Modern day cataract surgery has become a new type of refractive surgery. New intraocular lens (IOL) technology and advanced surgical techniques have improved surgical and visual outcomes to allow patients to see well at both distance and near. There are two types of IOLs: standard and premium. Multifocal IOLs, accommodating IOLs and toric IOLs are considered to be premium IOLs, because they provide a better visual outcome after cataract surgery than a standard IOL. A standard IOL is typically covered by a patient’s insurance, while a premium IOL can cost the patient an extra $1,000 to $3,000 per eye.
As can be expected, patients who pay extra for premium IOLs anticipate good vision following surgery. But, if their visual expectations are not met, they look to us for improving the outcome. In order to satisfy these patients’ demands, it is the eye care practitioner’s responsibility to determine what is causing the blurred vision and decide if further treatment is needed. In this article, we will review the different complications that may decrease vision following premium IOL surgery and the various treatments we can employ to ameliorate vision of patients with these complications.
IOL Options
It’s easy to get overwhelmed by the different IOL choices available for cataract patients. There are accommodating, multifocal, toric, aspheric and standard IOLs. Deciding on the right IOL for a patient is critical in successful implantation.
The Crystalens (Bausch + Lomb) IOL is the only accommodative lens that is FDA-approved in the United States at this time. It has undergone a number of upgrades from the first generation AT-45 to the current Crystalens AO option. Today’s newer version provides aspheric optics and excellent distance vision. The lens has hinged optics that allows it to arch forward with ciliary muscle contraction. This lens provides good distance vision and offers between 1.00D - 2.50D of accommodation. This is an ideal option for the patient who wants to see well at distance and does not mind wearing reading glasses for small print.
There are three types of multifocal IOLs on the market today: The ReZoom (Abbott Medical Optics), the Acrysof IQ ReStor (Alcon Laboratories) and the Tecnis (ZM900; Abbott Medical Optics) multifocal. The ReZoom lens has five different refractive zones with the center zone focused for distance. The Tecnis Multifocal IOL has an aspheric anterior surface and a diffractive posterior surface that splits light evenly between near and far focal points. The ReStor lens has an apodized diffractive surface. The newer version (ReStor +3.00D) gives a better range of near and intermediate vision than the older +4.00D version. In a study comparing the Rezoom, ReStor and the Tecnis multifocal, 75% of eyes with a ReZoom implant achieved J1 (Jaeger standard) in comparison to 85% with the Restor and Tecnis multifocal.1
There are two types of toric IOLs available on the market today. The Staar Toric IOL (Staar Surgical) was FDA-approved in 1998 and comes in two powers. One corrects 2.0D of astigmatism, and the other corrects up to 3.5D. The Acrysof IQ Toric IOL (Alcon) was FDA-approved in 2005. It corrects 1.5D to 3.0D of astigmatism and is available with aspheric optics and a UV blocker. Although the toric lenses are considered premium IOLs, we will mainly focus on the accommodating and multifocal IOLs.
| Halos, Glare and Diplopia |
|
“Rachel,” a 66-year-old patient has a
diffractive multifocal IOL implanted in each eye. The surgeries are done
one eye at a time, two weeks apart. At the one-week follow up of the
first eye, she reports halos around headlights, but is reassured that
the symptoms will resolve with time. The patient reports the same
symptoms in the other eye, and by the one-month follow up, she is very
unhappy because of reported decrease in distance vision, and the
presence of glare, halos and diplopia. Rachel reports to our office for a
consultation to see if her vision can be improved.
The one-month post-op exam reveals that her
uncorrected distance/near visual acuity is 20/50/ J3 OD and 20/40/ J3
OS. Her manifest refraction is +1.00-1.25 X 180 20/25 OD and +1.00-1.00 X
010 20/25 OS. The slit lamp exam shows a well-centered IOL with slight
capsular fibrosis and that the corneal incisions have healed well. No
cornea edema is noted. The patient’s Goldmann IOP is 17mmHg OD and
18mmHg OS.
At first glance, it appears that the
residual astigmatism is the culprit for the decreased distance vision.
With-the-rule astigmatism may induce diplopia and night vision problems,
but proper surgical planning should have prevented the residual
astigmatism from presenting after surgery. Capsular fibrosis is present
at this appointment but does not seem visually significant at this time.
Rachel is educated about her capsular
fibrosis and astigmatism, as well as the pertinent treatment options.
The patient had LASIK surgery in both eyes to correct the residual
hyperopic astigmatism. Immediately following the surgery, she reported
better distance vision, decreased symptoms of diplopia and slightly
improved night vision. The postoperative exam revealed that the corneal
cylinder is reduced to 0.25D in the right eye, and 0.50D in the left
eye.
