Despite the advances in PRK and LASIK in the past two decades, there are still patients who have complications from these procedures that keep them from experiencing the vision they expected. In these circumstances, contact lenses can help restore vision. However, many individuals who have elected to undergo surgery are often unhappy about the idea of wearing correction again. Therefore, it is important to be both skilled and efficient at fitting contact lenses for this population.
Gas permeable (GP) lenses are a good choice for fitting patients after refractive surgery. These lenses have excellent optics and can mask several diopters of regular and irregular astigmatism. Additionally, the practitioner has complete control over the lens parameters and the lenses can be made in high Dk materials. This article will review GP lens fitting after refractive surgery using a series of case studies.
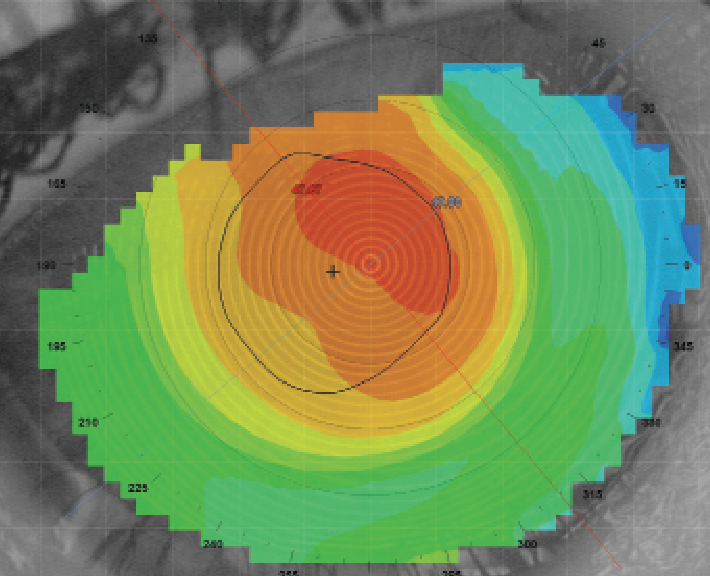 | |
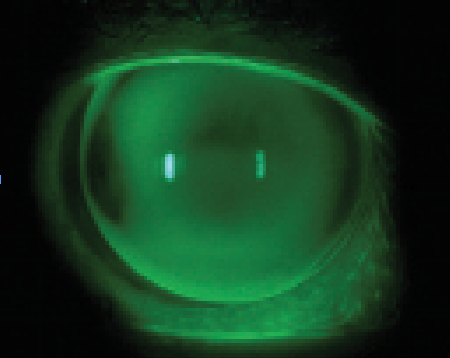
| Fig. 1. Right eye axial power corneal topography post-hyperopic LASIK. | |
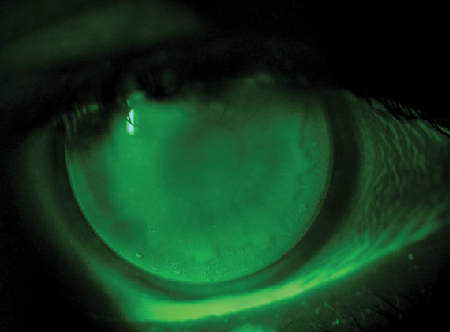 | |
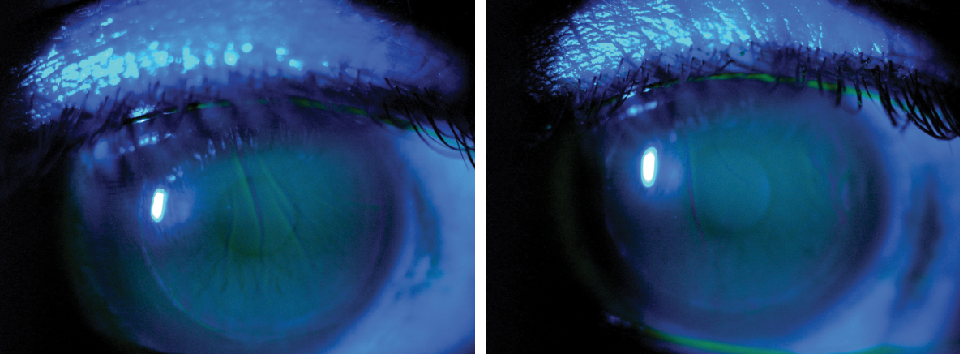
| Fig. 2. A regular geometry tricurve corneal GP lens design on a post-hyperopic LASIK eye. | |
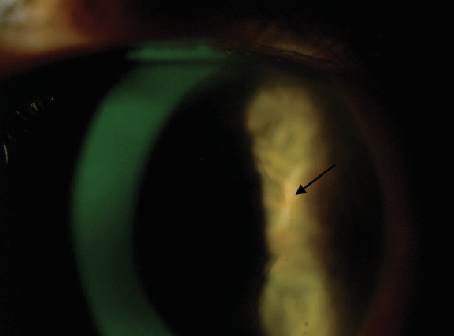 | |
| Fig. 3. LASIK flap interface with fold irregularity OS. Note the arrow, which points towards the defect. |
Corneal Shape Considerations
Fitting patients who have undergone refractive surgery is challenging due to their altered corneal shape. A typical cornea has a prolate shape, i.e., steeper centrally with flattening towards the periphery. The rate of flattening towards the periphery can be described by its eccentricity value. Normal corneas typically have eccentricity values of 0.5 to 0.7.
