Most patients with keratoconus and other forms of corneal ectasia struggle to overcome visual aberrations induced by irregularity of the anterior corneal surface. Distortions induced by the irregular posterior corneal surface and visual limitations from corneal scar opacities within the visual axis in more advanced cases are other contributing factors. Contact lenses function predominantly to address these visual impairments in two ways: first, by correcting traditional refractive errors like myopia, hyperopia and astigmatism (also known as lower-order aberrations) and, second, by masking the irregularity of the anterior cornea to create a smoother and more regularly shaped anterior optical surface, which can significantly reduce the visual distortions known as higher-order aberrations.
| Spectacles Can Still Play a Role Above all, the primary goal for correcting vision in patients with keratoconus is to provide clear, functional vision. There are many cases in which spectacles—the most classical form of vision correction—provide excellent outcomes. One of the key diagnostic methods to achieve acceptable acuity with spectacles is to perform corneal topography and observe the power distribution within the pupillary zone. If that pattern is unremarkable in terms of its astigmatic profile, one can expect the manifest refraction to result in good quality visual acuity, assuming that other elements of the ocular system are normal. Patient success with spectacle wear in cases of keratoconus is limited by various factors of the disease, including adaptation to high astigmatism or significant anisometropia, and frequent changes in refractive results in cases of progressive keratoconus. Practitioners should keep in mind, however, that even in cases in which contact lenses provide better correction for patients with keratoconus, spectacles can still play a role, if only to allow for limited function when contact lenses are not actively being worn. All keratoconus patients should have a back-up pair of spectacles if possible. |
For the most part, though, current contact lenses do not address the residual distortion induced by irregularity of the posterior corneal surface. This article will review current contact lens options with emphasis on how to select the best modality in certain cases. The advantages and limitations of each will also be covered.
Corneal Gas Permeable Lenses
Rigid corneal contact lenses have been the gold standard of vision correction for keratoconus for over half a century. Though other options have been developed that address the vision needs of the keratoconic patient, these lenses still hold an important place in our contact lens armamentarium. Advantages include good visual rehabilitation via their ability to mask the anterior surface corneal irregularity, ease of handling, excellent tear exchange and oxygenation of the cornea, low rates of infectious keratitis and a decreased rate of inflammatory changes. Primary disadvantages include initial and ongoing discomfort and awareness by many patients, debris and foreign body accumulation under the lenses with associated discomfort and irritation, difficulty with centration of the optics in highly decentered cone apices and the inability of the lens to properly contour the corneal surface without corneal apical bearing in more advanced cases of the disease.
Considerations when evaluating corneal GPs for keratoconus include the location and size of cone, the shape and status of the peripheral cornea and the final visual needs of the patient. Due to highly suggestive evidence that lens bearing on the apex of the cone may increase the rate of scarring, apical bearing should be avoided as much as possible. We typically choose larger overall lens diameters for corneas with larger, decentered cones by first aligning the lens with the corneal periphery and then allowing for adequate tear exchange via appropriate peripheral edge clearance.
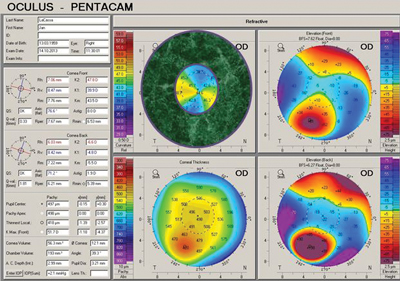 | |
| Fig. 1. Scheimpflug tomography demonstrating regular astigmatism within the pupillary zone of a patient with keratoconus. BCVA with manifest refraction was 20/20-. However, should the power distribution within the pupillary zone appear to be significantly irregular, one should expect reductions in best corrected manifest refraction acuity consistent with the degree of irregularity. | |
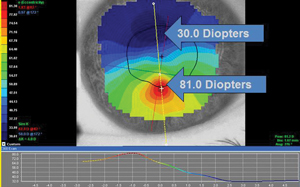 | |
| Fig. 2. Placido topography demonstrating highly irregular astigmatism and tremendous power distribution within the pupillary zone of a keratoconic patient. Best-corrected manifest refraction visual acuity was 20/60. |
Additionally, we need to address the visual needs of our keratoconic patients by not only masking the anterior corneal surface irregularity as completely as possible but also addressing residual astigmatism. Often, we see patients who present in their corneal GP lenses with limited acuity, only to find that a cylindrical overrefraction can improve acuity by a number of lines.
