Dry eye is easily one of the most common diseases worldwide, encompassing a wide range of ocular surface alterations with different etiologies and pathophysiologies.1,2 In recent years, eye care practitioners have made great advances in objectively measuring dry eye with precision, using high-tech tools to quantify tear osmolarity, inflammatory cytokines and Sjögren’s biomarkers in addition to familiar clinical evaluation tools like the Schirmer’s test and tear film breakup time. Methods to assign an objective number or severity score to dry eye have flourished.
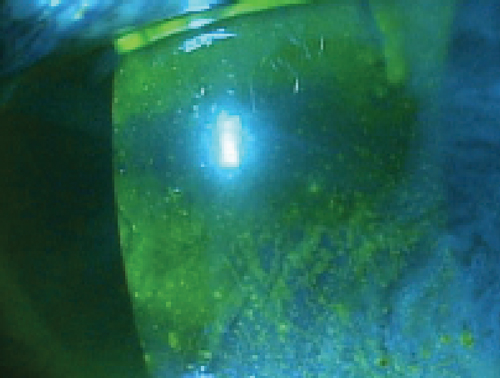 | |
| Does reliance on dry eye signs, like the corneal staining above, overshadow the role of the patient's symptomatic experiences and quality-of-life issues? Photo: Mile Brujic, OD |
But despite this success, the subjective component of the disease—how it feels for patients—remains for the most part poorly documented. Thus, it’s no surprise a number of patient evaluation questionnaires exist as part of an ongoing movement to quantify patient symptomatology. Dry eye questionnaires are commonly used in clinical research to screen participants, grade disease severity and assess the effects of treatments. They vary in length, focus and extent of validation, and often involve a number of rating scales that are combined to produce a total raw score (see “Comparing Notes,” p. 14).13 So, how does one determine which to use in a busy clinical practice, especially given that such questionnaires typically measure patients against a pre-established clinical diagnosis of dry eye?
This article discusses some of the more popular questionnaires available and examines their relevance in the context of evaluating patients in a clinical practice setting.
Expert Testimony
In 2007, the International Dry Eye WorkShop published a report on the epidemiology of dry eye, which evaluated the practicality of a number of dry eye questionnaires.17 Requirements for consideration included that the questionnaire had been used in randomized clinical trials (RCTs) or epidemiologic studies, had passed psychometric testing and been deemed suitable for evaluating general, non-disease specific dry eye populations.17 Fourteen questionnaires met the criteria, including five discussed here.
The committee identified characteristics that designate a questionnaire as suitable for use in epidemiologic studies and RCTs. First, it must be able to detect and measure changes in symptoms with effective treatment or disease progression.17 The recall period must also be specified and the ability to set a threshold of disease severity as an inclusion criterion should be present.17 Additionally, because of the possibility of dry eye symptoms worsening over the course of the day, there must be a single, set time for administering dry eye examinations and the questionnaire.17
The subcommittee recommended adding a better definition of clinically meaningful changes in scores as well as a better concept of the “worst” symptom and a question on visual function with respect to dry eye.17 Also, more research on the relationship between frequency and severity of dry eye symptoms as a means to better identify a clinically meaningful change in symptoms is warranted.17
Comparing Notes: Selected Dry Eye Evaluation Forms • McMonnies Questionnaire. Arguably the first modern dry eye questionnaire, the McMonnies is comprised of 14 items that focus on established risk factors for dry eye including age, sex, contact lens wear, medication use and certain systemic and ocular factors.5 The questionnaire was intended to both determine the presence of dry eye and identify individuals at risk for developing the disease. Several studies validating the McMonnies questionnaire as a means to screen patients for dry eye disease exist.6,7 A separate study evaluating the psychometric properties—reliability, validity and accuracy—of it reported poor internal consistency, moderate test-retest reliability and fair concurrent validity and accuracy.8 The two questionnaires also include questions on the perceived time of day that symptoms worsen, how much the symptoms affect daily activities, computer use, use of systemic and ocular medications, and presence of allergies.9 The DEQ has been successfully evaluated for its use in measuring the frequency and intensity of symptoms of ocular irritation in patients with aqueous tear deficient dry eye.10 Download DEQ here. Download CLDEQ here. • Ocular Surface Disease Index (OSDI). Developed by the Outcomes Research Group at Allergan, the OSDI questionnaire is a self-administered 12-question scale designed to assess a range of ocular surface symptoms, their severity and impact on visual function in a one-week recall period.11 Currently, the OSDI is one of only two validated dry eye questionnaires to include quality-of-life measures for clinical use.12 Download OSDI here. • Subjective Evaluation of Symptom of Dryness (SESoD). The SESoD is a three-item