When evaluating the pre-presbyopic contact lens patient, it’s best to educate them on future decisions they will need to make as their eyes change over the next few decades. Try not to fit a multifocal or monovision lens before the patient truly needs it in their world, as they won’t adapt as easily—let them tell you when they can’t see their phone screen anymore.
Which is Better: Monovision or Multifocal?
A diagnostic session in the office will usually point you in the right direction regarding whether to prescribe monovision or multifocal lenses. First, try overplussing the nondominant eye just enough for good near function—if this is successful, the patient is likely a good monovision candidate. However, if the patient feels dizzy or notices an imbalance or significant difference in vision clarity between eyes, multifocal lenses may be a better choice.
For patients not yet wearing contact lenses, especially hyperopic patients or new presbyopes, offering a pair of multifocals to be worn during dilation to allow for frame selection is a great way to demonstrate the positional independence of multifocal contact lenses. In other words, they can see up close in all viewing positions, not just in the reading position.
So, now that you have the patient’s attention, the fitting process for new multifocal and monovision patients starts with acquiring a thorough knowledge of their needs and desires:
- What are their visual priorities? Are they planning to wear the lenses full-time or only part-time?
- What daily activities could affect their lens preference?
- Are dry eyes or tear film abnormalities an issue?
- Is the patient a keen observer or more laid back concerning visual needs? Jewelers need excellent near vision; teachers probably don’t.
- How much astigmatism is there to be dealt with?
- How long do they use the computer or other electronic devices each day?
Stress to the patient that most—but not all—of their visual needs may be met, especially in cases of presbyopia after age 50, so they do not form unattainable expectations. For this reason, a “show and tell” using trial lenses is extremely valuable before proceeding with the full diagnostic fitting process, as you can discern the patient’s reaction to the new modality, and make minute adjustments after the initial adaptation. Emphasize to the patient that you are trying to find the best compromise for them. There is no perfect solution. In practice, most patients will achieve about 80% of their visual demands—and it is a process, with follow-up required.
As Keith Masnick, M.Optom., observed in the early days of multifocal contact lens fitting, “It doesn’t always make sense; the numbers don’t always work out as predicted.” Multifocal fitting is a highly pragmatic process. To be successful, the patient must first use the lenses.
A Tale of Four Patients
In this article, we will bypass the early, easy presbyopic fit. You know how to do that. But what about when a patient comes back one or two years later complaining their vision is blurry both up close and far away? Below are four sample cases. Although specific lenses are mentioned, the goal here is not to advocate for a particular lens but rather to walk through the process of problem solving. Many other products and approaches might work too—that’s the point. It all depends on what each patient responds to.
• Case 1: Modified Monovision. Many, if not most, soft multifocal patients eventually require modified monovision to obtain more working distance acuity. Modified monovision can be used with any lens design. The Biofinity Multifocal (CooperVision) is available in a dominant (center distance) and nondominant (center near) design, with a range of permutations and combinations of power available due to the specific add choices. I’ve had success with this lens in marginal dry eye patients and those who may have difficulty making the switch from hydrogel to silicone hydrogel materials. Some patients prefer the nondominant design in both eyes, while other prefer the dominant design in both eyes. (Don’t forget to think outside the box to problem solve—channel our friend Keith!)
CooperVision also offers one of the few toric multifocal designs available, the Proclear Multifocal Toric DW. This is a progressive design available in both dominant and nondominant options in two base curves, with an add that can be specified up to +4.00. Custom cylinder powers up to -5.75 are also offered, with sphere powers up to +/-20.00 D. The main drawback to this lens is the low oxygen permeability due to the hydrogel material; to reduce the possibility of tearing a lens, use lubricating drops before removal.
• Case 2: Residual Astigmatism or the Slightly Irregular Cornea. P.P., a 53-year-old female computer systems analyst presented wearing monovision SCL with a toric lens in her near eye. She has a history of low corneal rigidity and possibly low grade keratoconus, although she is correctable to 20/25 with spectacles. She reported being unable to read her phone without over-the-counter reading glasses.
This patient was refit into the Purevision (Bausch + Lomb) multifocal high add in both eyes, regaining better near vision and retaining her good distance correction. Though the new PureVision2 multifocal has excellent optics and is a great first choice for those patients that require excellent acuity, I frequently use the older design in cases like this, or in cases of higher residual astigmatism, because it helps “mask” astigmatism and low grade corneal irregularities due to its modulus and low water content.