When prescribing corneal GPs for keratoconus, practitioners can either custom design a lens or use proprietary corneal GP designs specifically developed to address the topographic requirements of the keratoconic cornea. As a general guideline, we suggest the following for corneal GP design selection for keratoconus:
• When fitting small central cones (i.e., nipple types), use small-diameter multicurve designs with overall diameters of less than or equal to 9mm and optic zone diameters of less than or equal to 7mm.
• When fitting moderately sized and decentered oval cones, use moderate-diameter multicurve designs with overall diameters of 9mm to 11mm and optic zone diameters of 7.2mm to 9mm. Intermediate and peripheral curves can be spherical, aspheric or even toric if the peripheral cornea is regularly toric.
• When fitting large and highly decentered “globoid” and “pellucid-like” cones, use larger-diameter intralimbal designs with overall diameters of 11mm to 12.2mm (that typically measure 0.2mm less than the overall corneal diameter), along with larger optic zones (typically over 9mm). Patients wearing these designs can benefit most from asymmetric peripheral geometries, in which peripheral curvatures can be varied along different quadrants or meridians.
Scleral Gas Permeable Contact Lenses
With the advent of highly oxygen permeable gas permeable lens materials, scleral lenses have gained significant popularity over the past decade. The general goal when fitting a scleral lens to virtually any eye—irregular cornea or not—is to completely vault the cornea and land on the bulbar conjunctival surface overlying the sclera. Avoidance of corneal bearing, especially in the limbal area, is critical for success. Additionally, peripheral landing should attempt to parallel the scleral surface without resulting in conjunctival impingement/compression or significant peripheral scleral lens lift or standoff.
When appropriately fit, these specialty lenses provide excellent visual performance and comfort independent of the degree of corneal astigmatism. Scleral lenses can be designed in a variety of sizes to accommodate a host of ocular shapes, and can be fabricated to include anterior surface optics that address residual astigmatism. Some are also available or are being developed in multifocal designs or to address residual higher-order aberrations.
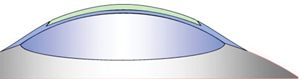 | |
| Fig. 3. Model of a recessed pillow lens system. Photo: Robert Davis, OD | |
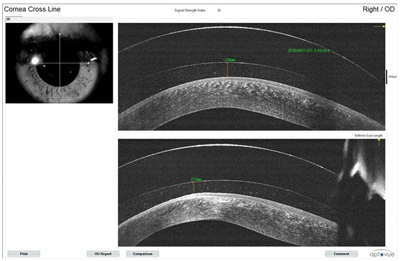 | |
| Fig. 4. An anterior segment optical coherence tomography scan of a scleral contact lens on the eye. |
Scleral lenses, however, are not a panacea. There are concerns regarding the oxygen transmission properties of these typically thick lenses, as they are fit with significant corneal vault and minimal tear exchange. We are still not certain what long-term physiological implications could be identified after years of wear on diseased eyes, especially on those patients with compromised corneal endothelial function, such as those who have undergone penetrating keratoplasty.
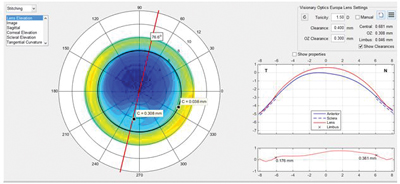
The scleral lens fitting process has advanced tremendously over the last few years, with the introduction of technologies like anterior segment OCT and various forms of corneo-scleral profile measurement instruments. The ability to “virtually” design scleral lenses without a required diagnostic lens evaluation and the capacity to measure their physical fitting characteristics immediately following dispensing has reached high levels of precision. When the degree of corneal and scleral surface irregularity is substantial enough to resist correction by even a vaulting scleral lens, an ocular prosthetic scleral device may be necessary. These are approximately the same size and fabricated from similar materials as scleral lenses, but are highly customized to address the unique and individual characteristics of more complex corneal cases. The Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) device by the Boston Foundation for Sight is one example; fitting this device involves the use of proprietary diagnostic lenses and a software program that measures the shape of the individual patient’s ocular surface.
Another example of a customizable ocular prosthetic device is the EyePrintPro by EyePrint Prosthetics, an optically clear prosthetic scleral cover shell that matches the contours of the eye to provide good vision and comfort. When creating this prosthetic, an impression is taken of the patient’s eye at the practitioner’s clinic, then shipped to EyePrint Prosthetics to be digitized by computerized topographical scanners. Using three-dimensional scanning technology and computer-controlled machining systems, an exact match is created to each individual cornea and sclera. In effect, instead of using a series of standardized curvatures to create the lens as is done with traditional scleral lenses, the EyePrintPro is generated to exactly match the unique irregularities of the individual eye. Because of the precise nature of the back surface fit, high quality and individualized optics such as toric corrections, multifocals, high-order aberration correction and prismatic powers can be placed on the front surface of the device.
 | |
| Fig. 5. A profile view of a scleral lens on the cornea. | |
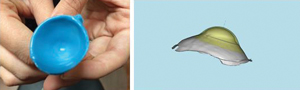 | |
| Fig. 6. EyePrintPro impression and computer simulation. |
Combining Soft and Rigid Materials
Patients and practitioners alike frequently prefer to combine the crisp optics of rigid lenses with the comfort of a hydrogel material. A number of interesting approaches allow us to do just that.