questionnaire created by Allergan to evaluate a patient’s perception of ocular discomfort related to dryness. Together with the DEQ, McMonnies and OSDI, the SESoD has been shown to exhibit unidimensionality—that is, it is comprised of questions that measure specific metrics simply and linearly to yield straightforward values.13 For example, income is a unidimensional variable; socioeconomic status, which includes income, occupation and education, is a multidimensional variable. • Impact of Dry Eye on Everyday Life (IDEEL). The 57-question IDEEL survey from Alcon assesses the effect of dry eye with respect to three primary modules: dry eye symptom bother, impact on daily life (comprising impact on daily activities, emotional state and work) and treatment satisfaction (comprising patient attitude towards treatment effectiveness and treatment-related bother/inconvenience).14 Together with the OSDI questionnaire, the IDEEL survey comprises a small category of dry eye questionnaires that include quality-of-life measures for clinical use.12 Download IDEEL here. A psychometric analysis performed as part of a validation study involving 210 subjects—130 with non-Sjögren's keratoconjunctivitis sicca, 32 with Sjögren's syndrome and 48 controls—found IDEEL to exhibit good consistency and reliability.14 Strong correlation between IDEEL and the Dry Eye Questionnaire was also noted.14 • Standard Patient Evaluation of Eye Dryness (SPEED). The SPEED questionnaire is a four-question survey developed by TearScience to assess frequency and severity of patient dry eye symptoms. In particular, it monitors diurnal and longer-term symptom changes over the course of three months.15 The SPEED questionnaire has been shown to exhibit good validity, unidimensionality, objectivity and consistency when compared with the DEQ, McMonnies questionnaire, OSDI and SESoD.15 Download SPEED here. • Dry Eye-Related Quality-of-Life Score Questionnaire (DEQS). The DEQS is a 15-item questionnaire created to assess the presence of dry eye symptoms and their severity, and the effects of these symptoms on aspects of patients’ everyday lives, including psychological and social aspects.16 A psychometric analysis found the study had good internal consistency, test-retest reliability, discriminant validity and responsiveness to change; thus, the test is valid and reliable for evaluating the multifaceted effect of dry eye disease on a patient’s daily life.16 Download DEQS here. |
What Do You Use?
Granted, dry eye questionnaires are commonly used in clinical research as a means to grade disease severity and assess treatment effects, all within a controlled environment with a pre-selected population segment. But are they useful in clinical practice, where many different patients present who have not been pre-sorted and who may fall within a range of disease severity and treatment types and stages?
A validated questionnaire, says Arthur B. Epstein, OD, provides a good starting point to evaluate the patient’s unique experience and gather information about the specifics of the disease. Dr. Epstein is director of clinical research at Phoenix Eye Care and runs a dry eye clinic at the practice. He uses dry eye questionnaires to evaluate every patient who walks in.
“I use questionnaires for documentation and especially for progress evaluations,” he says. “While both are important, my personal bias is to measure outcomes by a reduction in patients’ symptoms even more than a reduction in physical signs. Questionnaires provide a standardized way of assessing how well the patient is doing and if they are responding to therapy.”
Dr. Epstein uses both the OSDI and SPEED questionnaires, and says each has its own benefits. “SPEED is quicker, but OSDI provides a bit more information. As odd as it sounds, I haven’t totally settled on either, but I make sure we use the same one we used previously to monitor change” in a specific patient.
Overall, he adds, the usefulness of the different dry eye questionnaires varies depending on the patient. “For example, the CLDEQ is optimized for lens wearers, and the DEQS focuses more on quality-of-life issues. Some are research tools and less useful in clinical practice.”
Al Kabat, OD, and Whitney Hauser, OD, of Southern College of Optometry’s TearWell Advanced Dry Eye Treatment Center in Memphis, also use the OSDI and SPEED questionnaires for similar purposes. Because both are validated and used in the practice together, they act as a good system of checks and balances. “We use the questionnaires to first quantify the patient’s symptoms as a finite entity, and then track the patient’s progress as we perform or initiate specific treatment regimens,” Dr. Kabat says.
“Occasionally, patients are influenced by how they feel on a particular day, and the surveys provide a more global view,” adds Dr. Hauser. “Dry eye care, unlike many other eye diseases, is driven by symptom relief, and the surveys give a measureable indication of improvement.”