Hyperopic LASIK/PRK is accomplished by ablating the peripheral cornea in order to steepen the central cornea. These patients have a corneal profile similar to keratoconus and an eccentricity value of greater than 1.0. And so, keratoconic design lenses can be helpful in fitting those who have had a hyperopic procedure done.
Myopic surgery is accomplished by ablating the central cornea in order to make it flatter, which causes the peripheral cornea to steepen. This reverse corneal configuration is oblate in shape and has a negative eccentricity value. A reverse geometry design contact lens can be used to align better with the corneal profile of a patient who has had myopic refractive surgery.
The initial contact lens design after refractive surgery can be determined by looking at the eccentricity value. Values greater than 1.0 could be fit into a keratoconic lens. If the eccentricity value is negative, consider fitting a reverse geometry design.3
Corneal topography can also help practitioners choose contact lens parameters after refractive surgery. The initial base curve of a corneal GP lens can be determined after refractive surgery by taking an average dioptric curvature 4.0mm away from the center on axial curvature maps and 2.0mm on tangential curvature maps.4 Additionally, a height map shows linear distances between positions on the cornea and a reference sphere. This reference sphere over the cornea gives an idea of what the GP fluorescein pattern may look like.5 And so, a base curve calculated from a tangential or axial map could be applied as a curvature reference sphere on a height map to see how a corneal GP lens may fit on the eye.
Corneal GP Lenses
The notable differences in shape present between ablated and non-ablated corneal areas after refractive surgery can make GP lenses challenging to fit. Often, corneal GPs do not exhibit a classic alignment pattern on a surgically altered cornea. Instead, there will be pooling in flatter ablated areas and bearing over the steeper untreated areas. Nonetheless, this may be acceptable as long as there is adequate lens movement and room for a healthy tear pump behind the lens, and if the lens does not cause any harsh areas of punctate erosion.
Hyperopic procedures leave the cornea highly prolate. Patients who have had hyperopic refractive surgery can be fit into keratoconic lens designs.1,3 In contrast, myopic refractive surgery will cause the cornea to become oblate in shape; a reverse geometry design in which the base curve is flatter than the adjacent peripheral curve will align better in oblate corneas.1,3
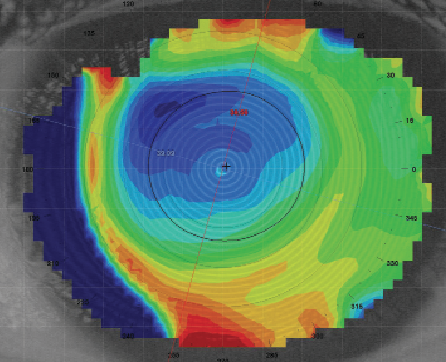 | |
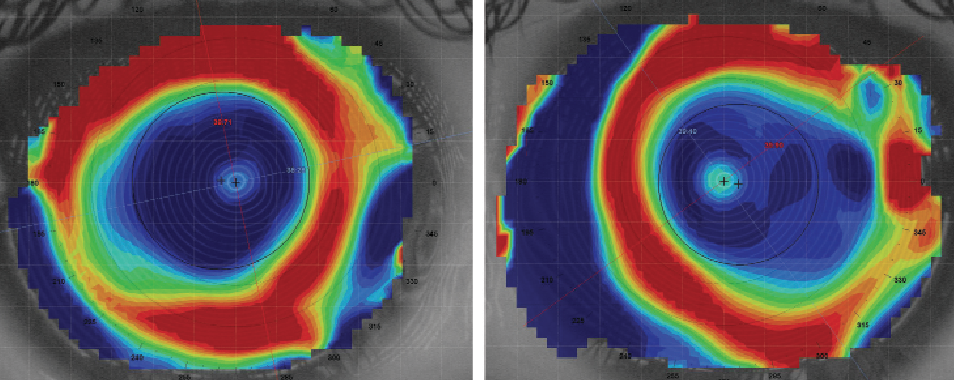
| Fig. 4. Tangential power corneal topography showing oblate-shaped OS cornea after LASIK in a patient with flap fold irregularity. | |
 | |
| Fig. 5. Reverse geometry corneal GP for correction of irregular astigmatism from flap fold after myopic LASIK. |