In the weeks following the procedure, Rachel
noted that the distance and near vision has steadily decreased, and the
night vision had become “intolerable.” Her manifest refraction is
stable from the last visit, but her best-corrected visual acuity has
decreased to 20/40 in each eye. Slit lamp examination reveals that the
capsular fibrosis has increased in each eye, and upon these findings,
Rachel is educated about the diagnosis and treatment of capsular
fibrosis. We also explain that once the capsulotomy procedure is done,
the multifocal IOLs could not be removed in the future. The patient was
undecided for a short time but finally decided to have the capsulotomy
procedure done one eye at a time. She noticed an immediate improvement
to her vision in one eye and chose to have the other eye done shortly
after. Although the patient continued to report moderate glare and halos
at night, she was happy with her near vision and her relative freedom
from eyeglasses.
This is a good example of the extra care a premium IOL patient sometimes requires. Although this patient needed some extra hand holding and surgical treatment, she eventually ended up with a result that was satisfying and fit her lifestyle. |
IOL Selection
Patients who come in for a cataract evaluation often do not realize that they will have a choice on what type of IOL they will receive. Lifestyle and financial decisions play a big part in the decision-making process. The referring practitioner also plays a key role in this process. You should identify the visual needs of the patient and recommend a type of IOL based upon these requirements. A questionnaire that asks about hobbies, occupation and expectations for vision is a great way to start the exam.
Here are just a couple of examples of how a questionnaire can help identify which lens is right for the patient. If the questionnaire reveals that the patient desires to have good distance vision for hobbies, such as golf or bird watching, and the patient does not mind wearing reading glasses for small print, an accommodating IOL—such as the Crystalens AO—is a good option. If patients prefer having better near vision for their computer or cell phone, and they do not drive very often at night, a multifocal IOL would better suit their needs. These are simplistic explanations of a rather complex decision, but are good examples.
Doctors and staff should discuss the length of visual recovery, the risk for enhancement surgery and visual side effects during the preoperative exam. Patients will sometimes try to gauge what exactly they will be able to see after surgery. I would avoid such detailed descriptions and try to live by the rule of under-promising and over-delivering. Most doctors do not like to discuss the financial part of the procedure, but it is important to explain fees and the price for any enhancement surgeries that may be needed. Some doctors will include the price of the enhancement surgery with the original cost, while others charge an additional fee if an enhancement surgery is necessary.
Ideal Candidates
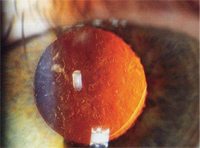
Capsular fibrosis can diminish the results of premium IOL surgery, which is why eye care practitioners should treat even small amounts of capsular fibrosis.
The best way to begin is with a thorough preoperative exam. The comanaging eye care practitioner and the surgeon’s office can work together to obtain accurate preoperative measurements. This includes a case history, cover test, ocular motility assessment, pupil testing, slit lamp examination, manifest refraction, keratometry, tonometry, topography and a dilated fundus examination. The surgeon should see the patient before surgery and perform brightness acuity testing (BAT), biometry, immersion A-scans (if needed), and a measurement of best-corrected vision with a potential acuity meter (PAM).
Pre-existing ocular pathology plays an important role in IOL selection. A patient who has macular disease does not seem to do well with multifocal IOLs. The multifocal rings provide simultaneous distance and near images that can be difficult for a diseased macula to interpret.
Some doctors perform OCT retinal imaging on every patient to identify any signs of macular disease, while others only perform the test on patients they suspect have a problem. The advantage of using an OCT before premium IOL cataract surgery is that the OCT can detect even subtle amounts of macular edema, epiretinal membrane formation and other macular diseases. Detection of these retinal problems before surgery will lessen the chance for problems postoperatively. It is important to remember that these lenses are going to last a lifetime. If an older patient has the beginning stages of age-related macular degeneration (AMD), they may be better off with a monofocal IOL vs. a multifocal.
Any pre-existing ocular surface disease should be treated before the surgery. Examples of these are anterior and posterior blepharitis, which increases the risk for infection and inflammation and dry eye, which is more prevalent in this older population. Conditions such as these should be addressed before referring the patient for cataract surgery.
Doctors need to determine if their patient is a good candidate for corneal refractive surgery in case a laser enhancement is necessary. If the patient is found to be a poor candidate for LASIK and PRK, the patient should be warned prior to cataract surgery that a corneal laser enhancement procedure is not an option.
