 |  |
Lens comfort often dictates whether a patient will continue with contact lens wear or drop out. Practitioners struggle with the concept of discomfort because the cause is usually multifactorial. If we ask a patient whether they want to wear a soft lens or a hard gas permeable (GP) lens, most say a soft lens. More often than not, patients associate lens comfort with lens material. However, we know that initial lens awareness and discomfort is heavily attributed to lens diameter and edge alignment, not lens material. Numerous factors, such as ocular surface disease, allergies and poor lens wettability, can also contribute to discomfort.
A comfortable initial lens fit is crucial to overcoming a patient’s apprehension with scleral lenses and keeping them happy in the modality long-term. New technologies can help clinicians better assess ocular shape and lens fit, providing patients the optimal all-day comfort they need.
Scleral Shape
When designing the landing zone, pay close attention to the patient’s scleral shape using diagnostic lenses, scleral mapping tools and impression molds.
For the average eye, the ocular surface beyond the cornea is asymmetrical in nature.1 The sclera, similarly to the cornea, may present steep and flat meridians even though corneal and scleral toricity are not associated.2 Based on studies evaluating the shape of the average eye, the nasal portion typically is flatter compared with the rest of the eye.1 Today, many practitioners use asymmetrical lens designs for the majority of their patients to compensate for irregular scleral shape.2
Asymmetrical back surface scleral lenses, such as toric- or quadrant-specific lenses, can eliminate many complications that can lead to discomfort, such as lens decentration, bubble formation and excessive tear exchange that can cause debris inflow.2
Determining the appropriate amount of central clearance and back surface toricity from diagnostic slit lamp findings is a skill that comes with experience and assistance from consultation. But using objective data from mapping tools, such as a scleral topographer, to design a scleral lens may be a more straightforward approach that can minimize the need for additional troubleshooting.
Scleral Profilers
Scleral topographers image both the depth and shape of the cornea and sclera. Information regarding the shape of the eye beyond the cornea is valuable in determining whether toricity is needed in the scleral landing zone. Oftentimes, clinicians underestimate the amount of sagittal depth or toricity needed for the landing zone, resulting in additional follow-ups to make adjustments and an increase in chair time costs.
These instruments may increase the rate of fitting success by providing a better understanding of the shape of the eye and eliminating some guesswork involved with diagnostic lens fittings. They may also help clinicians troubleshoot difficult-to-fit patients, minimize the amount of follow-ups and provide greater efficiency in the lens fitting process.
Currently, three scleral mapping instruments on the market measure the topography of the eye beyond the limbus and create scleral lenses empirically: the sMap3D (Precision Ocular Metrology), the Pentacam Cornea Scleral Profile (CSP, Oculus) and the Eye Surface Profiler (ESP, Eaglet Eye).
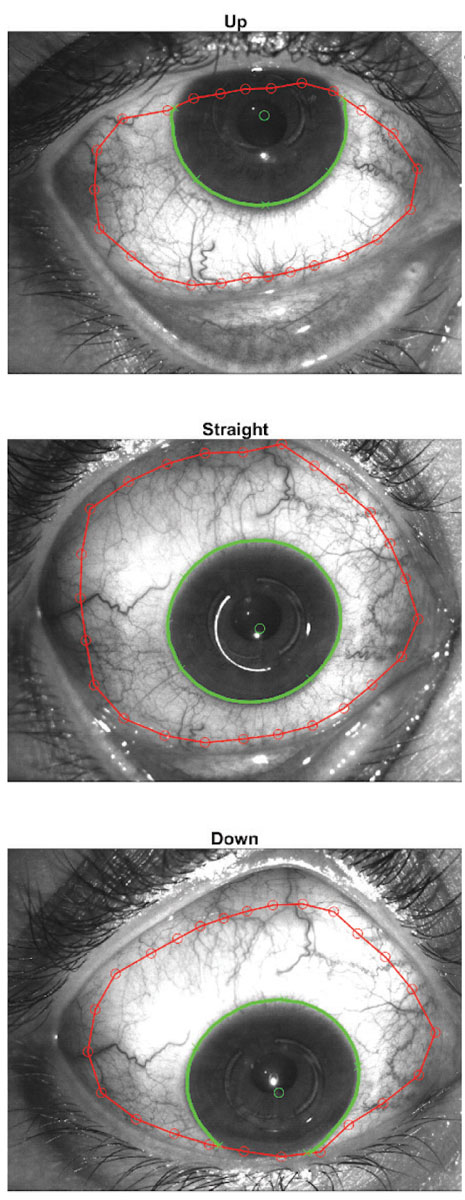 |
Fig. 1. The sMap3D uses three images in multiple gaze directions to create a single image of the ocular surface. Images: Sheila Morrison, OD. Click to enlarge. |
sMAP3D
The sMap3D is a fluorescence-based structured light topographer with a range of more than 22mm and 360° scleral coverage. The sMap3D captures three images in multiple gaze directions that are then stitched together to create a single image of the ocular surface (Figure 1).
