 |  |  |
We often welcome each year by reflecting on the preceding 12 months to identify changes we can make to enhance our lives, personally and professionally. Instead of looking backwards, though, let’s shift our focus forward to 2019 to pinpoint what opportunities we can capitalize on to enrich the lives of our patients. With the myopia pandemic continuing to worsen—the prevalence in the United States has increased by 66% from the 1970s to the early 2000s, and by 2050 half of the world’s population will be myopic—this year is the perfect time for optometrists to implement myopia management into their practices.1,2
It’s time to rethink myopia. For decades, we’ve thought of myopia as a refractive error and failed to acknowledge the extent of the impact the condition can have on patients. Myopes face an economic burden to satisfy their visual correction needs, experience a reduced quality of life and are at increased risk for ocular health conditions.3,4 While our priorities tend to gravitate toward higher levels of myopia, it is important to recognize that even a -1.00D prescription doubles the risk of glaucoma and triples the risk of retinal detachment (Table 1).4
We must see myopia for what it is: a progressive disease associated with long-term risks. With the multitude of technology, tools, research and information available to us, it would be a shame not to dive in to myopia management.
Identify and Treat
Many additive factors contribute to the development and progression of myopia, including genetics, minimal time spent outdoors, increased near demand and binocular vision characteristics.5
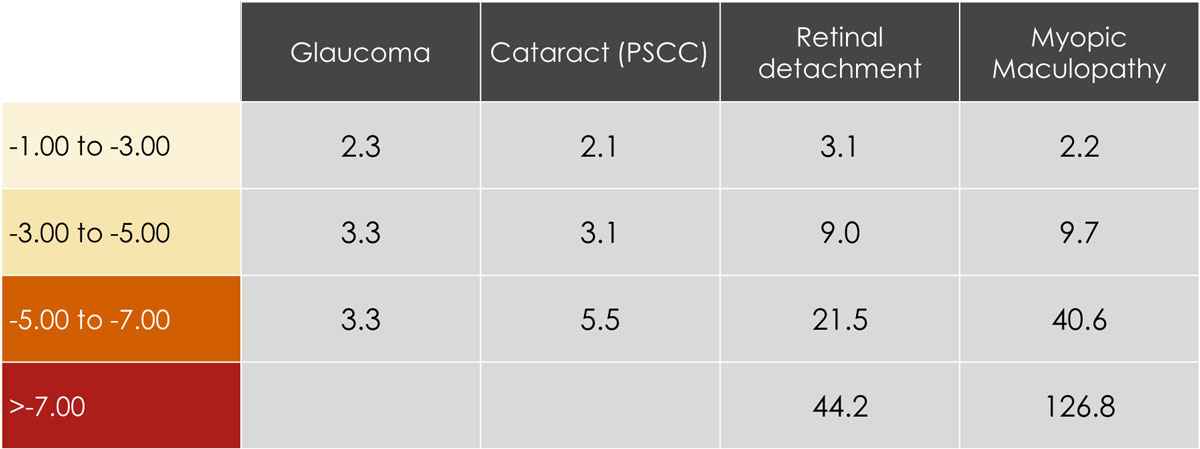 |
| Table 1. Odds ratios of different ocular health risks associated with increasing myopia.4 |
Emmetropia typically occurs when a patient is six to eight years old. Any amount of myopia preceding this age range is outside the norm and increases the likelihood of a higher myopic prescription later on.5,6 It is important to monitor existing myopes for changes of -0.50D or more over a one-year span, as these indicate myopic progression. Treatment should be initiated at the onset of myopia, regardless of the patient’s age. The most effective and widely used forms of myopia management include orthokeratology (ortho-K) lenses, center-distance soft multifocal contact lenses and topical atropine eye drops.
When a myopic eye is corrected with spectacles or single-vision contact lenses, central rays are focused on the fovea, while peripheral rays are focused behind the eye. This peripheral hyperopic defocus is thought to stimulate axial elongation. While the mechanism by which atropine slows myopic progression is not yet fully understood, we know that the goals of ortho-k and multifocals are to address and correct for hyperopic peripheral defocus and provide adequate central vision. Inducing peripheral defocus decreases eye elongation and slows myopic progression.
Ortho-k Lenses
While ortho-K has been shown to slow axial length (AL) progression by 52% and is the primary myopia management technique for many practitioners, it may not be successful in every patient.7 Patients with greater than -4.00D of myopia, -1.75D of with-the-rule astigmatism or -1.00D of against-the-rule astigmatism tend to be more difficult fits. When working outside of these parameters, however, experienced ortho-K fitters regularly achieve great fits.
