Fitting multifocal contact lenses combines scientific information we have integrated into our clinical decisions, information delivered by educators, and observations we have realized through patient management. This article will address the knowledge we have obtained and integrated into our multifocal contact lens management. The concepts we will discuss will dispel some of the notions many have taken as fact. Looking closer at the mechanisms of multifocal contact lens fittings, we will offer an alternative view of how multifocal contact lenses work. These observations will help you become more successful at fitting your patients with multifocal contact lenses as well as change the way you approach this lens design.
Placing the Prescription in Front of the Pupil
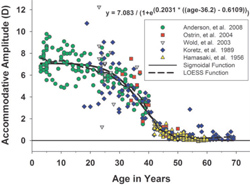
Maximum accommodative amplitudes for subjects pooled from the present study and four previous published studies.1-4
Before starting with a gas-permeable (GP) multifocal lens design, the lens power has to be considered; this will play a major role in selecting the lens design. A plus lens with the center of gravity behind the lens has difficulty centering because of its weight and tends to position inferiorly. A minus lens can easily center with the center of gravity in front of the lens. With either plus or minus power, the pupil is where the power of the lens controls the rays of light entering the eye and must fall upon the central retina. All multifocal lens designs, annular, aspheric or alternating, are controlled by the location of the pupil in regard to the optics of the lens. Generally, GP lenses can be elevated if a flatter base curve is selected. If a steeper GP base curve is selected, the lens will position more inferiorly.
Another option is to change the size of the lens. By making the lens larger, you are increasing sagittal height, simulating a steeper fitting lens and reducing the lift. Conversely, by making the lens smaller, you will simulate a flat fitted lens by reducing sagittal height and increasing the lift, which will position the lens superiorly. Gas-permeable lens movement on the cornea is created by either increasing or decreasing the lift of the lens, which is controlled by the amount of tears underneath it. The tears underneath the lens will cause the lens to float. Thus, if a patient has a reduced tear film layer, the effect of lift is minimized, and this lens will float less.
Ultra-thin disposable lenses wrap around the cornea, and lift has minimal effect on lens movement because of reduced tear flow underneath the lens modality. These ultra thin lenses do not move on the eye, and the only multifocal option is a simultaneous design. Although as you increase the thickness of a soft lens, more tears and fluid reside underneath it. The thickness of a soft lens increases the lens modulus or stiffness, and the lens takes on the traditional rules of GP contact lenses that are affected by size and base curve selection. The movement and positioning of a rigid lens is controlled by the base curve and size of the lens, but the movement and positioning of a soft lens is first controlled by the lens thickness. As the thickness of the soft lens increases, so does the influence of base curve and diameter on lens positioning and movement. By controlling the position and movement of either a rigid lens or a soft lens, we increase the rate of successful outcomes when fitting bifocal contact lenses. Understanding these simple rules will position the prescription power over the pupil and improve the resultant quality of vision in a bifocal lens.
Table 2. Expected Values of Accommodation (Diopters)7-9
Age (years)
10
15
20
25
30
35
40
45
50
55
60
65
70
Donders
14
12
10
8.5
7.0
5.5
4.5
3.5
2.5
1.75
1.00
0.5
0.125
Duane (mean)
13.4
12.6
11.5
10.2
8.0
7.3
5.9
3.7
2.0
1.3
1.1
1.1
---
Hofstetter (probable)
15.5
14
12.5
11
9.5
8
6.5
5
3.5
2
0.5
0.5
---
EyeVis Bifocal Add
__
__
__
__
__
__
0.50
1.00
1.50
2.00
2.25
2.50
2.50
Choosing the Add Prescription
The amplitude of accommodation in normal human eyes has been studied by various researchers and it was observed that the onset of presbyopia occurs at about the age of 45.5,6
A bifocal add prescription gives us the power to offset the loss of accommodation. If the value of accommodation is known and the supplemental add power is adjusted for the proper working distance, the resultant necessary add power is realized. Most patients need to have a range of clear near vision with the midpoint between 14 inches and 18 inches. When you know the remaining accommodation value and the working distance, the bifocal power can be assumed without the use of any measuring test. Donders and Duane have provided us with the data to discover the values of accommodation at a certain age (see Tables 1 and 2). Their investigation resulted in a specific diopteric power for nearpoint according to age. Their outcome analysis assumes average arm length with the other assumption being that the nearpoint demand is for 14 inches to 18 inches. The working distance of an individual with short arms will be different than someone with long arms. A simplistic approach is to quantify the bifocal age rather than dioptric power when ordering a bifocal contact lens. The push up test and other near point diagnostic measuring tools have been employed to arrive at a bifocal add. When ordering bifocal contact lenses, the observation typically utilizes a half diopteric interval, which falls within the EyeVis conversion (see “Expected Values of Accommodation” p. 29).