• Piggyback or Tandem Contact Lens Systems. This approach traditionally incorporates a corneal gas permeable lens over a soft lens. Advantages of this setup include improved initial and ongoing patient comfort as compared with direct corneal rigid lens wear, potential reduction of mechanical physical compromise to the ocular surface induced by the corneal rigid lens and possible improvement of GP lens centration for improved optics. The soft “carrier” portion of the system provides assistance with GP lens centration (especially if higher plus power soft lenses are used, which create a relatively central steeper element to the anterior ocular surface) and a barrier against direct contact between the rigid lens and the ocular surface.
The GP lens portion of the system, meanwhile, provides the necessary optical correction. Any design and optical configuration of GP lens can be used in piggyback/tandem lens systems; however, disadvantages include potential limitation of oxygen transmission through the system (depending upon lens material DK/t and thickness profiles) and the inherent difficulty or inconvenience of using such a system.
| Soft Lenses: Appropriate for Early to Modern Cases In the past, soft contact lenses had been considered inappropriate for management of keratoconus, as these lenses drape over the irregular corneal surface and conform to the anterior topography of the cornea. However, they may still have certain indications in keratoconic patients: advantages include initial and ongoing comfort, ease of handling and care as well as a tendency to maintain centration of the contact lens over the cornea and visual axis of the eye. Disadvantages include the limited potential for addressing distortion induced by irregular corneal optics, hypoxic sequelae and greater potential for infection and inflammation than rigid contact lenses. Traditional soft lens designs can be used in keratoconus when the best-corrected manifest refraction visual acuity is acceptable and the degree of secondary visual distortion is limited. Just as with spectacle lens considerations, examining the axial map in corneal topography can give the practitioner a good idea of the patient’s visual potential while wearing traditional soft lenses. Toric designs are often required due to the significant amount of astigmatism typically present in keratoconic patients; either planned replacement, disposable designs or conventional annual replacement designs can be used. Lenses made from materials that allow higher oxygen transmission like silicone hydrogels can be worn to reduce the likelihood of hypoxic sequelae, though non-silicone hydrogel materials have been used with success for many years without hypoxic complications when proper design and fitting strategies are considered. Additionally, giving special consideration to spherocylinder overrefraction (SCOR) with soft lenses is critically important for visual performance; as such, it is not unusual to achieve results from SCORs that are not predicted by the original refractive data or the toric rotation marks on the lenses due to the unpredicted draping effects over a keratoconic cornea. The key data to pay attention to, in this case, is the visual acuity outcome and visual stability found from the SCOR. If vision is acceptable and stable, results from SCOR can be incorporated into a design. When corneal irregularity is too high for traditional soft lens designs to provide acceptable vision quality, consider custom keratoconic soft lens designs. These lenses address corneal irregularity by thickening the optic zone to mask the condition. Central lens thickness values in these applications can vary from approximately 0.35mm to more than 0.60mm, depending on the degree of corneal surface irregularity. Note, hypoxic concerns due to increased lens thickness can be addressed with the following points in mind: • Fit these lenses with significant movement (i.e., up to 1mm with blink) to allow for tear exchange with oxygenated tears. • Limit lens thickness increases to the optic zone. Lenticularization can help keep peripheral portions of the lenses thin. This is critical, as oxygen transmission in the area of the highly sensitive limbal corneal stem cells is important for continued corneal health. • Some of these designs can be manufactured with higher oxygen transmission SiHy materials to offer added (albeit limited) benefit, and more designs will be available in this way over time. • Soft custom keratoconic lenses can also be designed with front surface toricity to address residual astigmatism. They may also have front surface aspheric optics that can minimize some of the residual higher-order spherical aberration found in keratoconic patients. • Finally, the centration tendencies of these lenses are often advantageous in providing stable, centered optics. In some cases, however, the visual axis is decentered from the corneal apex and, even in a well-centered lens, optical aberrations can be increased due to the mismatch of the visual and contact lens optics. Some custom design laboratories may be able to decenter the optic zone to address this issue. |
Today, the issue of corneal hypoxia has been largely addressed by the availability of multiple contact lens materials with high oxygen transmission properties. Additionally, use of frequent replacement soft lenses (especially daily disposable modalities) as the base carrier in these systems means practitioners can provide a more convenient and healthy option for piggyback/tandem lens wear as compared with options in the past (Table 1). In cases of corneal irregularity like keratoconus, the fitting characteristics of the soft lens may be influenced by the modulus of the material used. Higher modulus lenses may at times result in edge fluting with associated lens awareness or discomfort. As such, high Dk/low modulus lens designs are often preferred.
