 |
The contact lens manufacturing process has become more sophisticated and efficient since soft contact lenses were first introduced in the 1970s. Optometrists are now able to provide high quality lenses at a reasonable price to the general population.
To make the manufacturing of prefabricated lenses more cost efficient, companies design contact lenses to fit patients who fall in the center of the bell curve for shape and size. To create this bell curve, manufacturers evaluate the size and curvature of many different eyes and pick the base curve and diameter that work for as many of them as possible.
While this strategy is good for the majority of patients with average eyes, it’s not ideal for patients who are outliers. Luckily, practitioners can significantly improve fit and vision for these patients by turning to lens customization. This patient, for example, failed in traditional soft contact lenses, but found success with a little extra care.
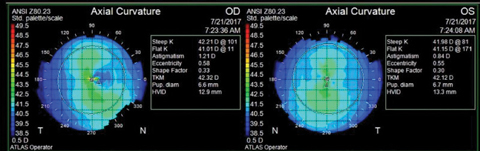 |
| Fig. 1. Corneal topography depicting large horizontal visible iris diameter OU. |
Case
A healthy 13-year-old female was referred by her ophthalmologist for a contact lens evaluation. Her motivation for wearing contact lenses was to get rid of her glasses before starting a new school in the fall.
Her ocular history was significant for nystagmus and mild amblyopia. Her medical history was positive for allergic rhinitis, for which she took Zyrtec (Johnson & Johnson) as needed.
Most importantly, she had a history of contact lens intolerance, and multiple doctors in the past two years had yet to find a successful contact lens fit. Every lens she tried would pop out. Her previous doctor went through multiple trials before settling on silicone hydrogel monthly disposable lenses, which she still couldn’t tolerate for long. She felt the lenses made her eyes dry.
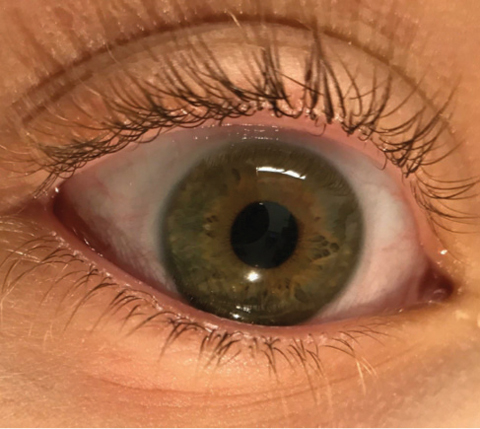 |
| Fig. 2. A 14.5mm diameter Biofinity toric lens, barely covering the corneal surface. |
The patient’s presenting visual acuity was 20/25 OD, 20/30- OS. Her presenting spectacle prescription was -1.50+0.75x089 OD and -2.25 sph OS. Manifest refraction was -1.75+0.50x085 20/25+ OD and -3.75+0.50x080 20/25 OS. Simulated keratometry per topography measured 41.01/42.21@011 OD and 41.15/41.98@171 OS (Figure 1). Horizontal visible iris diameter (HVID) was noted as 12.9mm OD and 13.3mm OS.
A slit lamp exam revealed clear lashes and cornea OU and 1+ papillae in the palpebral conjunctiva OU. The anterior chamber was deep and quiet OU. The iris and lens were normal OU. Intraocular pressure was 14mm Hg OD and 13mm Hg OS by Goldmann applanation. An undilated view of the posterior segment was within normal limits.
Contact lens fitting
The average HVID in the general population is 11.8mm.1 Due to the large diameter of her HVID, we tried Biofinity toric (Coopervision) lenses instead of spherical lenses. The new lens parameters were 8.7 BC/-1.00-0.75x175/14.5 diameter OD and 8.7BC/-2.50-0.75x170/14.5 diameter OS. The lens diameter barely covered her cornea, and the lens edge sat below the lid margin (Figure 2). A hard blink would eject the lens out of her eye. There was low movement of the lens, which appeared to be too steep on the flat cornea. We realized her large, flat corneas fell outside of the “one-size-fits-most” bell curve used by prefabricated contact lenses. From this evaluation, it was apparent she needed a custom lens.
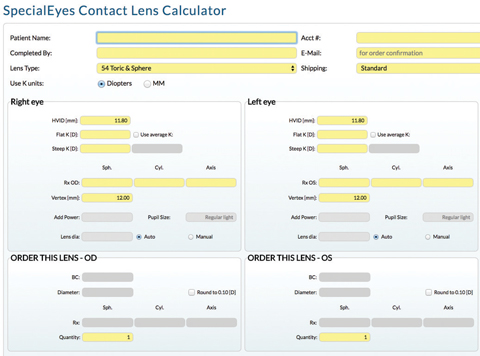 |
| Fig. 3. A custom toric lens was made for the patient using the SpecialEyes Contact Lens Calculator. |
We designed a lens empirically using the arc length soft lens calculator on the SpecialEyes website (Figure 3). Taking into account the HVID, base curve and prescription, we ordered a toric SpecialEyes lens of the following parameters: 8.6BC/-1.25-0.50x175/15.7 diameter OD and 8.5BC/-3.25-0.50x170 /15.9 diameter OS.
She also had ocular allergies, for which we prescribed Pataday (olopatadine hydrochloride) QD OU.
Dispensing
The patient presented for her lens dispensing two weeks later with no new complaints. With her new soft lenses in place, her visual acuity was 20/20 OD and 20/25 OS. The lens tucked nicely underneath the upper lid and was well-centered with adequate movement (Figure 4). We instructed the patient to use hydrogen peroxide cleaning solution for nightly cleaning to address her allergies and sent her home.
Two weeks later, the patient returned with no complaints. She was thrilled with her vision and comfort and had no issues with lens ejection.
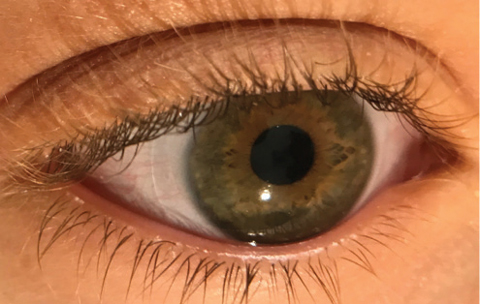 |
| Fig. 4. The patient’s new lens is well-centered with adequate cornea coverage. |
Size Matters
Soft contact lenses are traditionally fit without taking corneal diameter into account. In most cases, contact lenses are fit based on the patient’s refraction and keratometry reading. When HVID and sagittal depth are factored in, practitioners can improve patient comfort and vision by formulating a lens with better stability.
When customizing lenses, it is important to follow the fitting guidelines of each individual manufacturer. Lens materials have a large impact on the fitting characteristics of the lens.2
Custom-designed soft contact lenses will help produce loyal patients because most patients who need these lenses have given up on contact lenses. Simply listening to the patients and gathering more information can help practitioners fine-tune visual needs and personalize the fitting experience. With custom-designed contact lenses, practitioners are able to refine lens powers in smaller increments, prescribe cylinder axes to the exact degree, adjust multifocal zone sizes and specify the exact base curve and diameter of the lens to achieve the best vision and comfort.3
1. Caroline P, André M. The effect of corneal diameter on soft lens fitting, part 1. Contact Lens Spectrum. 2002;17(4)56. |