The Role of the Pupil
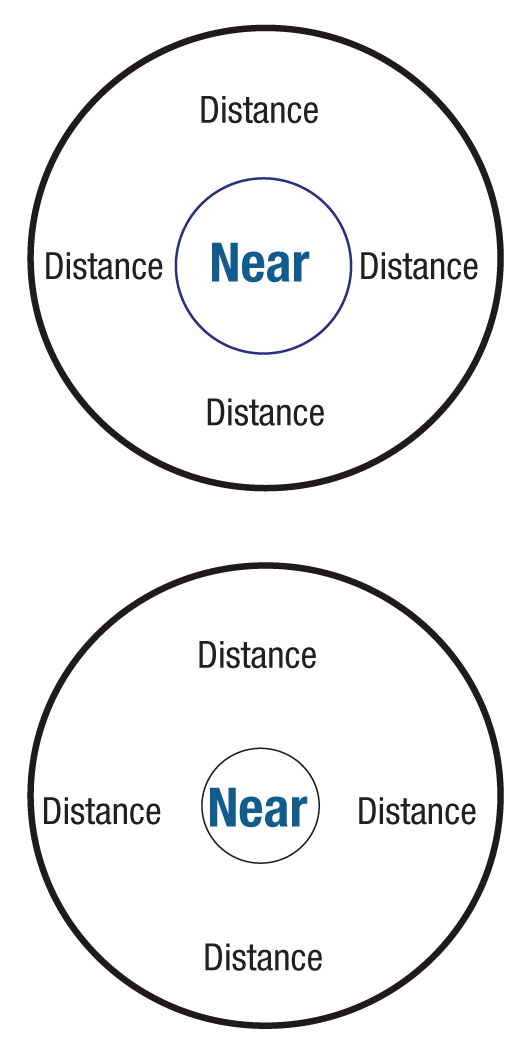
Aspheric lenses with different pupil sizes.
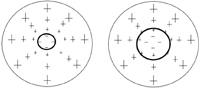
The most important parameter in constructing a multifocal contact lens is pupil size and the relationship between distance and near zone size. Pupil size controls the rays of light entering the eye. Ignoring the shape of the bifocal zones—circular with annulars and aspherics and rectangular with alternating—successful outcomes are achieved by placing the zone in a reachable position from the pupil. This is done with both soft and GP lens designs, so that the line of sight or angle of sight can achieve clear vision. The annular distance and near zone size is controlled by the size of the pupil. If the pupil is 3.5mm, you must determine how much of this area is distance, and how much is near. As an example the Proclear Multifocal “D” lens design (CooperVision) incorporates a fixed 2.3mm distance zone and the remaining area, 1.2mm, is designated for near. If a patient has a 6.0mm pupil, the distance zone size is still 2.3mm, but the near zone has 3.7mm of vision. Clearly, the visual results will be different just because of zone size, and your ability to customize the zone size will dramatically increase the rate of success.
Aspheric Lens Designs
Annular lenses with different pupil sizes.