The topographer provides many software features, such as simulated fluorescein 3D images to predict how the lens is vaulting over the cornea and how it will align with the scleral surface. Practitioners can use various maps to define sagittal height at any chord and visualize the ocular surface compared with an overlying scleral lens.
After imaging, the clinician can apply a scleral lens to determine the over-refraction. Once the clinician has added all the necessary parameters, the software designs a customized scleral lens that takes into account the amount of scleral toricity necessary and integrates it into the landing curves, if needed. The software designs the best-fit lens based upon the Europa scleral lens (Visionary Optics) to determine initial lens parameters.
Pentacam CSP
This tool measures up to 18mm of the ocular surface as well as the sagittal height for scleral lens fitting for both the cornea and sclera. This streamlines the first trial lens selection of sagittal depth based on measured corneal elevation. Each scan provides anterior segment and scleral topography analysis. The instrument takes five scans with 50 images each in primary gaze for a total of 250 Scheimpflug images. The resulting scan is a tear film–independent measurement. Therefore, it does not require fluorescein.
If a practitioner obtains a poor quality image or inadequate surface area, they can repeat an individual portion of the imaging without repeating the entire process. The goal is to measure as close to 18mm of the ocular surface as possible. Because the CSP software is not lens specific, clinicians can use a variety of lens designs. Another unique aspect to the CSP software is the ability to design a lens using external fitting software, such as Wave (Baush + Lomb).
ESP
This device is a fluorescence-based topographer that captures a single image of the cornea and sclera in primary gaze. Each scan provides more than 350,000 measurement points across a 20mm diameter area with a resolution of 2µm of the cornea, 10µm of the sclera and 0.1D of refractive error. Corneal and scleral curvature data is translated into height maps that are then used to select a lens from the software.3
The ESP software contains more than 30 lens designs, including corneal GPs, sclerals, hybrids, ortho-K and specialty soft lenses. The instrument generates the initial lens diameter based on corneal size, as well as the recommended initial lens sagittal value and amount of toricity in the scleral landing zone for optimal fit.3 The toricity in the landing zone is derived from both scleral shape and total sagittal value of each of the major meridians of the eye, allowing for precise landing in each meridian.3
Clinicians can place the suggested diagnostic lens on the eye, perform an over-refraction and finalize the initial lens order. Also, the ESP software can detect physiological changes related to contact lens wear through its different tangential maps. This is beneficial to monitor for subclinical corneal changes such as corneal edema or corneal warpage.
Despite the technological advancements clinicians have access to with scleral topographers, the information is only as valuable as the accuracy of the image acquired. If a patient has severe dry eye, then data collection may not be optimal. Ultimately, mapping devices in conjunction with diagnostic lens observations can help provide ideal landing zones leading to increased wear time and improved overall comfort.
1. van der Worp E. A Guide to Scleral Lens Fitting, Version 2.0 [monograph online]. Forest Grove, OR: Pacific University; 2015. 2. Jedlicka J, Johns LK, Byrnes SP. Scleral contact lens fitting guide. Contact Lens Spectrum. 2010;25:30-6. 3. Barnett, M. Utilize scleral profilers for scleral lens selection. Contact Lens Spectrum. 2017;25:30-6. |


