ABSTRACT Keywords: Pinguecula, pingueculitis, scleral lens, contact lenses, keratoconus Introduction Scleral contact lenses have gained popularity as an effective treatment to restore vision in keratoconus and other thinning disorders, including in patients who have previously failed in traditional corneal gas permeable (GP) and hybrid contact lenses.3,4 Patients wearing scleral lenses often report excellent comfort, most likely because the lenses vault the sensitive cornea and rest on the relatively insensitive conjunctiva and underlying sclera.3,5,6 A common challenge to successful scleral lens wear is the presence of a pinguecula on the conjunctiva, which may mechanically interact with the landing area of the lens, causing redness and discomfort.7,8 In one study, nearly half of the population had a pinguecula.9 While the elective contact lens wearer can discontinue contact lens wear and use glasses, most patients with keratoconus require the functional vision that only rigid-surface contact lenses can provide. The prospect of excellent vision at the cost of eye redness and discomfort is not acceptable—nor is poor vision with a comfortable, white eye. However, keratoconus patients with pingueculitis due to scleral contact lens wear can often remain in this modality with appropriate lens modification. |
A 39-year-old Caucasian male presented on referral for keratoconus care after relocating from another city. He reported wearing a contact lens (SynergEyes ClearKone) only in the right eye. He indicated an inability to tolerate wearing any contact lens in his left eye, including a corneal rigid lens, piggyback system with a corneal rigid lens and various hybrid contact lenses. He did not use any eyeglasses. Family ocular history was unremarkable, he denied taking any regular medication and had no known drug allergies. He had no previous ocular surgery, and general health was unremarkable.
Diagnostic Data
Unaided visual acuity was 20/100 OD and 20/400 OS. Autorefraction yielded readings of -2.50 -5.25X066 OD and no obtainable measurement OS. Manifest refraction was -2.50-6.00X065 OD yielding 20/30, and gave no improvement OS. Corneal topography showed asymmetric corneal steepening OU, with significant irregularity, especially OS (Figure 1).
Contact lens evaluation of his SynergEyes ClearKone lenses OU was performed, including assessment of his left lens, which he did not wear due to discomfort. High molecular weight fluorescein was applied and showed an optimal fluorescein pattern OD with good centration and approximately 150 microns of central vault, and an alignment relationship over the inner landing zone (ILZ). The fluorescein pattern OS showed hard apical bearing with inferior decentration, with an alignment relationship over the ILZ and no skirt fluting. Contact lens acuity was 20/25 OD with spherocylindrical overrefraction of +0.75-0.75X140 yielding 20/20, and 20/25 OS with spherical overrefraction of -0.50 DS yielding 20/25+.
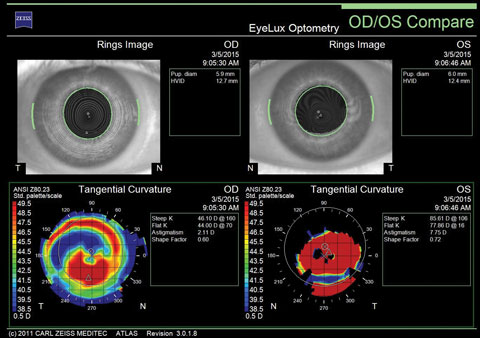 |
| Fig. 1. Topography showing corneal irregularity, more in the left than right eye. |
Biomicroscopy revealed that lids and lashes were normal, while the conjunctiva and sclera were unremarkable with no obvious conjunctival elevations. The right cornea showed iron deposition (Fleischer’s ring) and no apical scarring. The left cornea also showed a Fleischer’s ring, grade 2+ apical scarring and vertical folds at the level of Descemet’s (Vogt’s striae). Anterior chambers were deep and quiet, and the irides were healthy with normal anatomy.
Dilated examination was performed using a 78D condensing lens and biomicroscope, and using a 20D condensing lens with binocular indirect ophthalmoscopy. Crystalline lenses were clear, and anterior vitreous showed no liquefaction. Optic nerves were healthy with full neuroretinal rim tissue with C/D ratios of 0.2. Retinal vasculature, maculae and retinal peripheries were normal as well.
Diagnosis
I diagnosed keratoconus OS > OD with contact lens discomfort OS attributable to the pronounced corneal distortion causing mechanical interaction with the hybrid lens.
Treatment
I did not prescribe glasses because the patient rejected the manifest refraction when in a trial frame. I conveyed information about the eye disease, including how significant progression was unlikely at his age, as keratoconus is known to arrest on its own by the third to fourth decade of life.10
I recommended prescribing scleral contact lenses for both eyes and he scheduled a diagnostic fitting visit.
