  |
When deciding which contact lens modality is the best for a patient, contact lens specialists always consider curvature of the cornea, contact lens diameter and ocular surface conditions; however, the eyelids are often easily forgotten. The lids are taken into account when evaluating for blepharitis or meibomian gland dysfunction, but they may be an afterthought during a contact lens evaluation. When fitting GP lenses—whether corneal, intralimbal or scleral—it is important to evaluate lid position in relation to the cornea. The eyelids play a vital role in how a lens will fit and what options will be possible when troubleshooting a problem lens fit or potential design.
Positioning Corneal GPs
In our approach to fitting corneal GP lenses, practitioners tend to provide an apical alignment fit with slight upper lid attachment. In cases where a patient may have extremely taut lids, this may cause the lens to ride higher than average and result in corneal molding due to the pressure provided by the superior lid. Modifications in overall diameter or base curve of the lens may be necessary to bypass these issues. On the contrary, patients with dermatochalasis may have the opposite problem in that the lens sits low or decenters due to the narrowed palpebral aperture and reduced elasticity of the skin.1 In these patients, it may be necessary to consider a scleral instead, to prop the lid up and provide better overall centration.
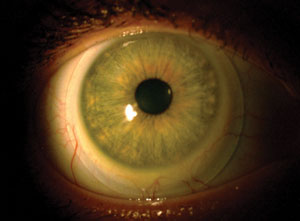 |
| Fig. 1. The natural tendency of a scleral lens to decenter inferiorly can be exacerbated in patients with tighter lids or a narrow palpebral aperture. |
 |
| Fig. 2. A decentered lens results in asymmetrical clearance, with the greatest amount noted inferiorly. |
In presbyopic patients, inferior lid position is important for proper orientation and lens movement. The lid position is also crucial in determining whether an aspheric, concentric or translating design will be successful for the patient. When considering an aspheric lens, the best candidates are those with lower lid margins well above or below the limbus, loose lids that will not support prism ballast or those with steep corneal curvatures.2 As with any multifocal, centration and minimal movement is critical for providing optimal vision with less aberrations at all distances. Good candidates for a concentric or translating design are those with a lower lid margin tangent to or slightly above the lower limbus, a normal-to-large vertical fissure width and normal-to-tight lid tension.2 Loose lids will not do well with these lenses, as they limit translation of the lens, preventing the patient from seeing through the full reading add.
Lids and Sclerals
Eyelids also play a role in the way a scleral contact lens fits on an eye. Naturally, scleral lenses have a tendency to decenter inferiorly. This can be exacerbated by having tighter lids or a narrow palpebral aperture (Figure 1). When fitting scleral lenses, hypoxia and corneal edema are two complications practitioners need to watch for closely. A decentered lens results in asymmetrical clearance throughout the lens, with the greatest amount of clearance inferiorly (Figure 2). This can lead to a decrease in oxygen permeability inferiorly, making hypoxia and corneal edema more of a concern.
Even after exhausting troubleshooting options such as incorporating toric peripheral landing curves, decreasing overall clearance or decreasing the overall contact lens diameter, sometimes the lens will continue to sit lower than normal because of lid positioning. In situations such as this, practitioners may have to leave the fit as is, as long as adequate central corneal and limbal clearance is provided. It is important to minimize lens thickness and use the highest Dk lens materials to allow better oxygen transmissibility. It is also crucial to provide closer follow-up care and thorough patient education on symptoms that could indicate hypoxic conditions.
Fitting front surface toric lenses is another instance in which the eyelids can affect a scleral lens fit. If an overrefraction indicates the need for astigmatic correction, a front surface toric may be needed. To stabilize the lens on the eyes, double slab-off ballasting stabilization can minimize rotation. Unfortunately, eyelids can have an effect on lens rotation, making it difficult to achieve stabilized vision.3
According to one expert, front toric against-the-rule cylinders will naturally align on axis in eyes that have eyelid margins that oppose each other in the vertical meridian due to the thin zones at 6 and 12. If the eyelids oppose more obliquely, the lens will rotate obliquely.3 This is important when the lens continues to rotate out of position despite toric peripheral landing curves and good centration of the lens.
There are several ways eyelids can affect lens position and fit. However, it is important to keep in mind the changes gas permeable lenses can have on the eyelids with prolonged lens wear. Research reports non-senile blepharoptosis, or drooping of the upper lid, as a complication of long-term contact lens wear.4 Ptosis results from dysfunction of either the levator palpebrae superioris or Müller’s muscle, which are responsible for elevation of the eyelids.
Etiologies for ptosis include neurogenic, myogenic, mechanical and aponeurogenic mechanisms. The most common acquired form is aponeurotic, in which disinsertion or dehiscence of the levator aponeurosis leads to ptosis.4,5 This form is often associated with age, ocular surgery and contact lens wear. Patients typically present with mild to moderate ptosis of one or both eyes, good levator function and elevated lid crease.6
There are two main theories for the mechanism behind contact lens–induced ptosis. The first involves the manipulation of the upper eyelid during contact lens removal. The pulling of the eyelid laterally followed by a harsh blink can lead to thinning of the levator aponeurosis.6 Research shows eyelid irritation and edema from constant interaction with the contact lens edge can lead to a reversible ptosis.7
Figure 3 demonstrates a patient who has worn gas permeable contact lenses for over 20 years. Her history consisted of mild keratoconus in the right eye and prior radial keratometry surgery in the left.
She has worn lenses that were two different sizes to allow for better centration and overall alignment on the cornea. As evident in Figure 3, the degree of blepharoptosis is different between the two eyes, with the left eye having a greater degree.
Lid manipulation during insertion and removal along with the amount of lid interaction with the lens could cause the asymmetrical blepharoptosis noted.
Ranges vary per study, but prolonged GP contact lens wear is the only identifiable cause of ptosis in up to 47% of patients under the age of 50.6,8 Studies also suggested there is an increased risk of blepharoptosis in soft contact lens wearers compared with non-wearers.9 While the percentage may seem high, the average duration of contact lens wear was 15 years, and not all patients are symptomatic.8 Unless the superior visual field is obstructed, surgical intervention is not typically warranted.
1. Benjamin WJ, Borish IM. Physiology of aging and its influence on the contact lens prescription. J Am Optom Assoc. 1991;62(10):743-753.
2. Bennett ES, Weissman BA. Clinical contact lens practice. Philadelphia: Lippincott; 1991.
3. van der Worp E SS. A Guide to Scleral Lens Fitting: College of Optometry, Pacific University. 2010.
4. Friedman NJ, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 3rd ed. Philadelphia: Elsevier; 2009.
5. Watanabe A, Araki B, Noso K, et al. Histopathology of blepharoptosis induced by prolonged hard contact lens wear. Am J Ophthalmol. 2006;141(6):1092-6.
6. Thean JH, McNab AA. Blepharoptosis in RGP and PMMA hard contact lens wearers. Clin Exp Optom. 2004;87(1):11-4.
7. Jupiter D, Karesh J. Ptosis associated with PMMA/rigid gas permeable contact lens wear. CLAO J. 1999;25(3):159-62.
8. Kersten RC, de Conciliis C, Kulwin DR. Acquired ptosis in the young and middle-aged adult population. Ophthalmology. 1995;102(6):924-8.
9. Kitazawa T. Hard contact lens wear and the risk of acquired blepharoptosis: a case-control study. Eplasty. 2013;13:e30.