With this lens, proper prevention of contamination from exogenous oils should be emphasized, and good lid hygiene should be reviewed with all patients. As with all soft lenses, the initial insertion is more comfortable if you avoid touching the inside surface of the lens when removing it from the case or flatpack. Instead, allow the lens to float out of the case onto your finger, rather than fishing for the lens in the case and leaving a fingerprint on the inside surface.
• Case 3: Aspheric Rigid Designs and the Borish Technique. Many of my translating or segmented rigid bifocals have at some point had cataract surgery, or shifted to an aspheric design. The new front surface aspherics generate far less spectacle blur than the older back surface aspheric options. These lenses are ideal for the rigid lens wearer with high visual demands.
M.P., a 61-year-old female hairdresser who is also a golfer, requires good intermediate vision for cutting hair. She started wearing rigid lenses over 40 years ago, and always has appreciated her better-than-20/20 vision. Her first experience with monovision was not good for golf, so she shifted to an aspheric front multifocal design, the Golden Eye AFM (Valley Contax). This process was suggested to me by the late Irvin Borish, OD, who said that when presbyopia becomes an issue with a GP wearer, try monovision in a larger diameter lens as you would use with a multifocal. If this method doesn’t work, switch to a multifocal design instead.
|
Fitting a Hybrid or Scleral Multifocal
Hybrid and GP scleral multifocals are some of the newest options available for presbyopic patients. Both designs have great features that turn some of even the toughest patients into good candidates for multifocals.
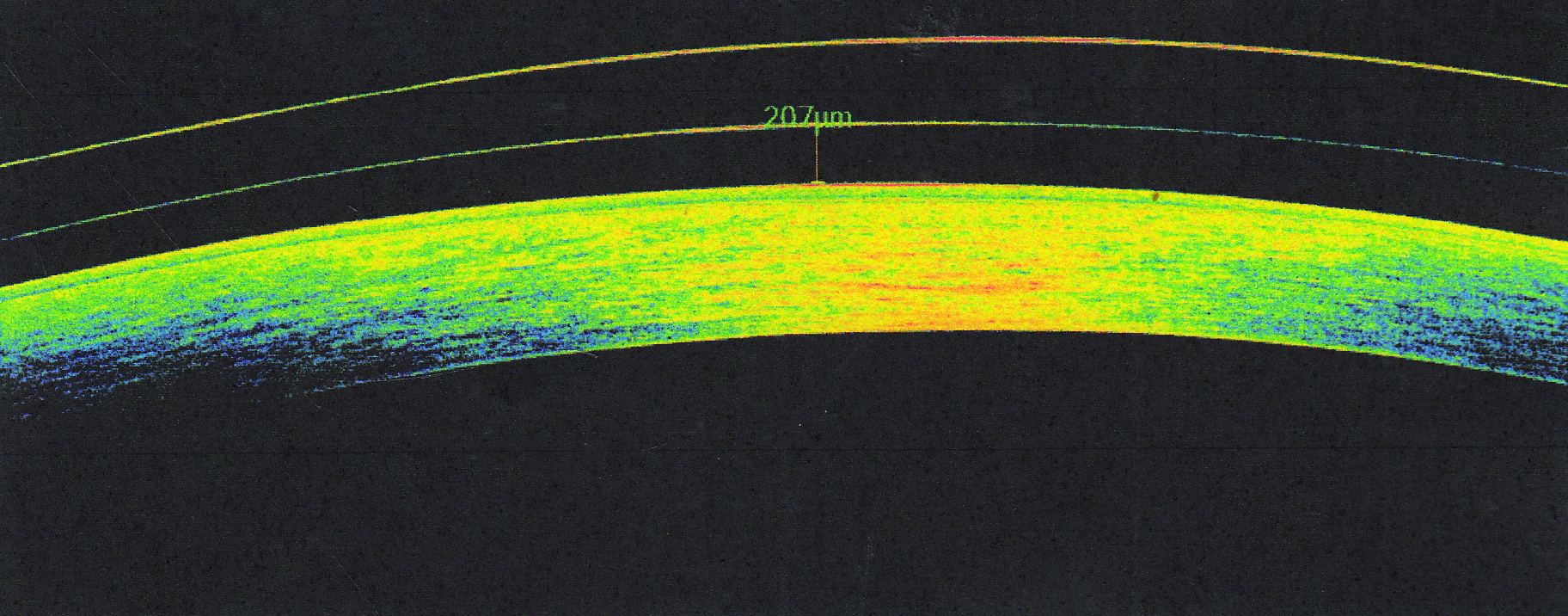
• Hybrid lens: Let’s say a 50-year-old presbyope who desires more freedom from glasses comes into your office wearing progressive addition lenses. Upon questioning, you find out the patient believes they are not a good candidate for contact lenses due to their astigmatism. Hybrid lenses are a great option for astigmatic presbyopes because the gas permeable center of the lens can mask corneal astigmatism, while the soft skirt of the lens provides patients with good comfort. Hybrid lenses can be ordered empirically with keratometry values, refraction, add power and eye dominance. This can greatly reduce chair time, especially if the first set of lenses ends up being the pair that is finalized. Also, the warranty on hybrid lenses is excellent in the case of any exchanges or returns. Patients with normal corneas can also benefit from scleral multifocals. Most of the designs have smaller diameters and are fit with less clearance (see the image above) than normal scleral lenses. Previous GP multifocal wearers along with prior soft lens wearers have both proven to be excellent candidates. In fact, I recently had a patient who had successfully worn GP multifocals for many years, but was interested in achieving slightly better comfort and reducing dry eye symptoms. I fit him into a scleral lens multifocal and he exclaimed, “This is best vision I have." |
Another modified monovision approach is to use an aspheric SV lens such as the Boston EO Envision (Bausch + Lomb) to enhance the depth of focus of both eyes. Keratoconus lens patients wearing an aspheric corneal lens reap the side effect of better near vision depth of focus than with a spherical design. I have also used the Rose K design as a multifocal lens in patients without keratoconus.
