 |  |
Practitioners often only think of scleral lenses as indicated for those with irregular corneas, ocular surface disease or those intolerant to corneal gas permeable (GP) lenses. However, manufacturers continue to introduce new designs that make these lenses a potentially helpful option for healthy eyes with hyperopia, myopia, astigmatism and presbyopia. Here’s an overview of the benefits these lenses can provide normal corneas, as well as some concerns, and two case examples help to bring it all home.
Advantages
A scleral lens’s large size allows for minimal lens-to-lid interaction, resulting in maximal comfort from the start. These lenses also provide good vision stability due to lack of rotation and minimal movement with blink. This is especially advantageous for athletes who require stable, comfortable vision all day without the risk of a lens dislocating and ejecting from the eye on blink.
Scleral lenses are filled with fluid, which provides constant ocular surface hydration, meaning they cause fewer factors related to lens-induced discomfort compared with soft lenses.1 This tear layer also helps reduce a certain amount of the higher-order aberrations that result from irregular corneas or lenticular opacities. Additionally, the larger optic zone provides minimal halos and glare, resulting in enhanced vision.
What’s more, research shows few complications associated with scleral lens wear. Current literature includes only isolated case reports of microbial keratitis.2-4 According to the SCOPE study, the most commonly reported complication was ocular surface injury due to handling or application error.5 A relatively small number of patients in this study experienced various forms of corneal pathology, including corneal edema, neovascularization, corneal infiltrates and toxic keratopathy. Of the 84,375 patients represented in the study, only 70 cases of microbial keratitis were reported. Results from this study suggest that vision-threatening complications associated with scleral lens wear may be rare.
Astigmatism. A spherical scleral lens design can compensate for up to 3.5D of corneal cylinder in an astigmatic patient, exceeding the range provided by corneal GP lenses.6 This is due to the fluid tear layer vaulting over the cornea and masking corneal astigmatism. Because soft lenses rely on rotational stability for clear vision, lens rotation while blinking can result in vision fluctuation during the day. If this occurs, patients often feel they are compromising their vision to wear contact lenses.
One recent study reports scleral lenses as a viable alternative to soft toric lenses for astigmatic subjects. Subjects wore each modality for one month, with 75% preferring the vision of the scleral lenses compared with the soft toric lenses, and 53% expressing a preference to continue with the scleral modality.7
Fluctuating vision can also be an issue with corneal GP lenses if they are not well centered or have excessive movement on blink. With scleral lenses, meanwhile, there is minimal movement with blink, and corneal astigmatism is bypassed due to the fluid tear layer, resulting in stable, clear vision. Scleral lenses also feature an 8mm to 9mm optic zone, which enhances the field of vision and limits interaction with the pupil diameter and the perception of higher-order aberrations.6
Once a scleral lens is placed on the eye, there may be a small degree of residual astigmatism related to lenticular astigmatism. If this happens, adding a front-toric design to the lens can provide the patient with optimal vision. Residual astigmatism can also come from lens flexure.6 This is often related to poor alignment of the scleral landing to the patient’s conjunctiva. To resolve this, practitioners can incorporate toric haptics to achieve a better lens alignment in all quadrants.
Presbyopia. With today’s increasing number of available multifocal scleral lens options, this modality is clearly a viable option for presbyopes and patients with concomitant dry eye. Despite several newly available soft lens options for these patients, contact lens dropout remains high in the presbyopic population due to unstable tear film and complaints of dry eye.6 Many of these patients also display significant refractive astigmatism that, if not adequately corrected by optical means, can lead to fluctuating and distorted visual acuity.6 Unfortunately, few toric multifocal contact lenses offer a positive outcome for presbyopes with astigmatism.6
However, several multifocal scleral lens options—including dual aspheric, center-distance and center-near designs—provide exceptional vision at all distances.8 Scleral multifocals provide the dual advantages of GP optics along with constant ocular surface hydration and, as a result, stabilized tear film.
Additionally, these lenses compensate for high degrees of refractive astigmatism without the need for a front surface toric design. The larger optic zone of traditional scleral lens designs also provides room for larger add power zones with unaffected distance vision.6 As with any multifocal lens, centration is crucial to provide optimal visual performance.
Concerns
Given the variety of scleral lens designs available today, some practitioners still do not jump straight into scleral lenses for regular corneas. Currently, there are questions about how the combination of lens material, lens thickness and post-lens tear reservoir affect corneal physiology.