The responses from the dry eye questionnaires do have a big influence on treatment decisions, Dr. Kabat says. “For a severely symptomatic patient, we are more apt to initiate aggressive therapy even in lieu of significant findings. Likewise, for a patient with less symptomology, we might be more conservative in our treatment algorithm.”
| McMonnies Dry Eye Questionnaire Please answer the following by underlining the responses most appropriate to you: Female / Male 2. Do you ever experience any of the following eye symptoms? 3. How often do your eyes have these symptoms? 4. Are your eyes unusually sensitive to cigarette smoke, smog, air conditioning, or central heating? 5. Do your eyes become very red and irritated when swimming? 6. Are your eyes dry and irritated the day after drinking alcohol? 7. Do you take: antihistamine tablets(2) or use antihistamine eye drops(2), diuretics (fluid tablets)(2), sleeping tablets(1), tranquillizers(1), oral contraceptives(1), medication for duodenal ulcer(1), digestive problems(1), high blood pressure(1), antidepressants(1) or ___________________? (Write in any medication you are taking that is not listed.) 8. Do you suffer from arthritis? 9. Do you experience dryness of the nose, mouth, throat, chest or vagina? 10. Do you suffer from thyroid abnormality? 11. Are you known to sleep with your eyes partly open? 12. Do you have eye irritation as you wake from sleep? From: McMonnies C, Ho A: Patient history in screening for dry eye conditions. J Am Optom Assoc 1987, 58(4):296–301. |
Eric Donnenfeld, MD, a Long Island ophthalmologist who specializes in cataract and refractive surgery, uses OSDI and SPEED to guide diagnostic testing. “All patients who have positive findings on the questionnaire undergo osmolarity and MMP-9 testing,” he says. “We can also assess treatment response by following the patient’s symptomatic improvement on the questionnaire.”
DIY Efforts
Some practitioners choose to create their own dry eye questionnaire. In addition to using the SPEED questionnaire, Paul M. Karpecki, OD, of Koffler Vision Group in Kentucky, also uses a custom one of his own making (shown below).
“The second is a much more extensive questionnaire about dry eye disease that is administered on a clipboard when the patient is placed in the exam lane waiting on the doctor,” he says. Contrary to the SPEED questionnaire, which is used on every patient, the custom form is only used for new patients referred specifically for dry eye disease evaluations. “The SPEED questionnaire initiates a potential dry eye patient workup,” says Dr. Karpecki. “The extensive custom questionnaire actually predicts potential diseases ranging from anterior blepharitis to dry eye to allergic conjunctivitis. It also triggers various treatment options.” Also, its short length allows patients to feel like they are making the best use of their time.
Dr. Karpecki created a custom questionnaire because he felt he “needed more information and didn’t want to have to rely on my memory to ask the right questions of the patient.” It’s a culmination of his 20 years’ experience running a dry eye clinic plus information from research papers and dry eye studies.
Another option is to adapt an existing questionnaire or two. John D. Sheppard, MD, president of Virginia Eye Consultants, uses both the OSDI and SPEED questionnaires, but says “both ask a little less than we’d like to differentiate the different types of ocular surface disease. We all think about dry eye, which is ubiquitous, but also extremely common are MGD and blepharitis as well as ocular allergy.”
Patients who present at Dr. Sheppard’s practice take a modified version of the SPEED questionnaire. “A good supplemental question to ask on the SPEED is, ‘Do your eyes itch?’ Answer choices include: Infrequently; frequently; all the time; it’s driving me crazy. Itching is an important symptom that overlaps between the three most common ocular surface conditions but focuses most on ocular allergy,” Dr. Sheppard says. “Another question that seems to help with blepharitis is, ‘Are your eyelids red?’ with the same frequency qualifiers. Also, ‘Are your eyes burning?’ Burning seems to be something that helps with identifying blepharitis. You can also ask patients about crusting and matting on their lids as well.”
The Ideal
What might the ideal dry eye questionnaire look like? Dr. Epstein says SPEED comes closest. “It’s free, it’s quick, it’s repeatable and it should be used consistently with all dry eye patients. It is also an excellent tool for uncovering dry eye among patients who are ‘silent sufferers’ and don’t realize they have a problem that can be effectively—or more effectively—managed.”
Dr. Kabat agrees about the basic principles of an ideal questionnaire and that the SPEED is one such example, but also offers a more general set of characteristics. “If the questionnaire takes more than three minutes for the patient to complete, then it is impractical. If it takes more than one minute to score, then it is impractical. If it cannot be administered and scored by a technician or assistant, then it is impractical,” he says. “For the physician, there should be no more of a time commitment than glancing at the number and assessing its value relative to the scale.”