When he returned for diagnostic lens fitting, I started with Jupiter scleral lenses (Visionary Optics). The following initial lenses were applied with fluorescein (NaFl):
OD: 7.50mm base curve, -5.00D power, 18.2mm diameter, standard peripheral system.
OS: 6.25mm base curve, -14.00D power, 18.2mm diameter, standard peripheral system.
The NaFl pattern OD showed excessive central bearing. Over-refraction was not performed. OS showed optimal fitting characteristics with good centration and approximately 250 micron central clearance extending toward the limbus and a scleral landing zone without any noted vascular blanching or edge lift. Spherical overrefraction OS was +1.00DS yielding 20/25.
A new right diagnostic lens with greater sagittal depth was applied with 7.18mm base curve, -7.00D power, 18.2mm diameter and standard peripheral system.
This lens showed an optimal NaFl pattern with slight inferotemporal decentration, approximately 250 microns of central clearance and light superonasal touch in the corneal periphery. The scleral landing zone appeared ideal without vasculature blanching or edge lift. Spherical over-refraction was -0.25DS yielding 20/25+.
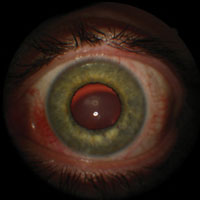 |
| Fig. 2. Left eye after removal of 18.2mm diameter scleral lens showing conjunctival injection, especially nasally surrounding pingueculum, and also Charleux’s sign with retroillumination. |
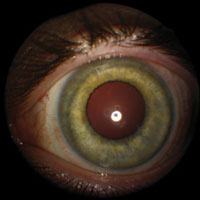 |
| Fig. 3. Left eye showing resolution of pingueculitis after the patient was prescribed the new 16.5mm diameter scleral lens. |
The final scleral lenses had the following parameters:
OD: 7.18mm base curve, -7.25D power, 18.2mm diameter, standard peripheral system, Boston XO Clear with drill dot.
OS: 6.25mm base curve, -13.00D power, 18.2mm diameter, standard peripheral system, Boston XO Clear.
Dispensing and Training Visit
Roughly two weeks later, I dispensed the scleral lenses and trained him on proper application, removal and lens care.
Contact lens acuity was 20/25+ with a spherical overrefraction of plano DS in each eye. A cursory evaluation using biomicroscopy showed a contact lens fitting relationship consistent with what I expected from the previous visit without air bubbles OU. He was cleared to wear his new contact lenses up to full waking hours, if well tolerated, and asked to return for a contact lens progress visit in one to two weeks.
Progress Visits
A week and a half later, he returned reporting that both new lenses performed well with excellent vision. Comfort in the right eye was excellent, and comfort in the left eye had improved by 90% compared with his previous experiences with other modalities. He noted that there was some tolerable redness and soreness in the left eye, especially by the end of the day. Wearing time at this visit was four hours.
Contact lens acuity was 20/25+ with a spherical overrefraction of plano DS in each eye. Fluorescein evaluation of the right lens showed slight inferotemporal decentration but an otherwise optimal fitting relationship with approximately 250 microns of central clearance and relatively even post-lens tear film distribution, but light superonasal peripheral touch. The left lens showed centration with approximately 250 microns of central clearance with a relatively even post-lens tear film extending toward the limbus, but mild peripheral vascular blanching at the nasal scleral landing zone. A new left lens was ordered with identical parameters except the scleral landing curve was changed from 14.50/0.5 to 15.50/0.5.
When he returned to exchange his existing OS scleral lens for the new lens, visual acuity in the eye was 20/25+ with a plano overrefraction. The new lens showed an improved fitting relationship with reduced nasal peripheral vascular blanching. There was no noticeable decrease in the central clearance. The patient was asked to report back within two weeks in the event there were any bothersome symptoms, but otherwise to return for routine examination in 12 months.
Annual Examination with Contact Lens Evaluation
When he presented the next year for his routine examination, he reported doing overall quite well wearing scleral contact lenses. However, he noted in the past one to two months the nasal conjunctival area of his left eye was red and sore. He stated that it was mostly a cosmetic issue and that on some occasions he would only wear the right scleral lens. Personal health history was unchanged with no regular medication and no known medication allergies.
Contact lens acuity was 20/25 OD with an overrefraction of -0.50D giving 20/25+, and 20/25+ OS with a plano overrefraction OS.
Biomicroscopy showed no changes to the right eye from the previous examination. However, the left eye showed an area nasally of raised and injected conjunctival tissue, which was interacting with the scleral lens edge (Figure 2).
Another Diagnosis
I diagnosed pingueculitis in the left eye related to mechanical interaction with the nasal edge of the scleral contact lens.
He was scheduled to return for diagnostic contact lens prescribing into a smaller diameter lens in the left eye.
