 |  |
Specialty contact lens designs help us restore significant visual function in patients with difficult prescriptions and corneal conditions. As these designs have flourished, so too have available options for these individuals. Several lens manufacturers aim to provide designs that improve predictability and efficiency in the fitting process.
Scleral lenses in particular have seen a number of advancements over the past several years. These lenses are intended to clear the cornea and are separated from it by a nonpreserved saline solution. As our knowledge of scleral lens fitting improves, the process has become easier. Here, we discuss the factors that have simplified scleral lens fitting for today’s practitioners.
Filling Solutions
For years, those fitting scleral lenses had few options when filling the lens bowl. Unisol 4 saline was popular for a while, but has been discontinued. Addipak saline, a preservative-free sodium chloride solution, was also widely used.
Recently, however, the release of two new FDA-approved filling solutions for scleral lenses has given practitioners more options. LacriPure (Menicon) is packaged in unit-dose vials containing 5mL of saline. This filling solution is ideal for both rinsing the lenses when removing them from multipurpose solutions and filling the lens bowl prior to lens insertion.1 ScleralFil (Bausch + Lomb) is also FDA-approved for rinsing and filling the bowl of the lens prior to insertion.
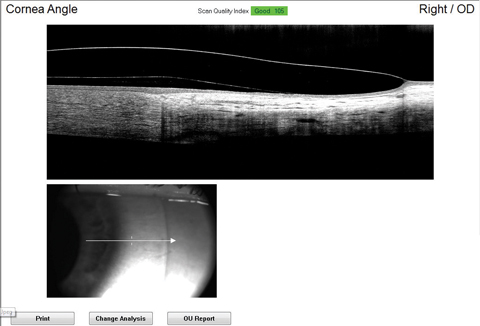 |
| Fig. 1. Limbal clearance as seen on OCT. |
Appropriate Central Clearance
Central corneal clearance can be measured a number of ways. The most commonly employed strategy is estimation at the slit lamp. Here, an optic section is created and the thickness of the lens is used to compare with the clearance.
The ideal corneal clearance is between 100µm and 300µm, and it will decrease throughout the day.3 In one study, corneal clearance decreased from the initial amount by 83µm.4 Frequently, we will attempt to fit these lenses initially closer to 300µm of clearance to allow for some expected settling throughout the day. Interestingly, the amount of settling is independent of the viscosity of the solution used to fill the lens prior to insertion.5
Although each scleral shape is unique, they tend to have an asymmetric profile that is flattest in the nasal region and steepest in the temporal and inferior regions.5 Because scleral lenses rest entirely on the sclera, they often follow the steepest regions of the scleral and migrate infero-temporally.6 Technology now allows us to visualize the central corneal clearance through optical coherence tomography (OCT) measurements. OCT cross-section scans through the lens, clearance and cornea provide a highly accurate look at the amount of clearance. This helps practitioners communicate the central corneal clearance with labs to determine any needed lens modifications.
OCT also provides unique views of the limbal region of the cornea and its relationship with the scleral lens. Practitioners can easily review a scan to confirm clearance in the limbal region (Figure 1).
Post-Lens Clouding
Clouding of the post-lens solution can be an irritating side effect for some of your scleral lens wearers. Studies show that visual quality tends to decrease over time when this happens.7
Post-lens clouding seems to occur when fluid enters and exchanges with the post-lens tear film. An inappropriate fit often causes an inadequate scleral lens fitting relationship with the conjunctiva and underlying sclera, allowing fluid exchange beneath the lens. To minimize tear exchange, some have tried using a more viscous preservative-free solution in the bowl of the lens prior to insertion. This can delay clouding, but in many cases it will still occur.
If you place a spherical landing zone on a toric sclera, there will be regions where the lens is either impinging upon the conjunctival tissue or elevated from the surface of the conjunctiva. For example, a spherical scleral lens on a sclera steeper vertically than horizontally may be elevated in the superior and inferior regions of the lens if it is aligned in the horizontal meridian. Here, the lens inappropriately aligns with the sclera.
This may occur inadvertently and cause fluid exchange under the lens in the vertical meridians. To combat this, some manufacturers have made toric peripheral curves more readily available in their scleral lens designs. This allows the lenses to better fit toric scleras. Additionally, this creates more of a chamber behind the lens, preventing fluid exchange and minimizing the effect on post-lens clouding. When used appropriately, toric peripheral curves can help alleviate a number of instances in which chronic clouding occurs.
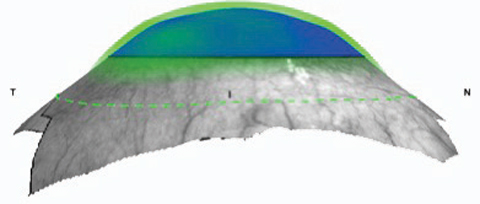 |
| Fig. 2. The sMap3D allows practitioners to create a three-dimensional model of the eye. Image: Gregory DeNaeyer, OD |
Mapping the Ocular Surface
Recent developments and advances in corneo-scleral topography provide new scleral lens fitting methods. Unlike placido-based corneal topographers, corneo-scleral topographers measure the entire anterior ocular surface, including the sclera. Elevation data is used to determine sagittal height and scleral shape. The sMap3D (Visionary Optics) corneo-scleral topographer creates a three-dimensional model of the eye and automated fitting software aids in designing a customized scleral lens (Figure 2). Customizable sMap3D options include toric haptics, quadrant specific haptics, multi-meridian (more than four quadrants), notches and edge vaults.
Lens Surface Drying
A major cause of discomfort for gas permeable (GP) lens wearers is lens surface drying. Because of this, solution manufacturers have optimized their multipurpose disinfecting solutions to help improve lens surface conditioning. Also, plasma treatments for GP surface materials have provided greater wettability.
Recently, a new treatment, Hydra-PEG (Tangible Science), has helped increase surface wettability for GP lenses.8 This involves bonding polythylene glycol to activated GP surfaces, resulting in a lens surface completely encapsulated with Hydra-PEG polymers.8
Sclerals give practitioners the opportunity to improve vision for many patients who otherwise couldn’t wear contact lenses. While these lenses require appropriate training, new technologies and designs have made them less complicated. As a result, the fitting process and patient wearing experience are more efficient than ever.
The authors would like to thank Gregory DeNaeyer, OD, for his contribution to this month’s column.
1. Menicon LacriPure, Rinsing & Insertion Saline. Available at www.meniconamerica.com/consumer/lens-care/gp/lacripure. Accessed October 20, 2017. |