Early scleral lens designs came with complications due to their non-permeable materials. The lack of oxygen transmissibility led to corneal edema and neovascularization, resulting in hazy vision and increased risk of eye infections.8 With the advent of GP materials, this risk is minimized; however, proper lens alignment and central clearance is still necessary. Various studies have suggested that, despite the availability of highly breathable materials, hypoxia is still a concern.7,9
Research shows a consensus that scleral lenses should be manufactured with highly oxygen permeable (Dk) materials (>125 to 150+), low center thickness (200μm to 250μm) and low corneal clearances (less than 150μm to 200μm).7,9,10 One study acknowledged that wearing large scleral lenses is associated with chronic oxygen deprivation, leading to 2% to 3% of edema at the end of the wearing period if the lens is thick (more than 300μm) and clearance remains high (more than 250μm) throughout the wearing period.11 Another study found that the amount of corneal edema was 1.7% after eight hours of scleral lens wear.10 Clinically, this level of edema is not significant and similar to the 4% of physiological edema present upon waking.12 Still, practitioners generally use smaller diameter scleral lenses known as mini-scleral lenses for normal corneas.8
Most concerning with large scleral wear for normal corneas is uncertainty about the long-term effects of low-grade corneal edema. For patients with irregular corneas or chronic ocular surface disease, the risk is minimal compared with the benefits of restoring visual acuity or treating the ocular surface. Some clinicians will argue, however, that the benefits do not outweigh the risks for patients with healthy corneas.6 Until we have more evidence, this will remain a gray area. For now, mini-scleral lenses with limited thickness and clearance may be the safest method to provide normal corneas with scleral lens benefits.
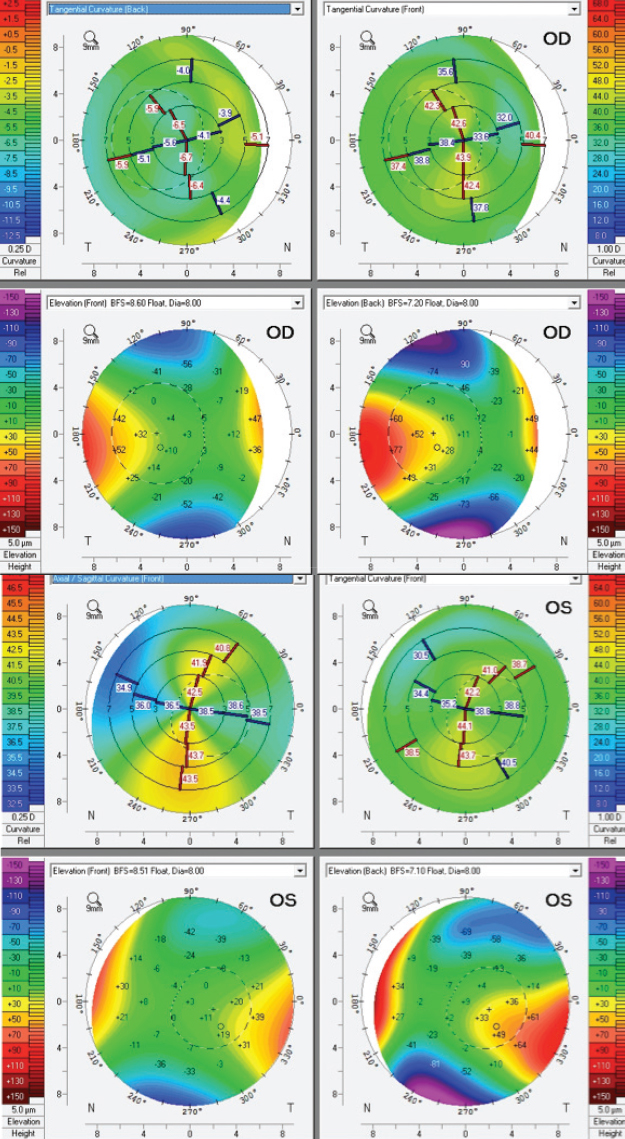 |
| Fig. 1. Corneal topography for this patient shows anterior corneal astigmatism 7.8D OD and 5.5D OS. |
Case Example #1
A 16-year-old male presented to clinic for a contact lens evaluation. He was wearing spectacle correction and reported monocular double vision in both eyes. He had ocular history of ocular albinism, nystagmus and refractive amblyopia in both eyes. Due to his high degree of hyperopic and astigmatic correction, he was self-conscious about wearing glasses at school. He reported the magnification of his eyes made students stare and he felt they could notice his eyes shake.