Treatment
When he returned for diagnostic fitting into new scleral lenses, the primary goal was to prescribe a smaller diameter lens in the left eye to reduce the amount of mechanical interaction against the small nasal pinguecula. The new lens design selected for the left eye was the 16.5mm diameter ICD scleral lens (Paragon Vision Sciences), as this diagnostic set was available in the office. Concurrently, I re-prescribed the right lens from the Jupiter design into the Europa design (Visionary Optics) which, according to the manufacturer, is an improved design with a larger optic zone, reverse geometry mid-peripheral reverse curve and an enhanced haptic profile.11
First diagnostic lenses (Europa design OD, ICD design OS):
OD: 7.18mm base curve, -2.50D power, 18.0mm diameter, standard peripheral system.
OS: 6.88mm base curve, -5.00D power, 16.5mm diameter, standard peripheral system, 4500 sag.
The right lens showed slight inferotemporal decentration with approximately 250 microns of central clearance with some light superonasal peripheral thinning of the post-lens tear film. The scleral landing zone was optimal. Spherical over-refraction OD was -5.50DS yielding 20/25+. The left lens showed centration and moderate central apical bearing. Due to the lack of central clearance, the following diagnostic lens with 300 microns of additional sagittal depth was then applied:
OS: 6.62mm base curve, -8.00D power, 16.5mm diameter, standard peripheral system, sag: 4800 sag.
This new left lens was centered with approximately 150 microns of central clearance and a relatively even post-lens tear film extending toward the limbus, with an ideal scleral landing relationship. Spherical overrefraction OS was -2.25 yielding 20/25.
The following contact lenses were ordered (Europa OD, ICD OS):
OD: 7.18mm base curve, -7.75D power, 18.0mm diameter, standard peripheral system, Boston XO Clear.
OS: 6.62mm base curve, -10.25D power, 16.5mm diameter, standard peripheral system, 4800 sag, HDS100 Blue.
When he returned for dispensing of his new scleral lenses, subjectively he reported excellent vision and felt that the smaller left lens was already more comfortable.
Visual acuity was 20/25+ OD with a spherical overrefraction of plano DS and 20/25 OS with a spherical overrefraction of +0.50 OS yielding 20/25. Biomicroscopy showed centered lenses with the left lens edge sparing mechanical interaction with the nasal pinguecula. Fluorescein evaluation was not performed. He was asked to return in one week for a contact lens progress visit, and to come in wearing his new scleral contacts for at least an hour.
Progress Visit
When he returned for his contact lens progress visit, he had been wearing his lenses for three hours and reporting that he was pleased with the new scleral lenses. He estimated that the redness and discomfort in the left eye had resolved by 98% with the smaller diameter scleral lens. For the right eye, there was no appreciable subjective difference in his wearing experience with the new design. Subjective vision was excellent in both eyes, with comfortable wear for full waking hours.
Contact lens visual acuity was 20/25+ OD with spherical overrefraction of plano DS, and 20/25 OS with spherical overrefraction of +0.50 OS yielding 20/25+.
Biomicroscopy showed the left bulbar conjunctiva had significantly reduced injection and the inflamed nasal pinguecula had subsided in size (Figure 3). There was no significant corneal staining.
Fluorescein evaluation with the right scleral lens showed approximately 250 microns of central clearance with a relatively even post-lens tear film extending to the limbal clearance zone. The scleral landing zone was optimal. The left lens showed approximately 150 microns of central clearance, also with an even post-lens tear film extending to the limbal clearance zone. The scleral landing zone was optimal as well.
A new left lens was ordered, accounting for the +0.50 overrefraction, and he was released to routine annual examination following the lens exchange.
Discussion
Pingueculae are the most common conjunctival lesion, occurring in 48% of patients.9 They can mechanically interact with the landing zone of a scleral contact lens, leading to redness and discomfort.7,8
Although prescribing topical corticosteroid therapy would quell the inflammatory component of pingueculitis, it would not eliminate the underlying mechanical interaction against the conjunctival elevation and could require chronic dosing. The risk of chronic corticosteroid therapy, even with the ester-based corticosteroid loteprednol, is the potential for cataract formation and increased IOP.12 For this reason, although suitable as a periodic adjunct, a more sensible approach is modifying the lens to address the root cause of scleral lens–induced pingueculitis.
 |
| Fig. 4. Just like scleral lenses with an edge notch, MicroVault lenses require lens application with rotational registration such that the MicroVault aligns with the conjunctival elevation. Photo: Alden Optical. |
A review of the literature describes lens-based modifications, such as adding an edge notch on the scleral lens to resolve the problems with pingueculae.7,8,14 However, because these edge notches are introduced using a hand tool, there is variability with lens reproducibility. MicroVaults (Alden Optical)—designed and manufactured with CAD/CAM technology—may overcome the problems of reproducibility found with traditional hand-notching, according to the manufacturer. (Figure 4).15 With both hand-notched lenses and MicroVaults, the patient must apply the notches in the proper orientation to correspond with the location of the pinguecula.
