 |
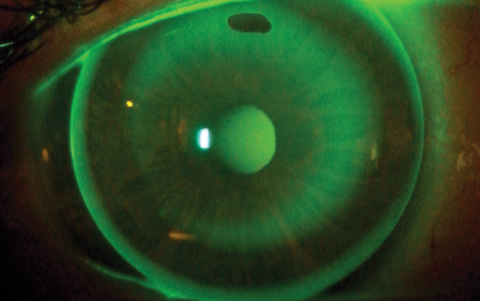
| Ortho-K’s effect on eye physiology may not always be desirable. Photo: Daddi Fadel, DOptom |
Several recent studies have addressed orthokeratology (ortho-K) and its effects on ocular physiology.1-4
A pair of studies out of Spain looked at the short- and long-term effects of ortho-K on corneal sub-basal nerve plexus (SBNP)1-2 While there were few changes in the short-term, long-term results showed a reduction in SBNP linked to changes in corneal nerve tortuosity. Also, this effect did not reverse in the first month after treatment was stopped, meaning these changes may be slow to return to baseline.
In another study from Spain, researchers found higher tear film osmolarity values in ortho-K lens wearers than in non-contact lens wearers.3 After the ortho-K lenses were removed, the tear film osmolarity values returned to normal. These results indicate that ortho-K lens wear can lead to increased tear film osmolarity, it also appears to be reversible, researchers conclude.
Another recent study explored the effect of ortho-K on axial length growth in juvenile myopic anisometropes.4 Findings revealed that axial length elongation was significantly slower in eyes treated with ortho-K than in contralateral eyes.
Additionally, 16 of the study’s 25 patients developed myopia in their contralateral eyes, which were not myopic at the start of the study.
“This study is interesting because it compares the axial length growth rate before and after ortho-K treatment in the less myopic eye after it became myopic,” says Karen Yeung, OD, senior optometrist at the Arthur Ashe Student Health & Wellness Center at the University of California Los Angeles. Ortho-K treatment in those eyes also slowed axial length growth.
Dr. Yeung says she is discontinuing ortho-K in more and more patients these days for reasons including irregular sleep and dry eye. “These patients just want one pair of glasses that they can see out of at any time,” she says. This leads her to wonder whether multifocal contact lenses or atropine for myopia be better options for myopia control.
One recent study looked at the efficacy of extra low-dose atropine (0.01%) in addition to ortho-K for myopia control in a pediatric population.5 While this reduced disease progression in patients with low and moderate levels of myopia, it didn’t impact disease progression in high myopes. As such, the researchers warn that atropine will not always be effective against myopia, but they note that a positive effect exists.
1. Nombela-Palomo M, Felipe-Marquez G, Hernandez-Verdejo JL, Nieto-Bona A. Short-term effects of overnight orthokeratology on corneal sub-basal nerve plexus morphology and corneal sensitivity. Eye & Contact Lens. 2017;44(2):77-84. |
Making Waves in Myopia
New research—slated for discussion at this year’s Association for Research in Vision and Ophthalmology (ARVO) meeting—suggests early age of myopia onset and fast progression rates are important factors of high myopia in adulthood.1 The researchers found 20% of their test subjects diagnosed with myopia before age 10 had high myopia by age 25. Such stark numbers emphasize the need for early—and effective—therapies. Clinicians planning to attend ARVO may get a sneak peek at what tomorrow’s myopia management may look like:
Contact lenses. While researchers are well versed on the benefits of exposure to violet light (360nm to 400nm wavelength) for patients with myopia, less is known about the violet light transmittance of contact lenses and its effect on myopia control. Researchers from Japan found that children who wore contact lenses with more violet light transmittance had less axial length elongation. If the results of this study are confirmed with future prospective clinical trials, the light transmittance of contact lens materials might become germane to the decision-making process surrounding myopia control efforts.2
In another ARVO abstract, a company-led case series analysis of NaturalVue Multifocal lenses (Visioneering Technologies)—a distance-center, extended depth-of-focus design—found myopic patients who switched to this lens had clinically significant reduction in progression and axial elongation. Though a small study of only one lens, the results are encouraging.3
Exercise. A recent retrospective, observational study at Kaiser Permanente Southern California found 41.9% of 60,789 patients had myopia. While the researchers were expecting the rate of myopia to increase with age, they were surprised to note that at least 60 minutes of self-reported daily exercise was associated with lower risk of myopia. The researchers believe exercise is an important modifiable risk factor clinicians should discuss with all at-risk patients.4
In addition, a recently published study of Canadian children found outdoor time positively impacted myopia, and one extra hour of outdoor play each week lowered the odds of myopia by 14.3%.5
Atropine. Yet another study shows once nightly low-dose atropine (0.05%, 0.025%, 0.01%) was effective in slowing myopia progression compared with a placebo group. The study also found atropine 0.05% had better efficacy while maintaining a safer treatment profile than other groups.6
Research has a long way to go before we fully understand myopia and how to combat it, but these findings are a step in the right direction and are poised to make waves in future treatment protocols.
1. Polling JR, Klaver CCW, Tideman W. The progression of myopia before the age of 25 years: The DREAM Study. Program 3953. Association for Research in Vision and Ophthalmology (ARVO) 2018. |
| In Brief Blackie CA, Coleman CA, Nichols KK, et al. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clin Ophthalmol. 2018 Jan 17;12:169-83. • Researchers recently found a high level of mild meibomian gland atrophy in a pediatric population. In the study, meibography was performed on 99 subjects from ages four to 17, and results showed that 42% of subjects had evidence of meibomian gland atrophy. According to those involved, this may mean it’s time to reassess our current understanding of baseline gland architecture and perhaps start examining younger patients for meibomian gland atrophy and dysfunction. Preeya K, Gupta MD, Madelyn N, et al. Prevalence of meibomian gland atrophy in a pediatric population. Cornea. Decemer 1, 2017. [Epub ahead of print]. • In a recent study of corneal biomechanical properties and anterior segment parameters in patients with obstructive sleep apnea syndrome (OSAS), findings suggest that, as OSAS severity increases, biomechanical changes may occur in corneas without topographical changes. The study looked at 54 OSAS patients and 20 healthy controls; results showed that those with severe OSAS had significantly lower corneal hysteresis and corneal resistance factor results. However, none of these patients showed any noteworthy findings on corneal topography. Dikkaya F, Yıldırım R, Erdur SK, et al. Corneal biomechanical properties in obstructive sleep apnea syndrome. Eye Contact Lens. February 7, 2018. [Epub ahead of print]. |


