously received a hand-painted prosthetic lens for the left eye, said she didn’t wear it because she felt it did not sufficiently match the appearance of her right eye.
In addition to the potential for mismatching, their lack of reproducibility, disposability and availability in silicone hydrogel materials are all drawbacks, further compounded by relatively high cost.
Commercially available silicone hydrogel colored contact lenses can overcome most, if not all, of these drawbacks. The higher Dk silicone hydrogel material can minimize complications from ocular hypoxia. Research shows a reduction in conjunctival hyperemia when patients move from hydrogel to silicone hydrogel lenses—which was certainly the case for this patient.4 Although she did not demonstrate corneal neovascularization from hypoxia, silicone hydrogel lens wear is preferable to hydrogel lens wear to reduce the risk of neovascularization, which is associated with an increased risk of corneal allograft rejection.5
The patient was pleased with her visual outcome, in part because I set realistic expectations prior to re-prescribing, including awareness that the goal was not a perfect cosmetic match but a general improvement. In the same manner that oculoplastic surgeons typically perform blepharoplasty bilaterally even when the patient complains of unilateral blepharochalsis, a better cosmetic outcome likely results from prescribing the same colored contact lenses bilaterally. Of course, if the patient is functionally monocular, it is appropriate to counsel the patient about the risk of microbial keratitis in the good eye. If the patient consents to bilateral contact lens wear, he or she should be reminded of the necessity of minimizing the risk of infection, including hand washing, proper disinfection and daily lens removal.6
In addition to the cosmetic benefit and reduction of ametropia, the patient felt there was reduction of her light sensitivity, likely attributable to the color print of her new contact lenses blocking light that would otherwise enter the enlarged and irregular pupil—and she wasn’t the first patient of mine with this benefit. Two other patients complaining of glare following laser peripheral iridotomies found some relief when wearing silicone hydrogel colored contact lenses. Research shows exposed and partially exposed iridotomies are more frequently associated with glare-type symptoms than iridotomies covered by the superior lid.7 These experiences suggest that colored contact lenses may bring functional benefit by blocking out light for patients complaining of glare after iridotomy.
To be sure, colored contact lenses are not suitable for all patients with disfigured eyes, and prosthetic contact lenses will continue to play an important role. But some patients are happy with the cosmetic improvement provided by silicone hydrogel colored contact lenses—not to mention their disposability, silicone hydrogel materials and relatively low cost.
Dr. Chou is a partner at EyeLux Optometry in San Diego, CA, where he directs a referral-based keratoconus clinic.
1. Alcon. Air Optix Brand Contact Lenses US Lens Parameter Guide. November 2016. Available at www.myalcon.com/docs/contact_lens_parameter_guide.pdf.
2. Cole CJ, Vogt U. Medical uses of cosmetic colored contact lenses. Eye Contact Lens. 2006 Jul;32(4):203-6.
3. Yildirim N, Basmak H, Sahin A. Prosthetic contact lenses: adventure or miracle. Eye Contact Lens. 2006 Mar;32(2):102-3.
4. Dumbleton K, Keir N, Moezzi A, et al. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci. 2006 Oct;83(10):758-68.
5. Perera C, Jhanji V, Vaipayee RB. Factors influencing outcomes of the treatment of allograft corneal rejection. Am J. Ophthalmol. 2011 Sep;152(3):358-63.
6. Lim CH, Carnt NA, Farook M, et al. Risk factors for contact lens-related microbial keratitis in Singapore. Eye (Lond). 2016 Mar;30(3):447-55.
7. Spaeth GL, Idowu O, Seligsohn A, et al. The effects of iridotomy size and position on symptoms following laser peripheral iridotomy. J. Glaucoma. 2005 Oct;14(5):364-67.


