 |
A 46-year-old Hispanic male presented to the clinic with concerns of red bumps on the white part of his right eye that have been growing rapidly since he first noticed them about four weeks ago. He reported that they are generally not painful but are sensitive to the touch, creating an uncomfortable sensation.
Ocular History
The patient had a pterygium removed on the same eye approximately two months prior. When he returned to his surgeon’s office upon noticing the bumps, he was told he had cysts that were normal and he was healing well. As the lesions continued to grow, however, the patient sought a second opinion.
The patient was using prednisolone acetate once daily in the right eye as part of his pterygium recovery and had been using timolol maleate 0.5% once daily since roughly a week after his pterygium removal.
Preliminary Testing
Entrance testing showed uncorrected visual acuities (VAs) to be 20/50 OD and 20/25 OS, with a pinhole VA of 20/25 OD. The patient’s pupillary responses, confrontation fields and extraocular muscle ranges were normal OU. His intraocular pressures were 13mm Hg OD and 12mm Hg OS.
The slit lamp exam of the left eye showed normal structures. The right eye was normal with the exception of the conjunctiva and the cornea. The conjunctiva had two large, velvety, fleshy masses, one of the nasal bulbar conjunctiva and one of the superior bulbar conjunctiva under the upper lid. These bumps were smooth and highly vascular. Though they both had a placoid, low-lying appearance, they were attached to the underlying eye wall by a much narrower appendage.
Each of these zones was surrounded by an immediate area of injected conjunctiva, though this was much more intense with the superior lesion and extended well down into the temporal interpalpebral area. Mucus was collecting around the growths but did not appear to be excessive. Other zones of the conjunctiva were white and quiet. The patient’s corneal abnormality was limited to nasal fibrosis characteristic of eyes that have undergone pterygium removal.
The Problem
The differential diagnoses in this case are relatively small. Vascular tumors of the conjunctiva include Kaposi’s sarcoma, papillomatous growths, ocular surface squamous neoplasm (OSSN) and pyogenic granuloma (PG). We can rule out Kaposi’s sarcoma because the patient has no known history of immune suppression, a feature that is closely linked to the growth. His lesion had a smooth, nodular appearance, which, although not definitively uncharacteristic of papillomatous growths or OSSNs, is much more consistent with a PG. Further, while PGs may develop spontaneously, they are often linked to antecedent insult to the conjunctiva. These insults may be incidental traumas but usually follow a surgical disruption of the conjunctiva, which our patient had with his recent pterygium removal.
Modern pterygium surgeries involve taking a conjunctival graft from the superior bulbar conjunctiva and placing it in the bed of the excised pterygium with the help of fibrin adhesive or sutures. This is done to reduce the rate of scleral melt, which occasionally occurs with bare scleral beds, but, more importantly, to reduce the rate of recurrence of the pterygium. The process creates two beds of surgically traumatized conjunctival tissues, the site of the graft harvest (superiorly) and the site of the pterygium removal (nasally). These zones, not coincidentally, correlated with the locations of our patient’s PGs. The surrounding injection was likely due to mechanical irritation of the lid blinking over the lesion and the mucus, a byproduct of that mechanical irritation combined with the disruption of tear flow across the conjunctiva.