Iatrogenic corneal ectasia following myopic corneal refractive surgery results in anterior bulging of the ablated cornea to cause a keratoconus-like situation. This poses a unique challenge in fitting corneal GP lenses because the topography will have a combination of steeper areas at the apex of the cone and in the untreated periphery, and will be flatter in the non-ectatic ablated areas. If the apex of the cone is central, a prolate keratoconus design lens can be fitted. In contrast, oblate reverse geometry designs will work better if the apex is decentered. In cases of iatrogenic corneal ectasia, consider a large diameter lens (i.e., greater than 10mm), as the increased size typically centers better over broader areas of irregularity.1
1. Refractive Error After Hyperopic LASIK. A 58-year-old female presented with complaints of blurry vision while reading at near. She had undergone monovision hyperopic LASIK four years prior, during which her right eye was corrected for near reading and her left eye for distance. Although she presented with 20/20 distance vision OU, she could only read J5 at near. Her manifest refraction corrected her to 20/20 and J1 (-0.50-0.75x035 OD and plano OS with a +2.25 add).
Prior to the LASIK procedure, she had been a long-time monovision corneal GP wearer and desired to have her vision corrected with this same modality. Since she was fully corrected for distance in the left eye, we only fitted the right eye. Her topography showed a normal eccentricity value and a topographic keratometry reading of 47.00@40/47.67@130 OD (Figure 1). Because her eccentricity values were normal (steep E value of 0.64 and flat E value of 0.59), she was fit into a regular geometry tricurve corneal GP lens. This lens was fit half a diopter flatter than K. Her final lens parameters were: 46.50/+2.00/9.60 OD, and the lens demonstrated a close-to-alignment fluorescein pattern (Figure 2). She reported successful wear of this lens about three times a week when she wanted to be free of spectacles.
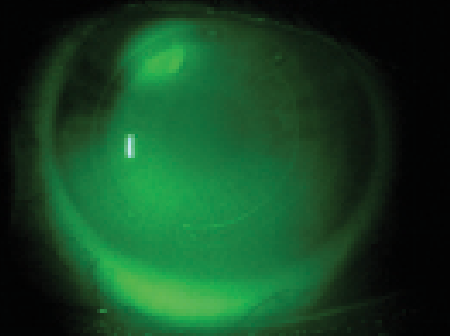
2. Flap Fold Irregularities Corrected with Corneal GP. A 65-year-old female with a history of myopic LASIK presented with complaints of light sensitivity and glare OS while driving at night. These symptoms were caused by irregular astigmatism from a flap fold (Figure 3). Her vision was 20/40 with a spectacle correction of -0.25-0.75x085 and her corneal topography showed an oblate corneal shape with keratometry values of 39.09@164/39.56@074 (Figure 4).
Since her eccentricity value was negative, a 4D reverse geometry corneal GP with the following parameters was trialed: 40.00/plano/10.8. However, the lens ultimately appeared to be about 0.75D too steep with minimal edge lift. A new lens with a flatter base curve and periphery was created with an over-refraction of +0.25D. The final lens parameters were 39.25/+1.00/10.8, and she was able to see 20/20. This lens showed mild apical touch and moderate bearing in the horizontal mid-periphery (Figure 5). Nonetheless, the lens had great movement and good tear exchange, and the patient’s corneal health looked great at subsequent follow-up visits.