Additionally, Dr. Kabat says, it should assess symptom impact on lifestyle and provide a metric for quantifying symptom severity, and should have the ability to be used “as a screening tool for all patients in a practice with interest in dry eye management, or as part of the data/history collection in a specialty dry eye practice.”
The ideal dry eye questionnaire should also cover certain symptoms. “Key symptoms must be included such as blurred or transient blurred vision, dryness/grittiness, irritation, burning and watering,” Dr. Karpecki says, and also include severity, frequency and which eye drops are currently being used.
Dr. Donnenfeld adds, “We want to know the patient’s ability to function at normal tasks.”
Dr. Sheppard envisions the development of something more technologically advanced. “I would have a questionnaire that the patient could fill out at home in a reproducible format that we could then plug in digitally when they walk into the office with essentially no effort on the part of the technician,” he says. “The information would then appear as a global score on the chart, with maybe a bar graph read-out that tells us this is aqueous deficiency, this is lipid deficiency, this is blepharitis, this is allergy.” Historical data could then portray the progression or resolution of important complaints in one readout, he says.
Ultimately, the choice of which—if any—dry eye questionnaire depends on practitioner preference. But no matter what, “providing surveys to patients about their symptoms demonstrates a sense of empathy for their condition that many practitioners fail to do,” Dr. Hauser says. “Often, dry eye patients feel as if they are relegated to an afterthought by their doctors. The patients recognize that their activities of daily living have been inhibited, if not devastated, by ocular surface disease, and they appreciate the attention to their plight.”
1. Gayton JL. Etiology, prevalence and treatment of dry eye disease. Clin Opthalmol. 2009; 3:405-12. www.ncbi.nlm.nih.gov/pmc/articles/PMC2720680/
2. Savini G, Prabhawasat P, Kojima T, et al. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008 Mar;2(1):31-55.
3. Bjerrum KB. Test and symptoms in keratoconjunctivitis sicca and their correlation. Acta Ophthalmol Scand 1996;74:436–41.
4. Hay EM, Pal TB, et al. Weak association between subjective symptoms of and objective testing for dry eyes and dry mouth: results from a population based study. Ann Reum Dis 1998;57:20–4.
5. McMonnies CW. Key questions in a dry eye history. J Am Otpom Assoc. 1986 Jul;57(7):512-7.
6. McMonnies CW, Ho A. Patient history in screening for dry eye conditions. J Am Optom Assoc. 1987;58:296-301.
7. McMonnies CW, Ho A. Responses to a dry eye questionnaire from a normal population. J Am Optom Assoc. 1987:58:588-591.
8. Nichols KK, Nichols JJ, Mitchell GL. The reliability and validity of McMonnies Dry Eye Index. Cornea. 2004 May;23(4):365-71.
9. Begley C, Chalmers RL, Mitchell GL et al. Characterization of Ocular Surface Symptoms from Optometric Practices in North America. Cornea 2001;20(6):610-18.
10. Begley CG, Caffery B, Chalmers RL, et al. Use of the Dry Eye Questionnaire to Measure Symptoms of Ocular Irritation in Patients with Aqueous Tear Deficient Dry Eye. Cornea 2002;21(7):664-70.
11. Walt JG, Rowe MM, Stern KL. Evaluating the functional impact of dry eye: the Ocular Surface Disease Index [abstract]. Drug Inf J. 1997;31:1436.
12. Grubbs JR Jr, Tolleson-Rinehart S, Huynh K, Davis RM. A review of quality of life measures in dry eye questionnaires. Cornea. 2014 Feb;33(2):215-8.
13. Simpson TL, Situ P, Jones LW, et al.. Dry eye symptoms assessed by four questionnaires. Optom Vis Sci. 2008;85:692–699.
14. Espindle D, Simpson T, Nelson J, et al. Development and validation of the impact of dry eye on everyday life (IDEEL) questionnaire, a patient-reported outcomes (PRO) measure for the assessment of the burden of dry eye on patients. Health Qual Life Outcomes. 2011 Dec 8;9:111.
15. Ngo W, Situ P, Keir N, et al. Psychometric properties and validation of the Standard Patient Evaluation of Eye Dryness questionnaire. Cornea. 2013;32(9):1204-10.
16. Sakane Y, Yamaguchi M, Yokoi N, et al. Development and validation of the Dry Eye-Related Quality-of-Life Score questionnaire. JAMA Ophthalmol 2013 Oct:131(10):1331-8.
17. The Epidemiology of Dry Eye Disease: Report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007). The Ocular Surface. April 2007;5(2):93-107.


