If you work with multifocal contact lenses, you also deal with unhappy, frustrated patients. At times you may also feel unhappy and frustrated yourself. Vision and comfort issues can make multifocal fitting complex and, too often, unsuccessful. However, a successful multifocal fit doesn’t have to be a rarity. Changing how you communicate and re-structuring how you troubleshoot can flip your failures into successes. Here we discuss strategies for identifying dissatisfied patients, improving communication regarding lens wear and optimizing lens performance.
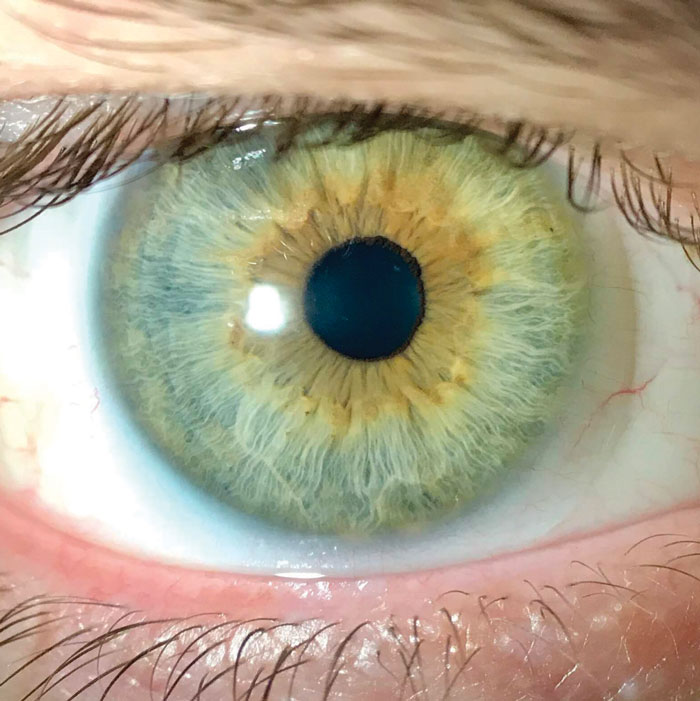 |
| With today’s advances, soft multifocal lenses present many benefits to patients, and it’s worth the extra time it takes to fit them successfully. Click to enlarge. |
Room for Improvement
Contact lens wearers are not always forthcoming about problems. When asked about their comfort or quality of vision, they may shrug and remark that they are doing “fine.” This short, nondescript answer is unhelpful and means you need to do more digging to get the real picture. In addition to the typical, “When and how long do you wear your lenses?” question, some others you can ask to help uncover room for improvement include:
- Why don’t you wear your contact lenses every day?
- Would you like to wear your contact lenses longer each day?
- At what time do your contact lenses begin to feel uncomfortable?
- How is your vision when driving or looking far away?
- How well can you see your phone and computer?
- How often do you use reading glasses over your contact lenses?
- What do you wish you could see better with your contact lenses?
These questions may help you realize that even if your patient’s current contact lenses are “fine,” their pattern of contact lens wear may highlight deficiencies. For example, limiting contact lens use to only evenings or weekends generally indicates a problem with vision or comfort that limits contact lens wear in the workplace.
Patients with specific multifocal complaints such as distance blur, glare or inadequate near vision may be disappointed in the performance of the lenses. While having appropriate expectations is important, avoid trying to immediately lower the patient’s expectations after a disappointing initial experience. This can leave the patient feeling as if they invested in a process that will yield meager results. Instead, reinforce your understanding of the patient’s limitations with their current contact lens brand and prescription, then highlight your plan to assess their vision and find opportunities for improvement. Your ability to win over dissatisfied patients correlates with the enthusiasm and confidence you convey in your ability to address their issues.
 |
| Conditions such as allergic conjunctivitis can hinder success and must be addressed to ensure patient comfort and continued multifocal lens wear. Click to enlarge. |
The Right Design
First, make sure you are fitting based on an updated refraction. Many presbyopes experience a hyperopic shift due to decreasing index of refraction in the lens, exacerbating their presbyopic symptoms.1 Use the most plus or least minus prescription to maintain clear distance vision while maximizing the benefits of the multifocal. Patients with astigmatism who have “gotten by” with spherical contact lenses in pre-presbyopic years may not be able to tolerate the combined astigmatic blur and multifocal aberrations.
For most spherical multifocal designs, up to 1.00D of astigmatism can be tolerated. Patients with higher refractive error powers often tolerate uncorrected astigmatism better. Consider toric multifocals for patients with higher amounts of astigmatism. Finally, emmetropic and low-hyperopic presbyopes are likely experiencing vision problems for the first time—an alarming revelation to these patients. Acknowledging these from the start will lead to a more optimal result.