The patient was happy with her improved visual acuity and nighttime vision and was able to wear her lens for the entire day.
 | |
| Fig. 6. Multiple stromal folds within a LASIK flap OD (left) and OS (right). | |
 | |
| Fig. 7. Tangential power corneal topography showing myopic ablation profile OU. |
Scleral Lenses
In contrast to fitting corneal GP lenses—a process in which corneal topography is crucial to lens design—a scleral lens has the advantage of being able to vault the cornea and rest on the anatomy of the scleral-conjunctival area. This makes scleral lenses ideal for fitting over highly irregular corneas after refractive surgery, such as in the case of uneven ablation zones or iatrogenic corneal ectasia. These large lenses center well and offer stable vision and good comfort; additionally, their fluid-filled reservoir offers therapeutic applications in the case of LASIK-induced dry eye.6 Scleral lenses are available in both regular and reverse geometry designs.
3. Flap Fold Irregularities Corrected with Scleral Lens. A 31-year-old male presented to the clinic with complaints of seeing glare around lights and decreased vision OU for the past year. The patient has a history of myopic LASIK OU and, within a week of undergoing the procedure, reported being aware of his symptoms. Anterior biomicroscopy revealed multiple LASIK flap folds OD>OS (Figure 6).
His manifest refraction was plano-1.00x065 OD and plano OS, which corrected him to 20/50 and 20/25, respectively. Corneal topography indicated a myopic ablation profile with keratometry readings of 38.26@012/38.71@102 OD and 39.40@126/39.00@036 OS (Figure 7). A 16mm 4.00D reverse geometry scleral lens with a 42.00D base curve and plano power was trialed in both the right and the left eyes. The lens demonstrated excessive vault of 500μm upon insertion over the central corneal surface, and the lens decentered inferiorly OU. Overrefraction values of -9.50D and -7.50D were found in the right and left eye, respectively, which led to the 20/30 OD and 20/20 OS visual acuity. As such, the following flatter lenses with compensated powers were ordered: 40.00/-8.50/16.0 OD and 40.00/-6.75/16.0 OS with a 2.00 D peripheral haptic OU (Figure 8).
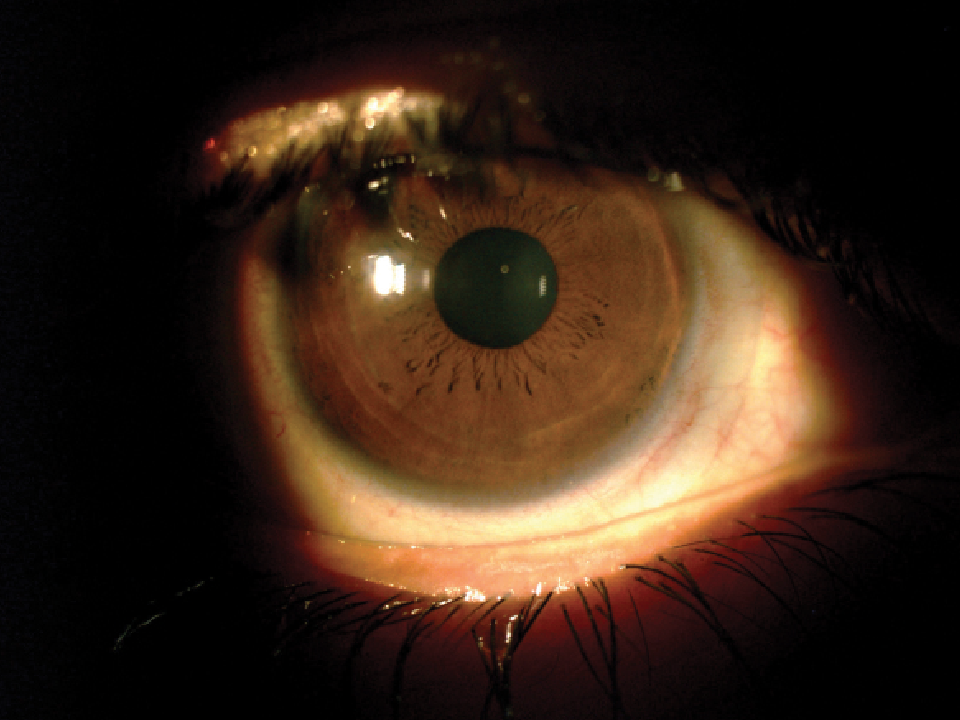 | |
| Fig. 8. A 16mm diameter scleral lens with a toric peripheral haptic over patient with multiple folds of LASIK flap. |
Following dispensing, the lenses centered well and had approximately 250μm of vault centrally after 40 minutes of allowance for settling OU. The lenses were dispensed to the patient and he reported less glare and better quality of vision in both eyes at the three-week follow-up appointment. The patient also had healthy corneas and noted being able to wear the lenses comfortably for 12 hours.