Visual Outcomes and Treatment
Most patients do very well with accommodating and multifocal IOLs and do not require enhancement surgeries.1-3 Cataract patients are sometimes easier to please than corneal refractive surgery patients because they have worn glasses all of their life and have experienced a cloudy cataract as well.
But, if the visual result is less than expected, the comanaging eye care practitioner should look at all possible causes of postoperative blurred vision. Decreased vision following cataract surgery is most likely a refractive problem, but it can also be the result of an eye health problem or a complication involving the IOL.
You should communicate to your patients before surgery that they may experience some blurred vision for the first few days after the procedure. The cornea may be edematous from the trauma of the corneal incisions and the phacoemulsification. Once the cornea edema resolves, there are other healing processes that take place. Multifocal IOLs require a certain amount of neuroadaptation and may take time for the brain to adapt.4,5 This process may take three to six months before the patient is completely adapted to the multifocal lens.4,5
Cystoid macular edema (CME) may also present after surgery and distort the vision. This occurs in 9% of uncomplicated cataract surgeries two to eight weeks after cataract surgery.6 It happens more frequently if there is a tear to the capsule during cataract surgery or if the patient has a pre-existing vascular disease such as diabetes.7 If the comanaging doctor suspects that there is macula edema, a dilated fundus exam, fluorescein angiography test or an OCT retinal imaging system can be performed to identify the problem. OCT retinal imaging has greatly improved the diagnostic testing for CME and now allows users to identify even small amounts of retinal thickening. Topical corticosteroids and non-steroidal anti-inflammatory drugs (NSAID) are the most common medications used to prevent and treat CME.7
Despite a carefully planned surgery, some patients will have residual astigmatism, myopia or hyperopia. The refractive error can be corrected with glasses and contact lenses or other refractive surgical procedures. Bifocal eyeglasses or contact lenses are the safest options to correct residual refractive error, but for patients who pay extra for a premium IOL, they are also the least desired option.
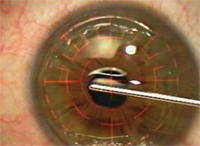
PRK surgery can be performed following cataract surgery to enhance the result.
The most precise procedure to correct residual refractive error is LASIK or PRK. Most patients would prefer to have LASIK instead of PRK because it offers a quicker healing time and causes less discomfort. But, not everyone is a good candidate for LASIK. If preoperative testing indicates abnormal corneal topography and thin corneas, the patient is at risk of developing keratectasia. Older patients or patients with epithelial basement membrane dystrophy are at higher risk for developing an epithelial slough during the creation of the flap. This happens more frequently if the flap is created with a microkeratome vs. a femtosecond laser.8
Surgeons may decide between LASIK and PRK depending upon their experience with refractive surgery. PRK surgery is simpler to perform than LASIK; therefore, an inexperienced refractive surgeon may feel more comfortable performing PRK surgery whether the patient is a good candidate for LASIK or not.
When performing excimer refractive surgery, the ablation can be done with a non-wavefront or a custom wavefront guided laser platform, although custom wavefront measurements are sometimes inaccurate following an IOL implantation.9 Furthermore, the reflections coming off the IOL may prevent the aberrometer from capturing a measurement. A non-wavefront laser ablation may be the best option in these cases.
Another possible outcome of IOL implantation is mild myopia. In these cases, surgery is not the best option, as the surgeon will sometimes purposely leave the non-dominant eye nearsighted for better near vision. But, if the patient is nearsighted in both eyes and unhappy with the distance vision, a myopic laser enhancement gives great results.
Piggyback IOLs can correct small or large spherical refractive errors after cataract surgery, but they are rarely utilized. These IOLs are placed in the sulcus of the eye while the original IOL remains in the capsular bag. Piggyback lenses are utilized if the patient is not a candidate for PRK or LASIK or if the refractive error is beyond the normal parameters of refractive surgery. For example, a piggyback IOL is a good option for a patient who is moderately hyperopic after surgery. LASIK and PRK works well for low amounts of hyperopia, but these procedures are not as predictable for higher prescriptions.
Residual astigmatism can diminish the results of a presbyopic IOL. Preoperative surgical planning and accurate measurements of corneal cylinder will decrease the risk of residual astigmatism. If a patient suffers from postoperative astigmatism, it can be corrected with a limbal relaxation incision (LRI) or corneal refractive surgery.