Aspheric multifocals have a similar problem with variations in pupil size and a constant lens zone size, although the cause is slightly different. These lenses either increase in plus power moving away from the distance center or decrease in plus power moving away from the near center. Aspheric multifocal power curves are controlled by the distribution of power change within the optic zone. In order to match the proper reading power with a patient’s visual demands, we must consider the patient’s pupil size, which will define the effective add power for a given aspheric multifocal lens design. The power spread for a patient with a 6mm pupil has wider zone than for an individual with a 3.5mm pupil. In order to produce an equivalent effective add, the patient with a 3.5mm pupil would need to utilize a lens with a significantly higher rate of power shift (i.e., a higher eccentricity designed aspheric lens) when compared to a patient with a 6mm pupil. But, as the required eccentricity increases, the degree of visual distortion and need for more perfect lens centration also increases. Often, aspheric lenses have a very small effective central zone, which can create problems with vision due to power compression. Actually, true aspheric lenses do not have a central “zone” because the power varies gradually from the center of the lens. This problem can be addressed by designing a central aspheric zone of a given power and eccentricity that is surrounded by an annulus of a different power and eccentricity. This is a lens design with two aspheric curves: the center aspheric zone is for distance to intermediate, and the peripheral aspheric curve is for intermediate to near vision. This lens design will decrease distortion by reducing the compression of powers. We can design either a distance center or a near center version of this type of lens and control the zone sizes according to the patient’s pupil size. When we match the annular or aspheric lens design with pupil size, it seems more reasonable to have separate zone sizes for large pupils and small pupils.
Alternating Lens Designs
Alternating lenses have two distinct zones instead of the distance and near powers surrounding each other. Distant zone is on the top, and the reading zone on the bottom. The optimal lens position for this bifocal design is the separation between the two zones placed within the inferior pupil, yet below the line of sight in primary gaze. If the line of separation is too high, the near segment interferes with the distance vision. If the line of separation is too low, the near zone will not come into focus. It has been said that the lower lid is the defining characteristic to observe when you want to determine whether this type of lens can be fit successfully.
It must be positioned at the limbus. Our experience is that if the lower lid is below the limbus, the lens needs to have a larger diameter so that the line of separation is positioned inside the lower edge of the pupillary margin. Conversely, if the lower lid is above the limbus or the palpebral fissure is small, the lens diameter needs to be reduced so that the line of separation between the two zones is positioned inside the lower margin of the pupil. Clarity is achieved by either looking only through the distant zone or by looking through the near zone. If the bifocal lens is positioned correctly, it is the line of sight change or angle of vision that receives distance or near vision.

This image shows proper lens location for an alternating bifocal lens.
An image emits or reflects light in different directions. Although this light diverges from the object in a variety of directions, the eye only sees a very small converging cone of rays that is coming toward the pupil. If the eye is angled downward toward the near zone, it will view a different cone of rays. Regardless of the eye location, in order to view an object, you must sight along a line at that object. When you do this, light will come from that object to your eye along the line of sight. This alternation of distant and near vision can also be achieved from the translation of the lens, but excessive lens movement can cause distortion of the vision coming in and out of focus. Minimizing lens movement and positioning the lens into the inferior portion of the pupil creates the best vision for the alternating lens design. The one caveat to this lens design is that the fit of the lens may cause the near segment to ride up into the pupillary zone with the blink, and the patient will describe their vision as going in and out of focus. This is why the lens design must be configured to minimize vertical movement with the blink. Optimal vertical movement with blink will be not only limited, but will exhibit what is described as a “quick drop” following blink back to its original position in primary gaze.

Straight ahead distance (left). Change in the angle or line of sight (middle). Lens translation (right).
Custom Lens Designs
Bifocal lenses made of soft or rigid materials are best configured in custom lens designs to achieve an optimal result that is based on the patient’s pupil size and controlling the images focused on the back of the eye. Rigid lenses are easier to adjust because of the variety of parameters available to achieve the ideal lens positioning. But, the problem with rigid lenses is that they tend to move too much because of the forces acting upon the lens with the blink. As the lens moves up and down, the visual system has to grab the image and suspend it in time in a straight ahead position.
When the globe is positioned downward, movement is minimized due to the reduced lid forces and gravity. Disposable soft lenses are difficult to manipulate because lens movement is nonexistent, and adjusting the line of sight presents a challenge. The only parameter in soft lenses that can adjust line of sight is zone size. Zone size will provide a power distribution in front of the pupil to change the line of sight or angle of vision when the globe is not in straight alignment. Hybrid lenses behave like soft lenses and move very little on the eye, making line of sight or angle of vision difficult to change. Thin, soft lenses, such as disposable lenses, tend to wrap around the cornea, minimizing the effect of the fitting base curve. By increasing the thickness of a soft lens, the hydrophilic lens design moves more like a rigid lens, making the fitting base curve critical. If you combine the optics of a rigid lens and the incremental control of movement that a thicker soft lens can provide, the combination creates a successful outcome.