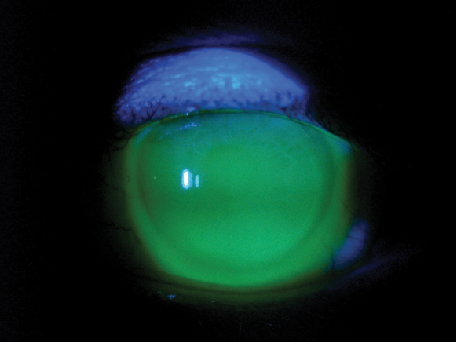
4. Intacs and LASIK-Induced Dry Eye Syndrome. A 54-year-old male with a history of myopic LASIK OS presented to the clinic having formed subsequent iatrogenic corneal ectasia and dry eye four months after the procedure. Additionally, he had undergone intracorneal ring segment implantation in his right eye. The patient admitted to using preservative-free artificial tears once every hour to treat his dry eyes. His keratometry values were 47.25@032/43.12@125. Though he was corrected to 20/25 with a spectacle prescription of -4.25-2.50x140, he desired to be free of glasses.
Due to his dry eye syndrome, he wanted to try a scleral lens to gain some symptomatic relief. A 45.00/-1.50/18.0 lens was trialed and with a -1.00 over-refraction, the patient could see 20/20. This lens also demonstrated adequate vault over the limbus and aligned in the periphery (Figure 9). A final lens was ordered with the parameters of 45.00/-2.50/18.0. The patient reported improved nighttime vision and was able to decrease his drops to application once every four hours.
 | |
| Fig. 9. An scleral lens fit on a patient with iatrogenic corneal ectasia and dry eye syndrome after myopic LASIK OS. This patient also has intra-corneal ring segments in place. | |
 | |
| Fig 10. Tangential corneal topography OU of a patient with dry eye syndrome after myopic LASIK procedure. The patient’s dry eye symptoms were exacerbated by lagophthalmos caused by her systemic Parkinson’s disease. | |
 | |
| Fig. 11. An 18mm diameter scleral lens with 4D reverse geometry used to treat the LASIK- and lagophthalmos-induced dry eye symptoms of the patient from Figure 8. OD lens shown here. |
5. Lagophthalmos Complicates LASIK-Induced Dry Eye Syndrome. A 73-year-old female with a history of myopic LASIK OU 14 years prior was referred in for scleral lens fitting to treat her severe dry eye symptoms. The patient stated that her eyes had remained relatively dry since her LASIK procedure, but that the severity of dryness had increased three years ago with the advancement of her Parkinson’s disease. The patient reported self-administering autologous serum drops hourly, topical steroids BID, preservative-free artificial tears every 15 to 30 minutes, doxycycline hyclate 50mg tablets PO daily and 1,000mg of omega-3 PO daily. Additionally, she had installed humidifiers in all the rooms of her house to help with her dry eye symptoms.