Finally, although not the case with this patient, hybrid lenses may afford resolution of the mechanical interaction on the pinguecula due to draping of the soft skirt over the conjunctival elevation.
As illustrated by this case report, ordering a smaller diameter scleral lens was a simple and effective treatment for this patient’s pingueculitis, particularly because it was peripherally located. The benefit of decreasing lens diameter is that it is simple, can minimize further cost to the patient, and removes the burden of applying the lens with the notch or MicroVault in the same location of the pinguecula. While decreasing diameter may seem an intuitive solution, interestingly, another purported strategy is to prescribe an even larger diameter scleral lens to compress the pinguecula.13
Scleral contact lenses are very well tolerated by most patients with keratoconus due to good comfort and vision, especially when compared to corneal gas permeables and other types of contact lenses.6 The high rate of success of scleral lenses should remind clinicians to educate those with keratoconus about the importance of ultraviolet (UV) light protection to minimize the risk of developing pingueculae. Although the aforementioned modifications to scleral lenses can help patients with pingueculae to remain in scleral lens wear, it is best if patients never develop these conjunctival lesions in the first place. Although UV light may have a therapeutic effect in mitigating keratoconus progression by facilitating collagen crosslinking, it is likely outweighed by the risks of UV exposure, including certain eyelid growths, pingueculae, pterygia, cataract and retinal damage.16
Scleral contact lenses are well tolerated by most keratoconus patients, but conjunctival lesions, including pingueculae, can pose an obstacle to success. For some patients, reducing the lens diameter to eliminate or reduce interaction of the lens edge with the conjunctival lesion—especially if the lesion is located peripherally—is the simplest treatment option. Conversely, for others with pingueculae, enlarging the scleral lens diameter to deliberately compress the conjunctival elevation may help. If these treatments are unsatisfactory, edge notching and MicroVaults are the next logical step, which involves greater complexity due to additional position specification of these lens modifications.
Dr. Chou is a partner at EyeLux Optometry in San Diego, CA, where he directs a referral-based keratoconus clinic.
1. Alió JL, Shabayek MH. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg. 2006;22(6):539-45.2. Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30(12):1510-6.
3. Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens. 2010;36(1):39-44.
4. Van der Worp E, Bornman D, Ferreira DL, et al. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014;37(4):240-50.
5. Visser ES, Visser R, van Lier HJ, et al. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007;31(1):21-5.
6. Bergmanson JPG, Walker MK, Johnson LA. Assessing scleral contact lens satisfaction in a keratoconus population. Optom Vis Sci. 2016;93(8[Epub ahead of print].
7. Messer M. Getting creative with scleral lenses: Part 1. Review of Cornea & Contact Lenses. 2012;148(1):7.
8. Denaeyer GW. Designing lenses to work around scleral obstacles. Contact Lens Spectrum. August 2012. Available at www.clspectrum.com/articleviewer.aspx?articleID=107286. Accessed May 24, 2016.
9. Viso E, Gude F, Rodríguez-Ares MT. Prevalence of pinguecula and pterygium in a general population in Spain. Eye (Lond). 2011;25(3):350-7.
10. Rabinowitz YS. Keratoconus. Surv. of Ophthalmol. 1998;42:297–319.
11. Visionary Optics. Europa Scleral Overview. Available at www.visionary-optics.com/products/scleral-lens-for-irregular-corneas/europa-scleral. Accessed May 30, 2026.
12. Comston TL, DeCory HH. Advances in corticosteroid therapy for ocular inflammation: loteprednol etabonate. Int J Inflam. 2012;2012:789623.
13. Barnett M. Case study: scleral lenses post glaucoma surgery. Optometric Management. December 1, 2014. Available at www.optometricmanagement.com/articleviewer.aspx?articleID=112072. Accessed May 24, 2016.
14. Messer B. Utilizing MicroVaults to improve comfort and cosmesis in scleral lens wearers with pingueculae. Poster. Available at www.aldenoptical.com/docs/zenlens/Zenlens_Poster.pdf. Accessed May 24, 2016.
15. Van der Worp E. A guide to scleral lens fitting, Version 2.0 [monograph online]. Forest Grove, OR: Pacific University; 2015:51. Available from: http://commons.pacificu.edu/mono/10/.
16. Behar-Cohen F, Baillet G, de Ayguavives T, et al. Ultraviolet damage to the eye revisited: eye-sun protection factor (E-SPF®), a new ultraviolet protection label for eyewear. Clin Ophthalmol. 2014;8:87-104.