Consider an alternate method of vision correction if your patient has a tropia and lacks stereopsis. Multifocal contact lenses are designed to supplement one another to offer the wearer a range of clear vision without the need for reading glasses. When a tropia exists, the vision system cannot summate the images as intended and the multifocal performance lags. These patients are better candidates for monovision or may need to use distance correction with reading glasses for optimal performance.
While many of the modern soft contact lens designs employ center near optics, both visual performance and lens preference can still vary from person to person. Contact lens decentration, pupil size variability, or the natural aberrations of the eye you are working with can have real impacts on vision performance. If, even after adaptation and optimization, the vision quality provided by the contact lens remains inadequate, consider trying a different multifocal design altogether.
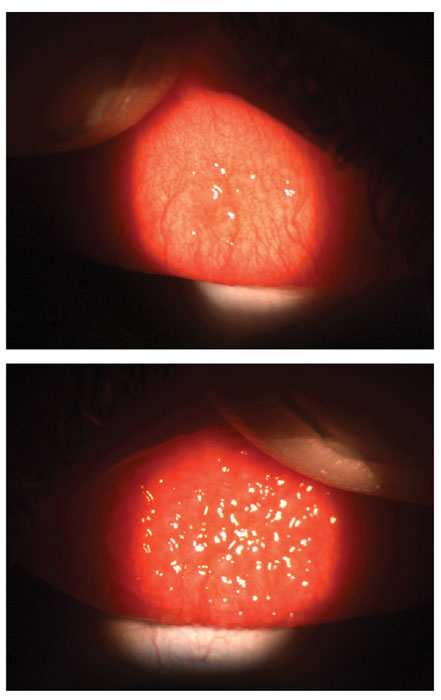 |
| Patients with mild (above) or severe contact lens papillary conjunctivitis will have textured, inflamed eyelids, which can cause discomfort and keep them out of contact lens wear. Click to enlarge. |
Vision Quality
Appropriately assessing vision in office will allow you to isolate areas of visual satisfaction and send your patient home with lenses that optimize vision at all distances. An effective vision assessment includes binocular high contrast visual acuity at distance and near, with over-refraction at distance only. If their history or entering visual acuity shows room for improvement, consider including monocular visual acuity at distance and near, which can help identify the cause of reduced visual acuity. For example, if visual acuity is reduced at distance but good at near, the eye is likely under-minused. Reduced visual acuity at both distance and near could be due to uncorrected astigmatism or an over-minused prescription. While these trends don’t help quantify a needed change, when considered along with the over-refraction, they provide rationale for implementing a lens change.
Interpreting and addressing patients’ symptoms can be challenging, but it’s even more complex if you aren’t speaking to your patients clearly. Optometry has specific definitions for distance, intermediate and near as they relate to working distances, but patients don’t adopt this same jargon. To minimize unintended context when discussing visual performance, encourage patients to focus on specific tasks or activities they are struggling with and encourage them to bring samples or identify similarly sized text in-office. If they are having difficulty seeing on the job, have them describe and simulate the setup of their workplace. Understanding the patient’s needs helps you make the best recommendations for material or parameter modifications.
If the patient reports distance vision problems, consider the results of the distance over-refraction. You should always implement a plus-powered distance over-refraction because this improves the entire range of vision in multifocal lenses. A minus-powered over-refraction, which will reduce multifocal effectiveness, should be demonstrated binocularly at distance and near before making a change.
In some cases, only part of the minus-powered over-refraction is implemented to maintain the patient’s range of near vision. If distance vision problems are reported with a plano over-refraction, rule out limitations by uncorrected astigmatism and then refer to the fitting guide to determine the appropriate change.
If the patient reports near vision problems, the ideal scenario is that the patient accepts plus in the distance over-refraction. If they do not accept plus, the fitting guide will recommend the next changes, which could include increasing the add power or adding plus power to the non-dominant eye.
Prescription or lens material changes should be driven by the patient’s subjective level of satisfaction, not visual acuity, especially when considering near vision. If you or your patient get caught up in specific acuity goals, lens changes may be made that improve acuity but do not positively impact the patient’s quality of life. Using point print sizes for near vision testing can help avoid fixation on achieving 20/20 vision and thus maintain focus on the patient’s visual goals.
If you don’t have the trial lenses you need, consider ordering them. Steps as small as 0.25D can have a significant effect on range of vision in multifocal lenses. When discussing the changes with the patient, reinforce your understanding of the patient’s visual needs and concerns, then highlight how you have addressed their needs.
