Contact lenses can be a safe and effective form of vision correction when properly worn, treated and maintained.1 When not cared for appropriately, however, lenses could present several problems that we should attempt to avoid whenever possible. Be on the lookout for and know how to address these top four contact lens complications in your patients.
Online Sales
More so now than ever, practitioners and patients alike are dealing with an outside threat: online contact lens vendors. These sellers cannot sell unverified lenses, alter lens prescriptions or fill lens prescriptions unless they are accurate and have not expired. Doing so is illegal. There are many illegal contact lens sellers in the United States, including those who sell decorative or colored lenses.
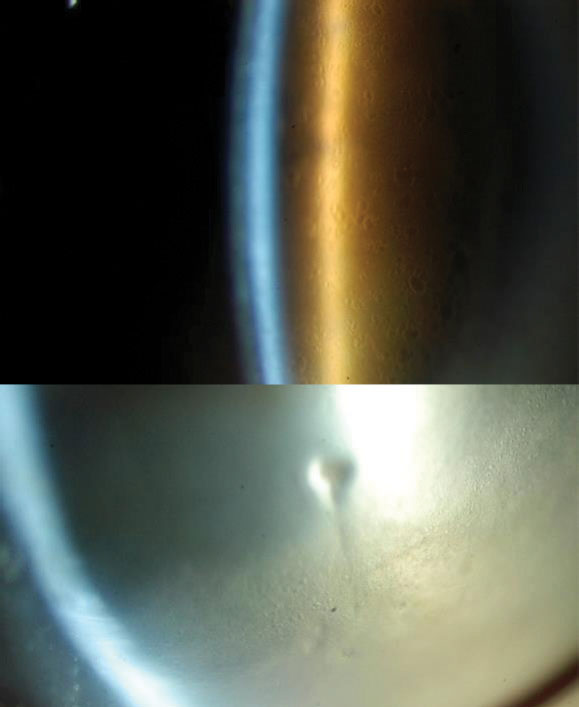 |
| Microcystic corneal edema appeared in two cases of post-penetrating keratoplasty and after eight hours of scleral lens wear. Photo: Karen Carrasquillo, OD, PhD |
A recent online survey of 22 optometrists outlined the consequences of purchasing decorative lenses through unauthorized vendors.2 Patient complications from obtaining these lenses both legally and illegally were reported by 77% of respondents.2 Half of those who had negative responses did not receive proper care and handling instructions and were unaware that these instructions even existed, rendering them inept in maintaining proper lens wear and warding off unwanted effects.2 If you suspect any illegal contact lens sales or observe any adverse events from unverified contact lenses, report these activities immediately by emailing [email protected] and contacting MedWatch, the FDA Safety Information and Adverse Event Reporting Program (www.fda.gov/medwatch), to prevent further consequences.
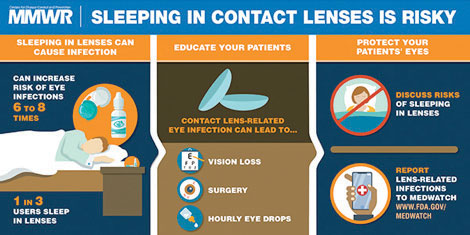 |
| Sleeping in contact lenses can cause eye infections.13 Image: MMWR |
According to Jeffrey Sonsino, OD, “we are at a time of unprecedented disruption in the industry.” Online-based vendors are discouraging the doctor-patient relationship, downplaying the importance of thorough eye examinations and contact lens fittings and taking advantage of unsuspecting lens wearers to make a profit at the expense of buyers’ ocular and systemic health. This makes it more important than ever to explain to patients that contact lenses are medical devices that require a valid lens prescription and a comprehensive eye examination. A multitude of systemic conditions, such as diabetes, hypertension and melanoma, can be caught with an eye examination to lower the risk of further visual impairment.
Lens Discomfort
Beyond providing good vision and comfort, well-fit contact lenses can promote retention and prevent dropout. Contact lens dropout, due to a complication like lens discomfort, is a prevalent issue and remains around 15% to 20%, even with new lens materials.3-9
Bridging the Age GapContact lenses should not only be considered for older demographics. They are an excellent option for children as long as these young patients can practice good hygiene and are motivated to take care of their contact lenses. A study found that myopic children who chose to wear contact lenses after five years of using glasses had higher self-esteem compared with those who chose to remain in glasses.24 The authors suggest that self-esteem may influence the decision to wear contact lenses.24 A 2016 population-based survey looked into contact lens wear, care behaviors, risk factors and demographics in different aged populations in the United States.13 Eighty-five percent of the estimated 3.6 million adolescents wearing contact lenses reported at least one behavior that put them at risk for a lens-related eye infection, compared with 81% of young adults and 88% of older adults.13 The authors concluded that encouraging adolescents to adopt healthy contact lens wear and care behavior earlier on may help them maintain these good habits into young adulthood when the frequency of risk behaviors associated with contact lenses increases.13 |
A study sought to determine if the meibomian gland and tear film characteristics were affected by soft contact lens wear and possibly contributing to lens discomfort.10 The researchers found that, in symptomatic contact lens wearers, grades of foam at meibomian gland orifices, expressibility, quality of secretions, tear evaporation rates with or without contact lens wear, tear break-up times and tear lipid layer thicknesses were all significantly associated with symptoms of discomfort.10 They noted that there were significant correlations between upper eyelid wiper epitheliopathy, meibomian gland acini reflectivity and tear meniscus height and comfort scores in both symptomatic and asymptomatic contact lens wearers.10
Another study evaluated the relationship between lid wiper epitheliopathy and ocular surface signs and symptoms.11 Lid wiper epitheliopathy width was associated with greater symptoms in contact lens wearers, decreased tear film stability, lid anatomy and lid-parallel conjunctival folds.11 The team found more Demodex mites in the upper eyelids of symptomatic lens wearers and attributed discomfort symptoms in these patients to morphological irregularities of the meibomian glands and alterations to tear film secretions that affect tear evaporative dynamics.11 Clinically, this highlights the importance of evaluating the ocular surface in contact lens wearers.