The patient’s spectacle correction was +7.00 -5.00x180 OD and +6.75 -5.00x175 OS. His entering acuity with spectacle correction was 20/150 OD and 20/100 OS. Due to his degree of corneal astigmatism, he was fit into a scleral contact lens (Figure 1). The patient had a horizontal visible iris diameter of 11.5mm. Since he did not have any corneal ectasia requiring excessive vaulting or dry eye complaints, we used a smaller diameter of 15.4mm.
The final scleral lenses ordered had a front surface toric due to residual astigmatism on over-refraction and toric periphery in both eyes. The toric periphery provided better alignment to the scleral landing while also improving centration and rotational stability. Best-corrected vision with scleral contact lenses was 20/100+1 OD and 20/70+1 OS.
The patient was able to wear his contact lenses for 10 to 12 hours daily. He had no issues inserting and removing lenses despite his nystagmus and reduced vision. He also reported improvement in the quality of his vision and felt more confident at school while wearing his contact lenses.
Case Example #2
A 33-year-old male presented for a contact lens evaluation. His left corneal GP lens had recently broken. He had previous history of high myopia with intolerance to corneal GP lenses and recurrent corneal abrasions while wearing them. The patient wore spectacle correction for back up; however, he had much better quality of vision with GP lenses. Given his history and degree of refractive error, he was re-fit into scleral contact lenses. His spectacle correction was -17.50 -2.25x034 OD and -17.75 -1.75x150 OS. Entering acuity with spectacle correction was 20/40 OD and 20/40 OS. He also had anterior corneal astigmatism of 1.4D OD, OS. His horizontal visible iris diameter was 12.1mm in each eye.
Given the patient’s larger corneal diameter, we fit him for a 17.0mm scleral lens. He trialed a diagnostic lens with a spherical landing zone; however, there was blanching along the horizontal meridian and uptake along the vertical meridian when sodium fluorescein was inserted (Figure 2). As such, a toric periphery was necessary to provide best alignment and avoid chamber clouding during daily wear. Best-corrected vision with scleral contact lenses was 20/25 OD and 20/30 OS.
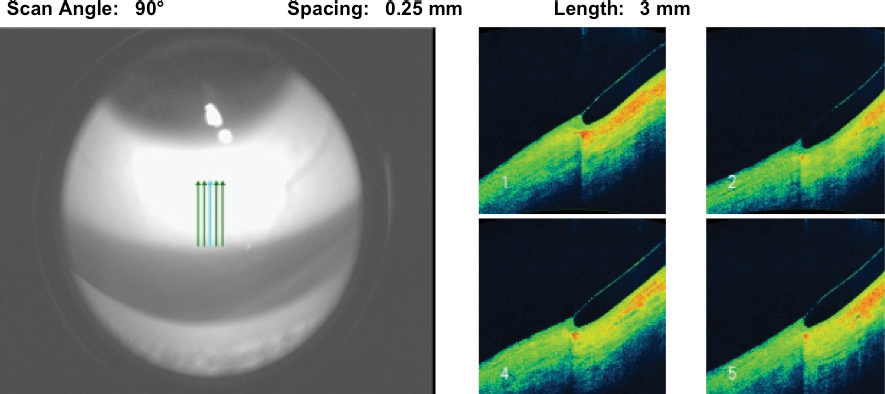 |
| Fig. 2. This lens shows mildly tight landing in the vertical meridian. |
The patient had around 220μm of central vault with 11 steps of total toricity between flat and steep meridians. He was able to wear his contact lenses for 14 hours with minimal clouding. On occasion, he would take his lenses out to clean the surfaces. Overall, the patient is happy with the vision and comfort he receives with his scleral lenses.
Scleral lenses can help manage a wide variety of irregular and normal corneas. Smaller scleral lenses may be more suitable for correcting normal corneas with refractive errors such as astigmatism, high myopia and presbyopia. These lenses may also accommodate low-to-moderate corneal irregularities.6 Larger lenses (15.8mm to 18mm in diameter) are more often used for managing severe ocular surface disease, severe ectasia and corneal irregularity.6
Practitioners should consider scleral lenses for both irregular and regular corneas. Using more than one trial fit set will allow management for a diverse patient population. Lens manufacturers and educational aids, such as the Scleral Lens Education Society, can help guide practitioners to provide successful lens fits for all patients.
1. Alipour F, Kheirkhah A, Jabarvand Behrouz M. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35(6):272-6. |