Before departing, review challenges the patient may experience and highlight the feedback you would like to receive at follow-up. The patient must know that multifocals often will not perform as well with fine print or dim lighting. Suggest a pair of low-powered (e.g., +1.25) readers for spot usage and extra lighting in their work area, if possible. The patient should be coached to keep track of activities that are challenging in the lenses. While complete freedom from readers may not be achievable, knowing what tasks are challenging will help you better understand the context of any vision issues.
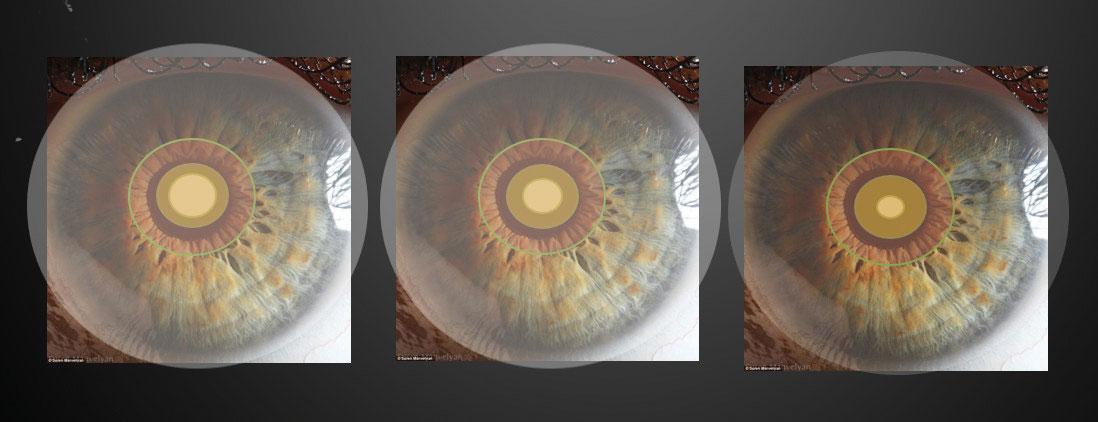 |
The patient’s pupil size can affect the lens performance, so varying the multifocal zone sizes, seen here, based on this measure can help. Click to enlarge. |
The Ocular Surface
Clear vision at all distances isn’t worth much if your patient is uncomfortable in their contact lenses. As with any contact lens modality, multifocal wearers may experience comfort issues. It may be easy to suggest an artificial tear and hope for the best, but lubrication alone is not a lasting solution for your patients’ comfort issues. A recent study reported that subjects using artificial tears wore their lenses less and were more likely to drop out of contact lens wear.2 Lubricant drops can offer short-term relief, but they require frequent dosing and may treat symptoms that could be better addressed with other interventions such as modifications to the contact lens material, care solution or replacement frequency.
Throughout the fitting process, make sure dry eye, meibomian gland dysfunction and allergic issues are addressed. Implementing appropriate lid hygiene, for instance, can improve the lipid tear layer, reducing tear evaporation and improving comfort. Allergic conjunctivitis and contact lens papillary conjunctivitis can lead to textured, inflamed eyelids with symptoms of itch, dryness and discomfort. Everting eyelids and evaluating the health and texture of the palpebral conjunctiva may help you isolate causes of discomfort and eliminate them early.
Using daily disposable multifocal modalities can help you manage and avoid many discomfort issues. Introducing a clean material that is free of allergens and deposits will allow for maximum comfort and vision quality. Daily disposables also eliminate the need for solution, avoiding any hypersensitivity reaction with a care solution. In the past, daily disposable multifocal lenses were rare and prohibitively expensive. But today’s contact lens market has expanded to include more daily disposable multifocals at a variety of price points. In addition, many reusable multifocal designs are available in a daily disposable design, so you should aim to fit the majority of your multifocal wearers in daily disposables to optimize comfort.
Compared with other fitting processes, successful multifocal fittings require a unique, highly communicative approach. Keeping patients involved in the fitting process by addressing their concerns early, educating them on how the lenses work and acknowledging negative symptoms will maintain their confidence in the process. Focus on subjective patient responses instead of objective visual benchmarks to achieve the patient’s specific visual goals. Next time you encounter an unhappy multifocal wearer, consider these tips and enjoy a smoother troubleshooting experience.
| 1. Grosvenor T, Skeates PD. Is there a hyperopic shift in myopic eyes during the presbyopic years? Clin Exp Optom. 1999;82(6):236-43. 2. Pucker AD, Jones-Jordan LA, Marx S, et al. Clinical factors associated with contact lens dropout. Contact Lens Anterior Eye. December 2018. |


