 |
Cyclosporine, a nonsteroidal immunomodulator that acts primarily by inhibiting T-cell proliferation, is well known to all eye care practitioners. Formulated as an emulsion in a concentration of 0.05%, this drug is FDA-approved to increase tear production in patients for whom it is suppressed, presumably due to ocular inflammation associated with dry eye syndrome.1
As the theme of this month’s edition focuses on anti-inflammatory pharmaceuticals, let’s discuss some nontraditional uses of cyclosporine and the use of medications off-label.
What is “Off-label”?
Before discussing the meaning of “off-label,” we must first define the term “on-label.” It describes a specific use for which a drug has satisfied safety and efficacy tests and received FDA approval. It is expensive and time-consuming for pharmaceutical companies to obtain multiple on-label drug indications; trials can take seven to 10 years and cost millions of dollars. Additionally, once a drug becomes generic, motivation to obtain other on-label indications decreases even further.
Once a drug is FDA-approved, physicians often prescribe it for conditions, population segments or doses other than what it was approved for—all of which constitute “off-label” use.2 For example, 75% of prescription drugs have no indications for children, so off-label use is often necessary. Pregnant women and nursing mothers are also often not included in drug studies.
Off-label use is generally legal; the FDA even states, “Once a [pharmaceutical] product has been approved for marketing, a physician may prescribe it for uses in treatment regimes of patient populations that are not included in the approved labeling.”3 However, practitioners should inform themselves about the drug prior to prescribing. The acid test is whether the use meets the “standard of practice” among eye care practitioners.4 In any case, regulations prevent manufacturers from endorsing the off-label use.
Keratoconus
Elevated levels of proinflammatory cytokines and matrix metalloproteinases (MMPs) have been shown to be present in the tears of patients with keratoconus. Corneal epithelial cells of keratoconic patients also demonstrate upregulation of some of these cytokines.5,6
In one study, keratoconus patients were separated into a control group and study group treated with cyclosporine 0.05% twice a day for six months. Researchers found MMP-9 levels, which had been significantly elevated at baseline, were reduced to levels comparable to the negative controls at the end of the study.
Interestingly, some patients who received cyclosporine showed corneal topographic changes, including focal flattening of corneal curvature, after six months’ use. Others did not manifest these changes, but also didn’t show evidence of disease progression. Researchers concluded that cyclosporine may be an effective treatment strategy for patients with keratoconus.7
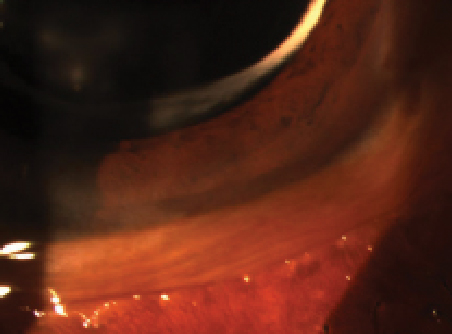 | |
| Conjunctivochalasis may respond to topical cyclosporine. |
Conjunctivochalasis
This condition manifests as loose, redundant, nonedematous bulbar conjunctival tissue; the presentation is typically bilateral and usually inferior. It may also occur nasally and centrally, but is usually noted temporally. The mechanism of onset is thought to be thinning or loss of Tenon’s capsule. Risk factors include dry eye and a history of ocular surgery. Patients with this condition often present with focal pain in the affected area that is exacerbated with eye movement or lid closure. This pain can often be reproduced by applying pressure to the eyelid using a finger. The patient should then be directed to look up and down.
Conjunctivochalasis often needs to be differentiated from dry eye.8 Two recent epidemiological studies in Chinese populations reported prevalence rates of 44% and more than 98%, respectively, in patients older than the age of 60.9,10 Despite the large discrepancy in these findings, conjunctivochalasis is common in the elderly. A separate Chinese study evaluated the impact this condition has on vision-related quality of life using several standardized questionnaires. Patients with conjunctivochalasis had a more significant decrease in tear film stability compared to those with dry eye.11
Tear MMP-9 levels are elevated in patients with conjunctivochalasis, and surgical intervention decreases inflammation.8 Others have proposed that the degeneration of the elastic fibers might be worsened by the presence of pro-inflammatory cytokines such as IL-1ß, TNF-α, IL-1 and IL-6.12,13 Because of the presence of these inflammatory components, conservative treatment of conjunctivochalasis should include pharmacologic intervention. In particular, cyclosporine may useful because of its inhibitory effect on these proinflammatory cytokines. Topical steroids and NSAIDs have also been advocated. If meds prove ineffective, surgical approaches also exist for managing this condition when moderate to severe.8
Adenoviral Conjunctivitis
Adenoviral conjunctivitis is a common and highly contagious infection. Following a two-day to 14-day incubation period, initial signs include conjunctival hyperemia and edema. Keratitis may develop and, after a period of two weeks in some cases, subepithelial infiltrates (SEIs) may appear. These infiltrates may affect vision clarity, as they often appear centrally. Histologically, SEIs are composed of lymphocytes, histiocytes and fibroblasts, which may also disrupt collagen within Bowman’s layer. These SEIs may persist for months, or even as long as a year.14
Three studies demonstrate that cyclosporine is an effective treatment for SEIs associated with adenoviral conjunctivitis.15-17 Two of the studies evaluated a concentration of 1%, which is stronger than what is commercially available in the United States; however, this concentration could be prepared by a compounding pharmacy. Despite this wrinkle, the findings from these studies do warrant consideration of cyclosporine for treating SEIs.