The fitting methods of these systems are typically quite simple and result in use of GP lenses with the same fitting and vision parameters as would be used when fitting the GP lens directly on the cornea. The exceptions to this would be cases in which high-power soft lenses are used to influence lens centration. It has been estimated that only 20% of the soft lens power manifests in a piggyback/tandem lens system; as such, since low power soft lenses are typically employed most, their influence on the total power of the system is quite insignificant.
In addition to the use of conventional disposable soft lenses as a carrier for the GP lens in piggyback/tandem lens systems, it is occasionally advantageous to consider custom soft lenses that have a recess or cut-out in the anterior surface in which the GP lens can be placed. Recessed soft lenses help better hold the GP lens in place for optimal centration; as such, in this case, the soft lens provides the system’s centration and movement, while the GP provides the optics. Examples of recessed or cut-out soft lenses include the Flexlens Piggyback (X-Cel) and the Recessed Pillow Lens System (Fusion Technologies and EyeVis Vision Research).
• Hybrid Contact Lenses. Based on the initial concept introduced by piggyback/tandem lens systems, hybrids are single lenses that combine the attributes and advantages of both soft lenses and rigid gas permeable lenses. The Saturn lens, introduced in 1984, was the first hybrid design; since then, various developments in hybrid lens technology have led to the contemporary version now manufactured and distributed by SynergEyes. Today’s hybrid lenses are fabricated from high oxygen transmission materials and constructed to avoid the fragility of the junction between the soft skirt and rigid center of former hybrid designs.
Along with advances in materials and manufacturing improvements, hybrid lens designs themselves have also moved forward, with more indications than ever. This includes their use on irregular corneas, with the most current lens being the UltraHealth lens (SynergEyes). The UltraHealth lens is a reverse geometry “vault” design configured to leap the apex of the keratoconic cornea. When appropriately fitted, the lens centers fairly well and maintains adequate movement during wearing time. It also provides acceptable comfort and good visual performance. An oblate design version of the lens, known as the UltraHealth FC, was also recently introduced. This reverse geometry design is most appropriate for corneas characterized by oblate topography, which is most commonly found in patients who have undergone refractive surgery or penetratingkeratoplasty. However, some practitioners have also used this design to successfully fit certain cases of keratoconus via incorporation of the more pronounced reverse curve as a way to “lift” the lens in order to achieve adequate apical vault.
| Table 1. Soft Lenses Typically Used in Piggyback/Tandem Contact Lens Systems | |||
| Design | Dk/t | Modulus (MPa) | Replacement Frequency |
| Night & Day | 175 | 1.50 | Monthly |
| Acuvue Oasys | 147 | 0.2 | Two-Week |
| Biofinity | 160 | 0.75 | Monthly |
| Ultra | 163 | 0.70 | Monthly |
| Dailies Total 1 | 151 | 0.70 | Daily |
| MyDay | 100 | 0.40 | Daily |
| AcuVue Oasys One-Day | 121 | 0.96 | Daily |
Contraindications for hybrid lens wear for keratoconic patients include scenarios in which appropriate physical fitting characteristics cannot be achieved and thus results in one or more of the following: apical bearing, lens landing areas with excessive bearing/compression or lack of movement either initially or after a period of wear. These issues are more commonly present when the cone is either too advanced in elevation or curvature and/or when the cone is significantly decentered. Thus a rule of thumb is that those cones that are mild to moderate and more centralized tend to respond much better to wear of vaulting hybrid contact lenses. Optical limitations can also present with hybrids when significant residual astigmatism is found due to the lack of availability of anterior toric options at this time, so this must also be kept in mind when evaluating a patient.
All in all, keratoconus is a challenging disease that presents in a wide range of severity and visual disturbances. A detailed understanding of the phenomenon and extensive clinical experience in its management allows the practitioner to tailor the most appropriate vision correction solution for each patient. Contact lenses have been and continue to be the mainstay for this patient population; fortunately, both old and new lens options abound. Integrating the most appropriate contact lens treatment with a comprehensive medical and surgical approach will allow the keratoconic patient to receive the highest quality of care, which should result in optimal vision along with appropriate control of the disease.