Dr. Borish also noted residual astigmatism has an increased blurring effect later in the course of presbyopia; that is, with reduced accommodation we are less able to compensate for any residual astigmatism, and eventually this will have a greater negative impact on visual acuity. So, patients who were initially tolerant of uncorrected astigmatism may require toric lenses as presbyopia progresses to obtain the best possible monocular visual acuity while remaining in a monovision modality. This must be balanced, however, against the loss of depth of focus that occurs when residual astigmatism is reduced; that is, one usually undercorrects astigmatism in monovision for better working distance.
• Case 4: Dailies and Meibomian Gland Dysfunction. M.M., a 52-year-old computer jockey, had stopped wearing his monovision lenses due to inadequate visual performance and repeated marginal infiltrates resulting from a compromised tear film and chronic blepharitis.
For a patient who has crossed the threshold to the second half of their century, multifocals may take the place of formerly successful monovision designs. Given the plethora of meibomian gland dysfunction in this population and its effect on the tear film, a dailies design is ideal. One example, the Dailies Aqua Comfort Plus Multifocal (Alcon), comes in low, medium and high adds, and in my experience can mask up to 1.00D of astigmatism. Sometimes, a little bit of residual astigmatism can actually help the depth of focus at near.
To find the best compromise for each patient, try over-refracting with flipper bars in 0.25D increments in a real-world setting. For distance, I have them look out the window and check them both binocularly and monocularly. Be sure to over-refract each eye individually, but also check their binocular distance vision and near point range. I usually explain to the patient that we can move their nearpoint range in and out, but it is more difficult to expand the range (unless the patient is comfortable with a modified monovision).
In this case, the patient was fit with a medium add Dailies Aqua Comfort Plus Multifocal in each eye, despite having around -0.75 residual cylinder in both eyes, and was aggressively treated for the blepharitis and meibomian gland dysfunction.
In cases of a severely irregular cornea or high astigmatism, a rigid design may be best. For those patients unable to adapt to a corneal lens, scleral lens designs or hybrid lenses would be the next step (see “Fitting a Hybrid or Scleral Multifocal”). As one example, SynergEyes now offers both the SynergEyes multifocal and the Duette multifocal and progressive designs, which offer better oxygen permeability. If you or the patient has difficulty removing an adherent lens, wearing latex gloves allows for easier removal—a useful tip from the late David Rosenbloom, OD, of Pittsburgh.
So, go ahead and jump right in! The possibilities are greater than they have ever been.
Dr. Keech is in a group practice in Shoreline, WA. Previously, she was on staff at Group Health Cooperative of Puget Sound in Seattle and an assistant professor at Indiana University. A fellow of the AAO and a Diplomate of the Cornea and Contact Lens Section, she also served as a member of the Executive Council.