Custom toric lens fabricators have adjusted their fitting paradigms to incorporate this concept of thicker soft lenses. By increasing the soft contact lens thickness and placing a rigid lens inside a recessed Pillow soft lens, you gain full control of lens movement. Remember: line of sight can be altered by changing the base curve of the soft portion of this combination lens, and the optics of the combination lens are provided by any rigid bifocal lens design.
Aspherics, annulars and alternating lenses have their advantages just as their counterparts in spectacle lenses do. The nose pads of spectacles provide the stability just as the soft lens in the combination/recessed Pillow lens. Comfort with the combination/recessed Pillow lens is no longer a problem as it was with the rigid lens design, and vision is no longer a problem as was the case with the soft multifocal lens. The issue of lens movement is also resolved, as it can be incrementally changed by altering the base curve of a soft Pillow lens. Finally, the optics of the combination/recessed Pillow lens can now be controlled by the rigid portion to achieve pristine distant and near vision.
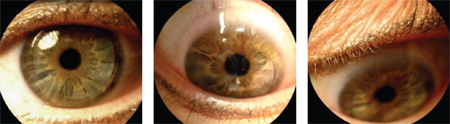
This Pillow lens has a
soft carrier and a rigid bifocal center. Straight ahead gaze (left);
downward gaze with inferior line of sight (middle and right).
Whether in contact lenses or spectacles, precise multifocal alignment is essential for a successful outcome. The same approach must be incorporated to accommodate straight ahead clear distance vision and downward gaze near vision. In spectacles, the nose stabilizes the device for proper segment positioning, and in contact lenses, we must incorporate creative lens designs to accomplish this task. Spectacle multifocal positioning is accomplished by meticulously measuring the bifocal segment position in each individual patient. If alignment problems exist with a multifocal spectacle lens, a simple frame adjustment can be made.Keep in mind that multifocal spectacle lenses are not prefabricated for rapid dispensing. If customization did not exist, the success rate for spectacle multifocals would probably be similar to multifocal contact lenses. Multifocal contact lenses require the same customization approach to significantly increase the success rate. Lens centration, pupil size and palpebral fissure width are the diagnostic measurements we must collect. By varying these specifications the success rates will dramatically increase.
Another key to success with multifocal contact lenses resides in the observations of multifocal lens movement dynamics. Positioning the separation between near and distance power curves within the pupil to successfully change the line of sight or angle of vision without inducing translation or causing distortion from the wrong power curve is the methodology that makes multifocal contact lenses work. As in most things in patient care, the solution to multifocal contact lens success is right in front of us. All we have to do is look.
Dr. Davis is co-founder of Eye-Vis Eye and Vision Research Institute. He practices in a suburb outside Chicago. He is a Diplomate in the Corneal, Contact Lens and Refractive Technologies of the American Academy of Optometry.
Dr. Eiden is president of North Suburban Vision Consultants, Ltd. He is also co-founder of EyeVis Eye and Vision Research Institute and an assistant clinical professor at the University of Illinois at Chicago Medical Center.
1. Ostrin LA, Glasser A. Accommodation measurements in a prepresbyopic and presbyopic population. J Cataract Refract Surg. 2004;30:1435–44.
2. Wold JE, Hu A, Chen S, Glasser A. Subjective and objective measurements of human accommodative amplitude. J Cataract Refract Surg. 2003;29:1878–88.
3. Koretz JF, Kaufman PL, Neider MW, Goeckner PA. Accommodation and presbyopia in the human eye-aging of the anterior segment. Vision Res. 1989;29(12):1685–92.
4. Hamasaki D, Ong J, Marg E. The amplitude of accommodation in presbyopia. Am J Optom Arch Am Acad Optom. 1956;33(1):3–14.
5. Donders F.C., 1864: Anomalies of accommodation and refraction of the eye bond., 1864
6. Duane A., 1922: Amer. Ophtlialmol 5: 865
7. Donders FC. On the anomalies of accommodation and refraction of the eye. London: The New Sydenham Society, 1864:206-11.
8. Duane A. Normal values of the accommodation at all ages. JAMA 1912;59(12):1012.
9. Hofstetter HW. A useful age-amplitude formula. The Pennsylvania Optometrist. 1947;7(1):5-8.