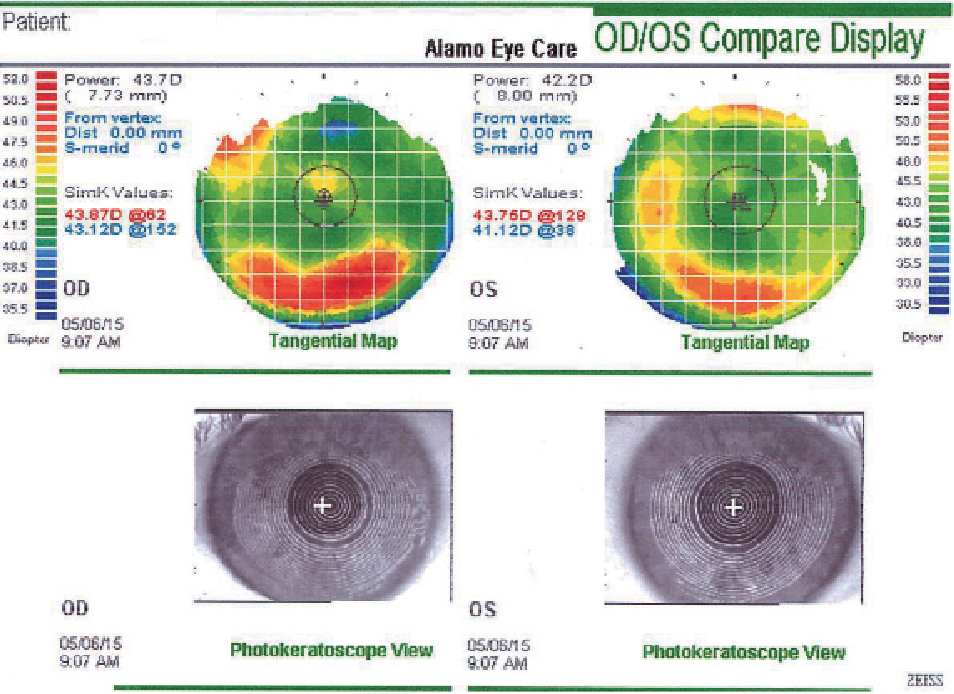
Despite all of these efforts, however, none of the treatments gave her significant relief. Additionally, she stated that her eyes constantly felt like they were “on fire.” A slit lamp examination demonstrated inferior punctate staining and a decreased blink rate of once every 30 seconds. The patient was correctable to 20/20 at distance and J1 at near with a mild hyperopic and astigmatic correction of +0.50-0.75x 040 OD and +0.50-0.75x180 OD with a +3.00 add. Her topography showed a myopic ablation profile OU and keratometry readings of 43.87@062/43.12@152 OD and 43.75@128/41.12@038 OS (Figure 10). The following 4D reverse geometry diagnostic scleral lenses were placed on her eyes: 46.00/-2.00/18.0 OD and 45.00/-1.50/18.0 OS. Following 45 minutes of wear in the office, the patient stated 60% relief of her symptoms. A -3.00D OD and 2.00D OS overrefraction was added to the front surface of the final scleral lens order. The lenses showed good vault over the corneal surface and aligned well with the scleral shape of both eyes (Figure 11). Following one month of wear, the patient stated that her symptoms were completely resolved and that she had discontinued all of her topical drops.
Though most patients who undergo refractive surgery exhibit good visual outcomes, there are still some who need to wear contact lenses afterwards to rehabilitate their vision and/or health of their eyes. Fitting contact lenses after these procedures can be challenging due to altered corneal shape and unenthusiastic patient attitudes about wearing lenses again. Knowledge of the various contact lens designs and the ability to interpret corneal shape after LASIK and PRK is key to helping this population succeed in contact lens wear. In most cases, GP lenses are a great choice and offer relief for surgically altered corneas.
Dr. Frogozo, a fellow of the AAO, is the owner and director of Alamo Eye Care and the Contact Lens Institute of San Antonio in San Antonio, Texas. She specializes in difficult-to-fit contact lenses for both adult and pediatric patients.
1. Steele C and Davidson J. Contact Lens fitting post-laser-in situ keratomileusis (LASIK). Contact Lens and Anterior Eye. 2007 May;30(2):84-93.
2. Garcia-Zakisbak D, Nash D, Yeu D. Ocular Surface diseases and corneal refractive surgery. Current Opinions in Ophthalmology. 2014 Jul;25(4):264-269.
3. Gruenauer-Kloevenkorn C et al. Varieties of contact lens fittings after complicated hyperopic and myopic laser in situ keratomileusis. Eye and Contact Lens .2006 Sep;32(5):233-39.
4. Szczotka-Flynn L, Jani BR. Comparison of axial and tangential topographic algorithms for contact lens fitting after LASIK. Eye Contact Lens. 2005;31:257–62.
5. Rabinowitz YS. “Corneal Topography: Corneal Curvature and Optics, Clinical Applications, and Wavefront Analysis ” Clinical Contact Lens Practice. ES Bennett, BA Weissman. Philadelphia, Lippincott Williams & Wilkins: 215-32.
6. Parminder A, Jacobs DS. Advances in scleral lenses for refractive surgery complications. Current Opinions in Ophthalmology 2015 Jul;26(4):243-248.