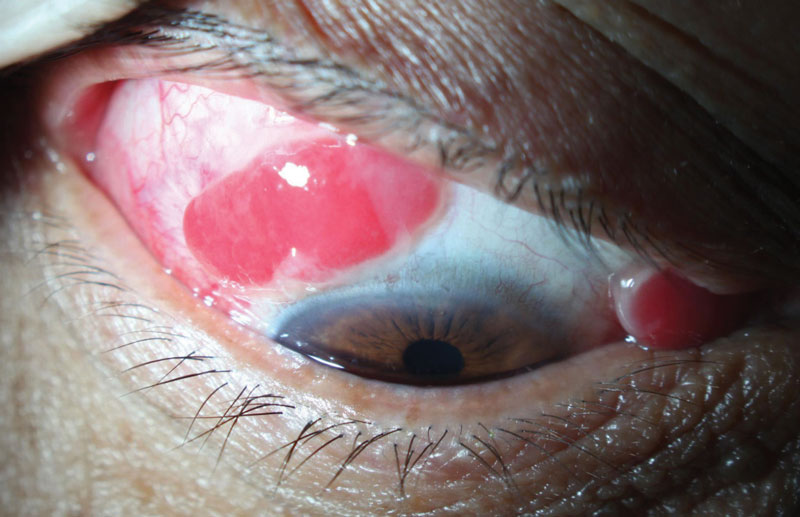 |
| These large, fleshy growths of the superior and nasal bulbar conjunctiva are consistent with PG. Click to enlarge. |
Solutions
Despite the name, PGs are neither pyogenic (related to infections) nor typically true granulomatous lesions. They are actually made up of immature capillary growths and connective tissues along with variable immune cells.1 These lesions usually develop as a result of some external insult but may occur de novo. Their color and texture are usually consistent with what you would expect of the palpebral conjunctiva. Their size and shape vary, but they are generally smooth and should be on the differential for any patient with an exuberant, red velvety conjunctival mass. As was the case with our patient, the base of these lesions may develop into a colleret.1
PGs may occasionally spontaneously involute. When involution does not take place, there are a few less-invasive treatment options available. Corticosteroids are the traditional topical option for PGs, and in a study of post-strabismus surgery patients, 90% of all lesions responded to this modality.2 A newer treatment option for smaller PGs is ophthalmic timolol maleate 0.5%, which, as a beta blocker, stifles angiogenesis, causes vasoconstriction and leads to apoptosis of the vessel.3 Studies generally show good efficacy with BID dosing over three to six weeks.4 Additionally, timolol is a reasonable, noninvasive treatment for other vascular growths of the conjunctiva, such as hemangiomas.3 For lesions that do not respond to less-invasive means, removal of the lesion with cautery of the base is standard. Recurrence of the lesion is linked to how quickly the resultant conjunctival defect closes, with those that close more slowly recurring more often.1
In our patient’s case, he had already failed on corticosteroid therapy and with timolol, given that he was using both while his growths were developing. Since conservative therapy did not prevent the growths or induce regression, we decided to take the surgical course. Due to the patient’s recent pterygium surgery, we felt the local surrounding conjunctiva would be fibrosed and our surgeon would be unable to stretch it over any resultant conjunctival defect. Therefore, we had an amniotic membrane sheet on-hand at the time of surgery to help close any open conjunctival defects. The patient was scheduled for surgery and asked to increase his prednisolone from one to four times per day until his surgery two weeks later.
Aftermath
Interestingly, when he presented for surgery, the patient reported the nasal lesion had “fallen out of his eye” earlier in the week. This was accompanied by some bleeding, which had alarmed the patient. It stopped after 20 minutes, so he did not seek help. On exam, the luxation of the lesion appeared to have left a small zone of conjunctival fibrosis and a subconjunctival hemorrhage but little else. This was probably due to a tourniquet effect of the growth’s underlying collarette combined with the constant mechanical pressure applied to it by the lid/blink reflex. We offered to observe the superior lesion, which was still present, in hopes of a similar non-surgical resolution, but the patient wished to proceed with surgery. The growth was removed, and the lesion bled significantly, but this was expected based on its vascular makeup. An amniotic membrane was used to close the conjunctival defect, and the patient healed uneventfully.
Any red, velvety, recently developed conjunctival mass should make a clinician think of PGs. Though these are not the only rapidly growing vascular conjunctival lesions, in my experience they are generally the most common and become markedly more common in circumstances where the conjunctiva has been disrupted. Fortunately, they are benign, and, though they may be alarming to the clinician initially, they often have a good prognosis and respond well to conservative therapy. In cases in which time and topical medications fail to provide relief, surgical removal is usually effective, as in this case.
| 1. Warner M, Stagner A, Jakobiec F. Subepithelial Tumors of the Conjunctiva. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. 4th ed. St. Louis: Mosby; 2017:443-65. 2. Espinoza GM, Lueder GT. Conjunctival pyogenic granulomas after strabismus surgery. Ophthalmology. 2005;112(7):1283-6. 3. Oke I, Alkharashi M, Petersen RA, et al. Treatment of ocular pyogenic granuloma with topical timolol. JAMA Ophthalmol. 2017;135(4):383-5. 4. Lubahn JG, Lee RK, Karp CL. Resolution of conjunctival sessile hemangioma with topical timolol. Cornea. 2014;33(1):99-100. |