Note, there have been concerns about the possibility of promoting increased viral shedding due to the use of cyclosporine, but by the time the SEIs appear, viral shedding has often ceased, so benefits ultimately appear to outweigh the risks.18
Other Potential Uses
In a small study (n=12), patients with chronic, recalcitrant follicular conjunctivitis were treated with cyclosporine 1%. Researchers observed a reduction in inflammation after one month of use; however, because of the small sample size, further investigation is warranted.19
Another small pilot study (n=20) evaluated cyclosporine 0.05% when administered to patients with ocular prosthetics twice a day for three months. All patients reported marked improvement in their symptoms after one month, and Schirmer tear test objectively improved at the three-month follow-up.20
In conclusion, using the literature to help guide the use of cyclosporine for off-label indications can provide an additional approach to managing inflammation with a safe nonsteroidal alternate.
1. US FDA. Restasis Highlights of Prescribing Information. Available at: www.accessdata.fda.gov/drugsatfda_docs/label/2013/050790s021lbl.pdf.
2. Fugh-Berman A, Melnick D. Off-label promotion, on-target sales. PLoS Med. 2008 Oct ;28;5(10):e210.
3. Wilkes M, Johns M. Informed consent and shared decision-making: a requirement to disclose to patients off-label prescriptions. PLoS Med. 2008;11;5(11):e223.
4. Wilkes M, Johns M. Informed consent and shared decision-making: a requirement to disclose to patients off-label prescriptions. PLoS Medicine 2008 Nov 11;5(11):e223.
5. Balasubramanian SA, Mohan S, Pye DC, et al. Proteases, proteolysis and inflammatory molecules in the tears of people with keratoconus. Acta Ophthalmol. 2012;90:e303–9
6. Lema I, Sobrino T, Duran JA, et al. Subclinical keratoconus and inflammatory molecules from tears. Br J Ophthalmol. 2009 Jun;93(6):820–4.
7. Shetty R, Ghosh A, Lim R, et al. Elevated expression of matrix metalloproteinase-9 and inflammatory cytokines in keratoconus patients is inhibited by cyclosporine a. Invest Ophthalmol Vis Sci. 2015 Feb3;56(2):738-50.
8. Acera A, Vecino E, Duran J. Tear MMP-9 levels as a marker of ocular surface inflammation in conjunctivochalasis. Invest Ophthalmol Vis Sci. 2013 Dec;54(13):8285-91.
9. Zhang X, Li Q, Zou H, et al. Assessing the severity of conjunctivochalasis in a senile population: a community-based epidemiology study in Shanghai, China. BMC Public Health. 2011 Mar; 11(198).
10. Mimura T, Yamagami S, Usui T, et al. Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol. 2009 Jan;147(1):171-177.
11. Le, Q, Cui X, Xiang J, et al. Impact of conjunctivochalasis on visual quality of life: community population survey. PLoS One. 2014 Oct 20;9(10).
12. Acera A, Rocha G, Vecino E, et al. Inflammatory markers in the tears of patients with ocular surface disease. Ophthalmic Res. 2008 Oct;40(6):315-21.
13. Latkany R. Dry eyes: etiology and management. Curr Op Ophthalmol. 2008 Jul;19(4):287-91.
14. Yanoff M, Duker JS. Ophthalmology 4th Ed. 2014. Elsevier.
15. Jeng B, Holsclaw D. Cyclosporine A 1% eye drops for the treatment of subepithelial infiltrates after adenoviral keratoconjunctivitis. Cornea. 2011 Sept;30(9):958-61.
16. Levinger E, Slomovic A, Sansanayudh W, et al. Topical treatment with 1% cyclosporine for subepithelial infiltrates secondary to adenoviral keratoconjunctivitis. Cornea. 2010 Jun;29(6):638-40.
17. Okumus S, Coskun E, Tatar M, Kavdu E, et al. Cyclosporine a 0.05% eye drops for the treatment of subepithelial infiltrates after epidemic keratoconjunctivitis. BMC Ophthalmol. 2012 Aug;12(42).
18. Romanowski E, Pless P, Yates K, Gordon Y. Topical cyclosporine A inhibits subepithelial immune infiltrates but also promotes viral shedding in experimental adenovirus models. Cornea. 2005 Jan;24(1):86-91.
19. Kolomeyer A, Nayak N, Ragam A, et al. Topical Cyclosporine A 1% for the Treatment of Chronic Follicular Conjunctivitis. Eye Contact Lens. 2014 Dec 10 [epub ahead of print.]
20. Han J, Yoon J, Jang S. Short-term effects of topical cyclosporine A 0.05% (Restasis) in long-standing prosthetic eye wearers: a pilot study. Eye. 2014 Oct;28(10):1212-17.