Eye Infections
While convenient, contact lens use also puts wearers at greater risk for lens-related eye infections, particularly when they do not wear and care for their lenses appropriately.12 Many behaviors increase the risk of developing a lens-related corneal infection, one of the biggest and most commonly reported being sleeping in lenses.13 Approximately one third of adolescent and adult contact wearers report that they sleep in their lenses.13 Regardless of lens material and replacement frequency, sleeping in contact lenses is a significant risk factor and increases the risk for lens-related eye infections six- to eight-fold.14-16 These eye infections can cause vision loss, require eye drop usage and may even lead to surgeries like corneal transplantation.
Microbial keratitis (MK), a sight-threatening condition that rapidly progresses, is the most serious corneal complication associated with wearing contact lenses.17 Pseudomonas causes MK in more than half of cases.18 Acanthamoeba keratitis should also be included in the differential, particularly if there is any water exposure, if pain exceeds the clinical appearance or if the patient is not responding to antibiotics. Although MK only affects a small proportion of contact lens wearers (four per 10,000 annually), the large population of individuals who wear contact lenses and the serious threat of vision loss make it a much larger issue to combat.19
A study investigating contact lens water exposure found that both soft and gas permeable lens wearers regularly expose their lenses to water and are unaware of the potential consequences of these risky behaviors.20 It is imperative to educate contact lens wearers on proper lens hygiene and the dangers of not taking proper care and handling instructions seriously. Tips for safe contact lens wear include washing and drying hands prior to lens handling, not using tap water to clean lenses, not rinsing lens cases in tap water, replacing lens cases monthly, not swimming and showering with lenses, avoiding eye rubbing when wearing lenses and replacing lens solutions daily.21,22
 |
| Any age demographic can use contact lenses as long as patients are following the proper care and handling instructions. |
Scleral Contraindications
While innovative in their corrective abilities for corneal irregularities and their indications for ocular surface disease, scleral lenses may not always be the most ideal choice.
Specular microscopy provides helpful information about the corneal endothelium and can help reveal any contraindications for scleral lens wear. Specifically, knowing endothelial cell counts can be especially useful in managing patients with corneal transplants. Patients with reduced endothelial cell counts and endothelial disease may be at higher risk for developing corneal edema and are not ideal candidates for scleral lenses. Pre-existing corneal edema prior to scleral lens wear and microcystic corneal edema with scleral lens wear are also concerns when considering scleral lenses. Evaluate the cornea prior to commencing a scleral lens fitting to determine if the patient has any underlying pathologies that may predispose the cornea to develop edema with scleral lens wear.
Prior to the initial scleral lens fitting, specular microscopy can also detect and quantify polymegethism (cell size variability) and pleomorphism (cell shape variation). Potential contraindications to scleral lens wear include epithelial basement membrane dystrophy, guttata, Fuchs’ corneal dystrophy, corneal edema and other corneal dystrophies. If a scleral lens is the only choice for patients who may not be the best candidates, options include reducing scleral lens wear time, adding channels or fenestrations and altering the scleral lens fit to make it looser.23
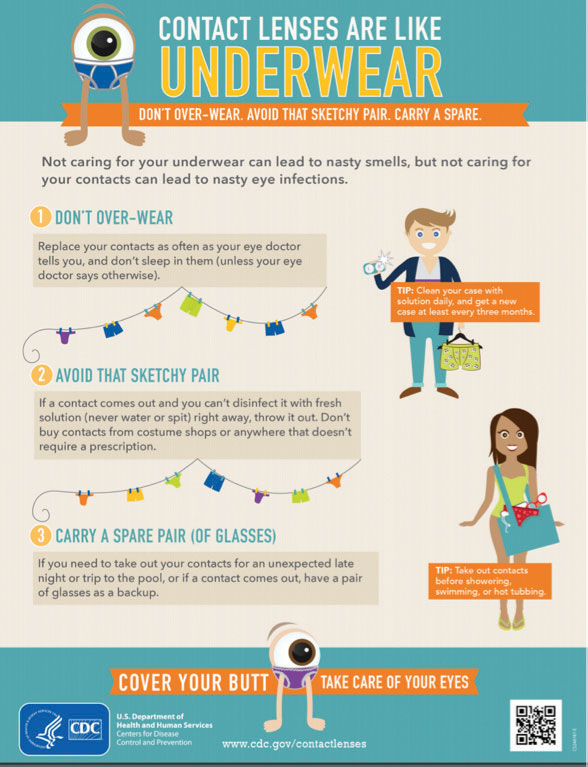 |
| Healthy contact lens habits go a long way in creating a comfortable, uneventful experience for wearers. Image: CDC |
There is an ongoing debate between researchers and scleral lens practitioners over whether scleral lenses elevate intraocular pressure (IOP) and impact glaucoma. Unfortunately, there is no direct and consistent way to accurately measure IOP on the cornea while wearing scleral lenses, and significant limitations exist associated with the tonometers researchers use to obtain these measurements. That being said, practitioners should exercise caution when fitting scleral lenses on patients who may be susceptible to or suffering from glaucoma.