An LRI is performed by making a pair of deep incisions at the corneal limbus, anterior to the vascular arcade. The length and placement of the incision is dependent upon the axis and amount of astigmatism. The incisions are typically performed during the cataract procedure but can be done postoperatively as well. LRIs work well if the spherical equivalent is close to plano, and the astigmatism is under two diopters. More significant errors will do better with corneal refractive surgery. LRIs are an inexpensive and simple approach to correcting astigmatism; however, some doctors have found that they are not precise and may not correct the total amount of astigmatism.10,11
Some patients are happy with their distance vision but are upset about being more dependent on their reading glasses than expected. This is a challenging scenario because it is difficult to determine if these patients have a legitimate complaint or they are expecting too much from the surgery. Compounding the problem is that it is difficult to assess the near vision after surgery. Measuring the near vision with a normal Jaeger visual acuity card does not give us an accurate assessment of visual function. But, a timed measurement of a continuous reading card is a better assessment of reading ability.
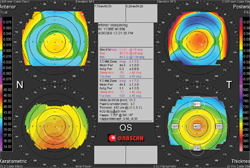
Bausch + Lomb Orbscan topography indicates that this patient is not a good candidate for LASIK because of inferior corneal steepening and thin corneas.
In order to provide the patient with the monovision effect, a monovision corneal refractive surgery can be performed over a non-aspheric accommodating IOL. There is a potential for visual distortion with performing a hyperopic laser ablation over a multifocal or aspheric lens. Hyperopic laser ablations induce negative spherical aberration and may cause visual distortion with IOLs that correct positive spherical aberration. A patient should trial monovision contact lenses before having any monovision procedures done. If the patient is happy with the monovision trial, then a standard ablation can be performed to induce myopia in the non-dominant eye.
Doctors should look closely at the posterior capsule following cataract surgery. Small amounts of capsular fibrosis may affect the visual result of a multifocal or accommodating IOL surgery. Capsular fibrosis that require a capsulotomy are needed in 18% to 44% of patients depending upon the type of IOL implanted and the material used.12 Surgeons should wait on performing an enhancement procedure with an accommodating IOL until the YAG capsulotomy is done. A study reported at this year’s American Society of Cataract and Refractive Surgery (ASCRS) meeting found that Crystalens patients had a mild hyperopic shift in refraction after capsulotomy.13
A capsulotomy should not be performed if the surgeon is considering lens removal and replacement because once it is performed, the barrier between the vitreous and the anterior chamber is compromised. Lens extraction following a capsulotomy could lead to vitreous prolapse, cystoid macular edema and retinal detachment.14 Both the surgeon and patient should make absolutely sure that the patient is satisfied with the lens before performing a capsulotomy.
Know When to Exchange
The last resort of treatment for patients who are unhappy with the result of their cataract surgery is IOL removal and exchange. Before a decision is made to remove the intraocular lens, the doctor should rule out all etiologies of blurred vision and treat even mild ocular surface disease. Patients who report having good days and bad days may be experiencing dry eye symptoms. Often, the patient needs to be reassured that having some visual side effects is not unusual. This is a delicate situation because you do not want these patients to feel that they are being abandoned or brushed off. IOL removal is an option if no other treatments can correct significant visual problems.
In some cases, a patient may request a multifocal IOL extraction because of decreased night vision or visual side effects, such as increased glare and halos, which are commonly reported side effects of multifocal IOLs.15 In most cases, the patient is aware of the risk of night vision problems before surgery and accepts the visual side effect as part of the visual outcome. Regardless of the side effect experienced by the patient, the decision to remove the lens should not be taken lightly—a second trip to the surgery center means there is a second chance for complication.
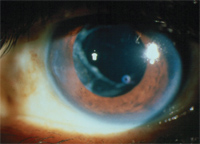
This image shows posterior capsule
following a YAG capsulotomy procedure.
There is a financial consideration here as well, as there is a fee to use the ambulatory surgery center regardless if it is an implantation or explantation. The patient most likely paid extra for the multifocal IOL and will not be expecting to pay another fee for the lens removal. In fact, the patient may be expecting a refund because he is now having a less expensive IOL placed in the eye. A more conservative treatment for glare and halos is the night time use of miotic eye drops such as Alphagan P (brimonidine ophthalmic, Allergan) or pilocarpine. Applying these eye drops 30 minutes before driving at night can decrease symptoms of glare and halos.
Dissatisfaction with vision is not the only reason a lens may need to be removed. Lens removal may need to be done if the IOL becomes decentered or develops a significant amount of tilt inside the capsular bag.15 Postoperative decentration occurs in less 1% of cataract surgeries.16 If the IOL does not fit in the bag properly, there is a higher risk of lens decentration, and the doctor is usually aware of the potential for decentration before or during surgery. Patients with pseudoexfoliation glaucoma or a traumatic cataract are more likely to have weak zonules and a decentered IOL.17,18 If the lens does decenter, a surgeon may use a tension ring to hold the lens in place or the lens can be removed and replaced.