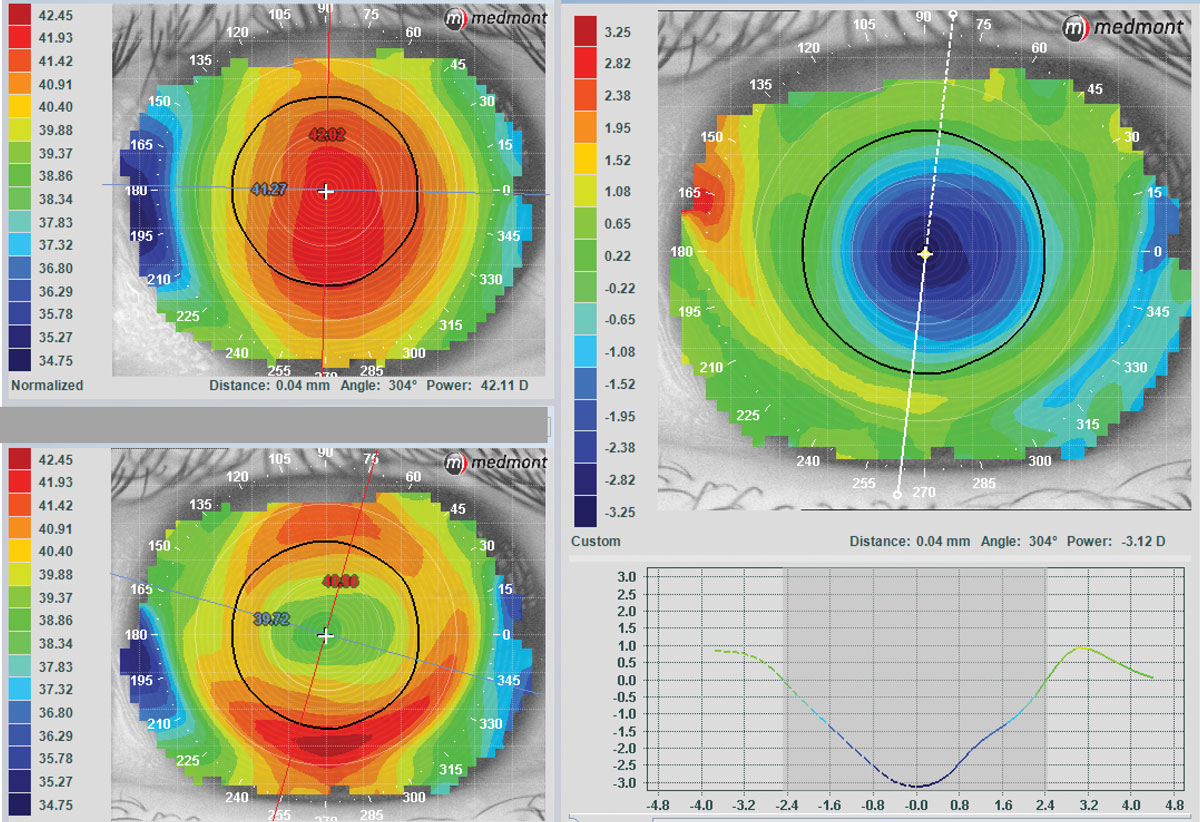 |
| Note the centration of the lens, bull’s-eye pattern and textbook “V” pattern of AL change in this ideal ortho-k fit. Photo: Randy Kojima and Patrick Caroline, Pacific University College of Optometry. Click image to enlarge. |
Despite having limited experience, new fitters have also shown impressive success rates. With the help of empirical fitting techniques, optometrists who have no previous ortho-K experience achieved 80% success on the first ordered lens.8 If they were unsuccessful with one lens, 95% were successful after one lens change and 99.5% after two lens changes.8
A successful ortho-K fit has been described as having good centration over the pupil, a bull’s-eye fluorescein pattern when the lens is on the eye, a bull’s-eye topographic pattern and acuities of 20/25 or better. Limiting myopic progression has been shown to be dependent on the relationship between the pupil size and the optic zone of the ortho-K lens—if the optic zone is much larger than the pupil, the peripheral hyperopic defocus may not be adequately corrected, making it important to maximize “plus in the pupil.”9
Soft Multifocals
Similar to ortho-K, studies investigating the effectiveness of multifocals in managing myopia have shown a reduced AL progression of up to 49%.10 These lenses are ideal for patients who present with high refractive errors. In our clinic, we use a center-distance daily disposable soft multifocal with a gradient +3.00 add. For patients with excess cylinder, spectacles can be worn over multifocals to provide improved clarity. This treatment option can be easily integrated into a practice already familiar with soft contact lenses.