It’s hard to imagine a world in which contact lenses don’t exist. They are often crucial for patients in need of vision correction. We as primary eye care providers can do many things to improve the overall wearing experience, including discouraging illegal online sales, promoting contact lens comfort, combating eye infections and choosing the optimal contact lenses for our patients based on their individual characteristics.
Dr. Barnett is a principal optometrist at the University of California Davis Eye Center in Sacramento, CA, and the past president of the Scleral Lens Education Society. She is a fellow of the American Academy of Optometry, a diplomate of the American Board of Certification in Medical Optometry and a fellow of the British Contact Lens Association.
|
1. Cope JR, Konne NM, Jacobs DS, et al. Corneal infections associated with sleeping in contact lenses—six cases, United States, 2016-2018. MMWR. 2018;67(32):877-81. 2. Gaiser H, Ho J, Janier N, et al. Practitioner perceptions of patients wearing decorative contact lenses purchased through unauthorized sellers. Eye Contact Lens. 2017;43(2):135-9. 3. Schlanger JL. A study of contact lens failure. J Am Optom Assoc. 1993;64(3):220-4. 4. Weed KH, Fonn D, Potvin R. Discontinuation of contact lens wear. Optom Vis Sci. 1993;70(12s):140. 5. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999;26(6):157-62. 6. Young G, Veys J, Pritchard N, et al. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002;22(6):516-27. 7. Richdale K, Sinnott LT, Skadahl E, et al. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007;26(2):168-74. 8. Rumpakis J. New data on contact lens dropouts: an international perspective. RO. 2010;147(11):37-42. 9. Dumbleton K, Woods CA, Jones LW, et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):92-9. 10. Siddireddy JS, Vijay AK, Tan J, et al. The eyelids and tear film in contact lens discomfort. Cont Lens Anterior Eye. 2018;41(2):144-53. 11. Li W, Yeh TN, Leung T, et al. The relationship of lid wiper epitheliopathy to ocular surface signs and symptoms. Invest Ophthalmol Vis Sci. 2018;59(5):1878-87. 12. Keay L, Edwards K, Stapleton F. An evidence-based brochure to educate contact lens wearers about safe contact lens wear. Clin Exp Optom. 2009;92(5):402-9. 13. Cope JR, Collier SA, Nethercut H, et al. Risk behaviors for contact lens-related eye infections among adults and adolescents—United States, 2016. MMWR. 2017;66(32):841-5. 14. Dart JK, Radford CF, Minassian D, et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology. 2008;115(10):1647-54. 15. Stapleton F, Edwards K, Keay L, et al. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology. 2012;119(8):1516-21. 16. Sauer A, Meyer N, Bourcier T. Risk factors for contact lens-related microbial keratitis: a case-control multicenter study. Eye Contact Lens. 2016;42(3):158-62. 17. Zimmerman AB, Nixon AD, Rueff EM. Contact lens associated microbial keratitis: practical considerations for the optometrist. Clin Optom (Auckl). 2016;8:1-12. 18. Keay L, Edwards K, Naduvilath T, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113(1):109-16. 19. Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115(10):1655-62. 20. Zimmerman AB, Richdale K, Mitchell GL, et al. Water exposure is a common risk behavior among soft and gas-permeable contact lens wearers. Cornea. 2017;36(8):995-1001. 21. Taher EE, Méabed EMH, Abdallah I, et al. Acanthamoeba keratitis in noncompliant soft contact lenses users: genotyping and risk factors, a study from Cairo, Egypt. J Infect Public Health. 2018;11(3):377-83. 22. CDC. Water and contact lenses. www.cdc.gov/contactlenses/water-and-contact-lenses.html. Accessed February 8, 2019. 23. Barnett M, Johns L. Scleral lens complications in contemporary scleral lenses: theory and application. Bentham Science Publisher 2017. Volume 4. Ch. 12:369-82. 24. Dias L, Manny RE, Weissberg E, et al. Myopia, contact lens use and self-esteem. Ophthalmic Physiol Opt. 2013;33(5):573-80. |


