Corneal Thickness May Help Predict CXL Outcomes
Researchers recently examined how preoperative characteristics impact the outcomes of corneal collagen crosslinking (CXL) in pediatric patients and found that the thinnest baseline corneal thickness impacts the success rate of CXL after two-year follow up.1
“Keratoconus has potentially devastating effects on our patients’ quality of life,” says Barry Eiden, OD, co-founder and president of the International Keratoconus Academy. “Younger individuals (<18) who develop keratoconus have been shown to progress faster and develop more advanced disease with a higher rate requiring corneal transplantation.”
Research shows that collagen crosslinking can slow down or halt the progression of the degenerative disorder and, when successful, CXL may stabilize keratoconus while leading to a permanent flattening of the cornea—a result that potentially saves individuals from progressive vision loss or risky corneal transplants in the future. This study help to further identify the particular characteristics of patients who will more likely be successful candidates for this leading-edge procedure.
The study included 72 eyes of 52 patients with keratoconus. The subjects were all under the age of 18 with a two-year follow up after CXL. Researchers analyzed subgroups determined by age, sex, baseline uncorrected and corrected distance visual acuities (UCVA, CDVA), topographic cone location (central and paracentral), maximum keratometry (k-max) and corneal thickness at the thinnest point (thCT).
Results of the study show that two years after CXL, the mean UCVA improved considerably, while the mean thCT decreased significantly in all patients. The k-max in patients with paracentral cones and/or a thCT of less than 450µm was more likely to progress. The other characteristics did not present any notable effect on the progression of CXL after treatment.
“The challenge,” says Dr. Eiden, “is for us to develop metrics that reliably indicate keratoconus stability vs. progression. In this study, progression was defined as a steepening of the maximum anterior corneal curvature value (>1D) within 3mm of the apex of the cone (k-max). Other studies suggest alternative measures that may be more reliable indicators.”2
While the efficacy and safety of CXL in pediatric and adult patients have been thoroughly demonstrated, this study sheds light on factors that help predict successful outcomes for pediatric patients undergoing crosslinking. “Further research surely is needed,” suggests Dr. Eiden. “However, the take-home message continues to be the importance of early diagnosis of keratoconus and implementation of treatment methods to hopefully halt the progression of the disease prior to its significant impact on visual function.”
1. Sarac O, Caglayan M, Cakmak HB, Cagil N. Factors influencing progression of keratoconus 2 years after corneal collagen cross-linking in pediatric patients. Cornea. 2016. EPub ahead of print.
2. Duncan JK, Belin MW, Borgstrom M. Assessing progression of keratoconus: novel tomographic determinants. Eye and Vision. 2016 Mar;3(6).
| In Brief |
| Dry eye symptoms and body fat may be correlated, a new prospective study suggests. Researchers sampled ocular symptoms and indices of adiposity in the general adult population and in the 305 participants, including 53 contact lens wearers. Results show a moderate correlation between body fat percentage and dry eye symptoms. Chronic inflammation may be the link. “Adipose tissue contributes to a rise in circulating levels of many proinflammatory mediators,” the researchers state. Ho KC, Jalbert I, Watt K, Golebiowski B. A possible association between dry eye symptoms and body fat: a prospective, cross-sectional preliminary study. Eye & Contact Lens. 2016. EPub ahead of print. Keratitis infections appear to be more common in the summer, according to a new study. Researchers performed a retrospective chart review on patients presenting to the emergency department who were diagnosed with infectious keratitis from 2008 to 2013. Looking at data from 155 patients diagnosed with keratitis, researchers found that 12.3% of patients with ulcers presented in the fall, 21.3% in the spring, 21.9% in the winter and 44.5% in the summer—indicating a higher frequency of infectious keratitis and P. aeruginosa positivity during the summer months. Researchers posit that possible factors for this include warmer temperatures, higher levels of humidity and increased ocular exposure to water. Gorski M, Genis A, Yushvayev S, et al. Seasonal variation in the presentation of infectious keratitis. Eye & Contact Lens. 2016 Sep;(42(5):295-7. Researchers recently developed and evaluated a new meibomian gland dysfunction (MGD)-specific questionnaire based on accepted tests such as the Schein symptom survey, tear break-up time, corneal and conjunctival staining, abnormal meibum or meibomian gland atrophy and a normal Schirmer test. The MGD questionnaire initially contained 24 items targeting the intensity and frequency of 12 symptoms. Using data from the 69 MGD subjects who completed the survey and clinical testing, researchers worked through three iterations of analysis of subject responses to the tests. The final questionnaire included seven question pairs. Researchers conclude that the study is a valid and quantitative measure of symptoms common for patients with MGD. They acknowledge that further research is needed to determine whether the diagnostic efficacy is an adequate means of differentiating MGD dry eye subtypes in an independent sample of normal subjects. Paugh JR, Kwan J, Christensen M, et al. Development of a meibomian gland dysfuntion—specific symptom questionnaire. Eye & Contact Lens. |
New Stats Highlight the Need for More DED Education
Nearly 90% of eye care providers (ECPs) believe there is no representative type of dry eye disease (DED) patient, according to the National Eye C.A.R.E. (Current Attitudes Related to Eye Health) Survey. The online survey included more than 1,000 optometrists and ophthalmologists, as well as more than 1,200 adults who had been diagnosed with DED or experienced dry eye symptoms and used artificial tears within the past month. Results provide new statistics on many aspects of dry eye care, including:
Patient demographics
76% said they see more patients aged 18 to 34 with DED symptoms than 10 years ago.
89% of ECPs believe DED is on the rise due to multi-screen digital device use.
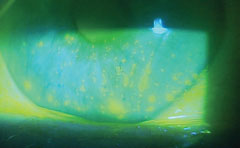 |
| Dry eye is on the rise, according to a new study, and prolonged digital device use might be to blame. Photo: Paul M. Karpecki, OD. |
Screening
94% said DED screening should be part of the comprehensive eye exam.
75% believe it’s necessary to screen for dry eye symptoms in all patients regardless of age, gender or lifestyle.
88% deem it important to screen women over 50.
Symptoms
79% of patients said their DED symptoms are currently under control.
52% said their symptoms are getting worse over time.
75% said dry eye impacts their digital device use and 64% said it impedes daily activities.
54% said DED symptoms impact their ability to work.
69% believe dry eye is something they have to live with.
The survey also revealed the need for more patient education, noting that 72% of ECPs said most patients aren’t familiar with DED. Patient responses are in accord with this finding, as 25% said they didn’t realize eye dryness is a symptom of a disease, and 32% said they didn’t know DED could cause long-term damage to their eyes.
Despite the well-known need for dry eye care, 72% of patients who participated in the survey said they initiated the DED conversation themselves. More telling, 45% of patients said they did not feel it was worth mentioning dry eye because the ECP did not ask about it.
Armed with these new statistics, ECPs are better equipped to address dry eye in every exam and help more patients find the relief they never knew they needed.
Shire Pharmaceuticals. The National Eye C.A.R.E. (Current Attitudes Related to Eye Health) Survey. September 2016. Available at www.myeyelove-ecp.com/dry-eye-info-from-peers. Accessed October 19, 2016.


