 |
In any profession, new products and designs drive innovation. Within the scope of contact lenses, it is important to discuss new products, materials and fitting modalities with appropriate patients, including early cataract and post-surgical patients. These individuals may be considered “medical” patients rather than “contact lens” patients because of their recent history, but they too may benefit from corrective lenses. Below, Dr. Miller describes three cases.
Case 1: Cataract Conundrum
A 54-year-old female patient presented with complaints of blurred vision at both distance and near while wearing her soft toric monovision contact lenses. Specifically, vision in her right eye fluctuates throughout the day more so than her left eye. She is considering discontinuing contact lens wear due to the loss of clear, crisp vision. Her average wear time is eight to 10 hours; however, she has steadily decreased this time due to her visual and comfort symptoms. The patient is a teacher who works in front of a computer; she has experienced dryness, discomfort and ocular fatigue with her current lenses. She also reported that night driving is becoming increasingly difficult. She has been wearing her current prescription for the past three years. She reported vitreous floaters in the past that seem to have remained about the same.
An external ocular examination revealed both eyes were slightly dry with a tear film breakup time of six to seven seconds, but no fluorescein staining present OU. These signs are consistent with grade 1 dry eye. Dilating drops were administered, and a subsequent internal ocular examination revealed a small “off-center” posterior subcapsular cataract OU (Figures 1 and 2). The patient reported this finding in her history as being present since she was a child; no prior treatment or surgery had been recommended.
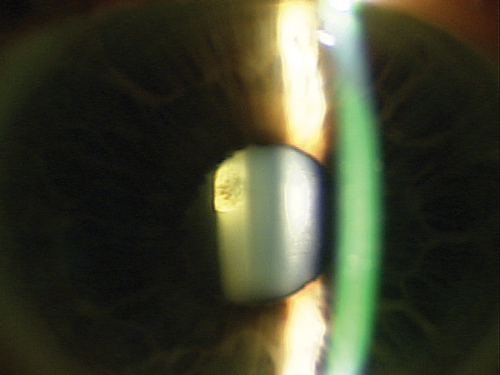 | |
| Fig. 1. Posterior subcapsular cataract OD. | |
 | |
| Fig. 2. Posterior subcapsular cataract OS. |
After reviewing various contact lens options, the patient and I concluded a hybrid multifocal was the best choice for her particular combination of astigmatism and cataract. The design also alleviates discomfort due to her mild dry eyes. I discussed appropriate visual expectations and the basics of the lens design, including the expected time it would take for the fitting appointment and subsequent visits. She adapted nicely to the lens and her visual needs were satisfactory.
Case 2: Post-LASIK Multifocal Fit
A 49-year-old female patient presented looking to wear contact lenses again. She underwent LASIK 10 years ago and reported satisfaction with the results up until the last few years, as she was needing to wear her readers more and more often. Her refraction was slightly hyperopic (+0.25D OD and +0.50D OS) at distance and required a +2.00 near add. All other ocular health evaluation points were unremarkable.
The challenge with these patients is that many wore soft contact lenses preoperatively and, often, they expect they can also wear them postoperatively. Some have this ability, but for others, it is difficult to maintain stable vision because of alterations in corneal architecture. The central flattened cornea can be difficult for soft lenses to conform to and will, at times, lead to the lens vaulting the cornea. This will result in visual instability between blinks.
I discussed these challenges with her and recommended starting with a daily disposable multifocal lens due to her history of soft lens wear prior to LASIK. She tried two different multifocal lens designs that ultimately did not work: after allowing them to settle for a few minutes, her vision was not nearly good enough at distance or near, even with an over-refraction. I tried one more daily multifocal design with a slightly flatter base curve and achieved much better initial results.
Case 3: Post-Surgical Fix
A 41-year-old post-refractive surgical patient presented looking for better vision in her contact lenses. Her RK and AK scars were distorted and wavy in both eyes. Her MR was +3.00-2.75x004 OD and +3.50-3.00x175 OS postoperatively after unsuccessful refractive procedures OU. Her corneas were extremely irregular, with best-corrected visual acuity being 20/25- OD and 20/30+ OS. She had a history of unsuccessful contact lens wear and was looking for some relief.
I recommended large diameter, reverse geometry GP lenses for this patient. Reverse geometry GP lenses allow for complete vaulting of the central cornea and enhance patient comfort, improve centration and visual acuity in cases such as this one. The patient elected to try the lenses and, at her follow-up visit, she reported better comfort. Her vision was also slightly better at 20/25+ OD and 20/25-2 OS.
Being comfortable and proficient with satisfying a wide variety of patients’ visual needs is critical to the success of your contact lens practice. Always choose a design that will provide good optics and comfort. Discuss the benefits first, then touch on the challenges associated with correcting their visual needs. Remember, these lenses may require some creativity on the part of the doctor, so always be prepared to accommodate necessary changes.