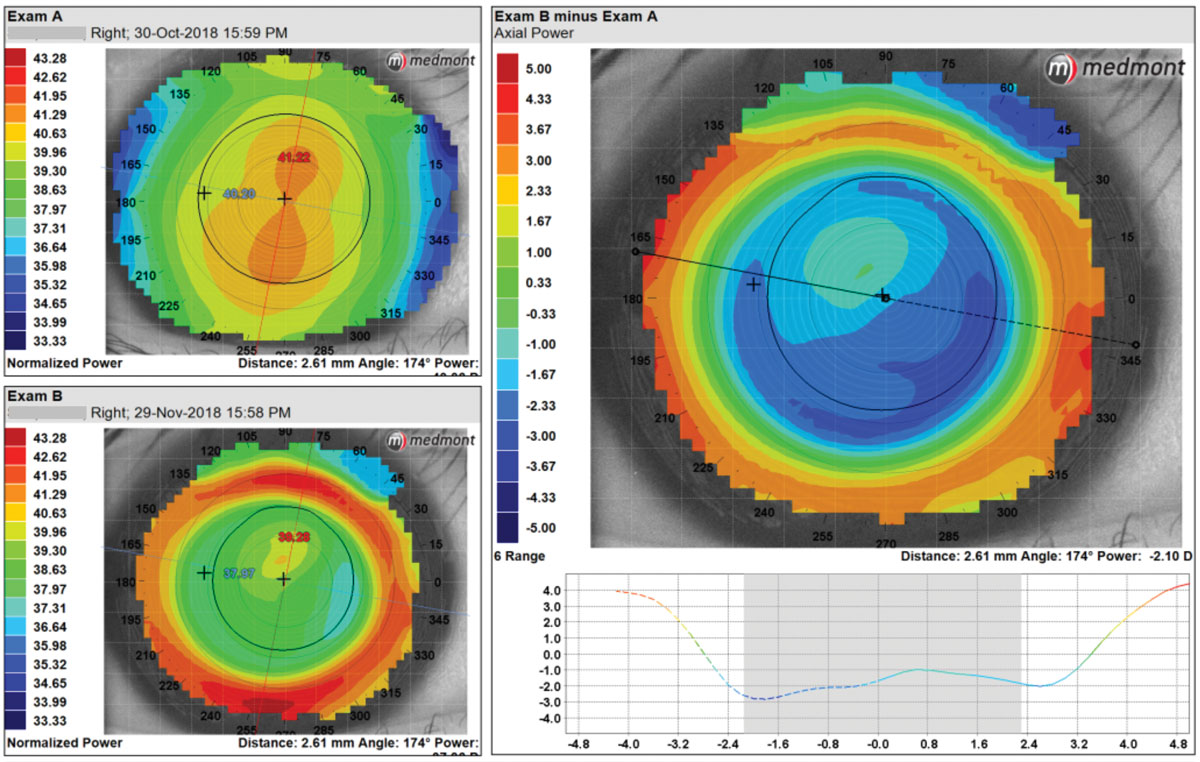 |
| Centrally, this patient has an irregular treatment zone with an optical zone that is too large and would not provide adequate “plus in the pupil.” The optical zone parameters were switched from 6.0mm to 5.4mm for a better fit. Click image to enlarge. |
Atropine Drops
Topical atropine has been shown to reduce the progression of myopia in children, with one study finding that 1% atropine had a 77% reduction in refractive progression and prevented AL progression after two years.11 As expected, however, 1% atropine had significant side effects, including near blur and photophobia.11 Another study compared the effects of various concentrations of atropine on myopia progression and concluded that a once-daily dose of 0.01% atropine had the most significant effect on slowing myopia progression.12
Currently, many clinicians have accepted 0.01% atropine as the standard dosage for myopia management. Some argue that since the second study mentioned above reported a decrease in refractive progression rather than AL progression, 0.01% atropine should not actually be the concentration of choice. In reality, long-term use of a higher concentration may stave off AL progression more effectively.13
When presenting myopia management options to patients and their parents, it is important to set realistic goals and expectations. Be open and honest by acknowledging that, while we do everything we can to decrease AL progression, it is not always possible to stop myopia in its tracks. As optometrists, we pledge to maintain or enhance the general health of our patients. By recognizing myopia as an ocular disease and taking the necessary steps to limit its progression, our patients can enjoy a lifestyle free, for the most part, of the ocular risks associated with high myopia.
|
1. Vitale S, Sperduto RD, Ferris III FL. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632-9. 2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 3. Resnikoff S, Pascolini D, Mariotti SP, et al. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bulletin of the World Health Organization. 2008;86:63-70. 4. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-60. 5. Gifford K. Preparing your practice for the myopia control stampede. Cont Lens Spec. 2016;31:20-3, 25, 55. 6. Flitcroft DI. Emmetropisation and the aetiology of refractive errors. Eye (Lond). 2014;28(2):169-79. 7. Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE Study). Invest Ophthalmol Vis Sci. 2013;54:6510-7. 8. Davis RL, Eiden SB, Bennett ES, et al. Stabilizing myopia by accelerating reshaping technique (SMART)-study three year outcomes and overview. Adv Ophthalmol Vis Syst. 2015;2(3). 9. Chen Z, Biu L, Xue F, et al. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012;89(11):1636-40. 10. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152-61. 11. Chua W, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113(12):2285-91. 12. Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eye drops. Ophthalmology. 2016;123(2):391-9. 13. Yam JCS, Jiang Y, Tang SM, et al. Low-concentration atropine for myopia progression (LAMP) study. Ophthalmology. 2019;126(1):113-24. |