Your Role in IOL Success

Postoperative dryness can diminish the visual result of the cataract surgery.
Comanaging a patient who has a premium IOL can be very rewarding, but it can also be challenging due to the potential complications and unwanted side effects. In the majority of cases, the patient can expect to have the procedure performed once in each eye and experience good results within days or weeks after surgery.
Still, the primary eye care practitioner should be able to recognize potential problems and be prepared for the possibility of other necessary surgeries. These extra procedures should not be viewed as a complication of cataract surgery but as part of the process in obtaining good vision. An eye care practitioner who is vigilant before and after surgery plays a major role in IOL surgery success!
Dr. Polk is the clinical director of TLC Laser Eye Center in St. Louis and an adjunct assistant professor at the School of Optometry University of Missouri - St. Louis.
1. Gierek-Ciaciura S, Cwalina L, Bednarski L, Mrukwa-Kominek E. A comparative study of the visual results between three types of multifocal lenses. Graefes Arch Clin Exp Ophthalmol. 2010:(1):133-40.
2. Cumming JS, Colvard DM, Dell SJ, Doane J, et al. Clinical evaluation of the Crystalens AT-45 accommodating intraocular lens: results of the U.S. Food and Drug Administration clinical trial. J Cataract Refract Surg. 2006;32(5):812-25.
3. Hayashi K, Manabe S, Hayashi H. Visual acuity from far to near and contrast sensititivty in eyes with a diffractive multifocal intraocular lens with a low addition power. Cataract Refract Surg. 2009;35(12):2070-6.
4. Lubinski W, Gronkowska-Serafin J, Podboraczynska-Jodko K, Karczewicz D. Cataract surgery with bilateral multifocal ReZoom intraocular lens implantation-Comparison of 3 and 12 month follow-up. Klin Oczna. 2009;111(10-12):327-31.
5. Palomino Bautista C, Carmona Gonzalez D, Castillo Gomez A, Bescos JA. Evolution of visual performance in 250 eyes implanted with the Tecnis ZM 900 multifocal IOL. Eur J Ophthalmol. 2009;19(5):762-8.
6. Mentes J, Erakgun T, Afrashi F, Kerci G. Incidence of cystoid macular edema after uncomplicated phacoemulsification. Ophthalmologica. 2003;217:408-12.
7. Nelso ML, Martidis A. Managing cystoid macular edema after cataract surgery. Curr Opin Ophthalmol. 2003;14(1):39-43.
8. Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(4):804-11.
9. Hardten DR. Refractive surgery enhancements after presbyopic IOLs. Paper presented at: The 2009 ASCRS Symposium on Cataract, IOL and Refractive Surgery; Cornea Day Meeting;April 3, 2009, San Francisco, CA.
10. Roman S, Auclin F, Baudouin C. Limbal relaxing incisions to correct preexisting astigmatism during cataract surgery. J Fr Ophthalmol. 2009 Jun 32(6):390-395.
11. Mendicute J, Irigoyen C, Ruiz M, et al. Toric intraocular lens vs. opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg. 2009;35:451-458.
12. Vock L, Menapace R, Stifter E, Georgopoulos M, et al. Posterior capsule opacification and neodymium:YAG laser capsulotomy rates with a round-edged silicone and a sharp-edged hydrophobic acrylic intraocular lens 10 years after surgery. J Cataract Refract Surg.2009;35(3):459-65.
13. Bucci FA. Effects of Postoperative Atropine, YAG Capsulotomy, Spherical Aberration, Defocus and Pupil Size on Near Visual Performances of Models of Blended Hinged Accommodating IOLs.2010 ASCRS meeting.
14. Abbasoqlu OE, Hosal B, Tekeli O, Gursel E. Risk factors for vitreous loss in cataract surgery. Eur J Ophthalmol. 2000;10(3):227-32
15. Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(6):992-7.
16. Packer M. Tilt and decentration: toward a new definition of tolerance. EyeWorld. 2005;10(6):65-66.
17. Conway RM, Schlotzer-Schrehardt U, Kuchle M, Naumann GO. Pseudoexfoliation syndrome: Pathological manifestations of relevance to intraocular surgery. Clin Experiment Ophthalmol. 2004;32(2):199-210.
18. Arbisser LB. Managing intra-operative complications in cataract surgery. Curr Opin Ophthalmol. 2004;15(1):33-9.


