 Recent progress has been made in recognizing, classifying and treating lid disease. This is due, in a large part, to the efforts of the International Workshop on Meibomian Gland Dysfunction, chaired by Kelly Nichols, O.D., M.P.H., Ph.D., professor at the Ohio State College of Optometry. The committee members have worked tirelessly to help those in clinical practice and research to better understand the mechanisms that play a significant role in this disease process.
Recent progress has been made in recognizing, classifying and treating lid disease. This is due, in a large part, to the efforts of the International Workshop on Meibomian Gland Dysfunction, chaired by Kelly Nichols, O.D., M.P.H., Ph.D., professor at the Ohio State College of Optometry. The committee members have worked tirelessly to help those in clinical practice and research to better understand the mechanisms that play a significant role in this disease process.
A Complex System
The meibomian glands are quite complex, holocrine in nature and are extremely important to successful lens wear.1,2 The secretions are neuronally regulated by the parasympathetic, sympathetic and sensory sources, and are subject to hormonal (androgen and estrogen receptors) and vascular regulations.3,4 Therefore, evaporative tear film loss is primarily due to meibomian gland dysfunction and related disease.1,3,4 With MGD, there is an androgen deficiency that results in a loss of the lipid layer—specifically triglycerides, cholesterol, mono-saturated essential fatty acids and polar lipids.1,4 The loss of polar lipids exacerbates the evaporative tear loss and the decrease in unsaturated fatty acids raises the melting point of meibum.4,8 This results in a more viscous, thicker secretion that obstructs dusts and causes significant stagnation.4
The Screening Process
Any pre-fit evaluation for potential contact lens wear must include a careful screening for lid disease. It is fundamentally important to ask the right questions during the screening process in order to pinpoint MGD.1 Addressing several major issues, including red, dry, gritty or irritated eyes and sensitivity to makeup helps to make a timely diagnosis and allows practitioners to match patients to the right treatment plan.1,2 A careful external and slit lamp examination should include gland expression, lash inspection and an overall assessment for signs of inflammation of the lids and face. Rosacea, blepharitis and demodex are common guests of the lid area and will negatively impact contact lens wear.
It’s important to note that lens wear has a direct effect on the meibomian glands and their secretions; contact lenses likely cause a decrease in the number of functional meibomian glands and this appears to be proportional to duration of lens wear.6
Constant Assault
Contact lens wearers experience a constant assault on the lids, especially the meibomian glands. Several investigators have made the association of meibomian gland alterations with allergic eye disease.7 Eric Donnenfeld, M.D., of Long Island, N.Y., and associates have shown significant histological changes to the glands, such as meibomian gland distortion with perennial allergic conjunctivitis. Although the exact mechanism is unknown, inflammatory changes likely induce pressure on the meibomian glands and cause distortion over time. Eyes with allergic conjunctivitis were found to have markedly higher meibum inspissation (higher meibomian expression scores) and superficial punctate keratopathy scores than the non-allergic control eyes.7
Classification System
A classification system that helps to differentiate and lead to appropriate treatment and management is key. The International Workshop has proposed a classification system based upon pathophysiology. The sub-committee has stratified MGD by designating a low delivery and high delivery state of secretion and obstructive conditions in meibomian gland disease.1,3,8 MGD is a chronic, diffuse abnormality of the meibomian glands that is commonly characterized by terminal duct obstruction and/or qualitative and quantitative changes in the glandular secretion.3 According to J. Daniel Nelson, M.D., professor of ophthalmology at the University of Minnesota, “Meibomian gland dysfunction is not synonymous with blepharitis or meibomitis. Meibomian gland dysfunction is often present without inflammation.”8
Workshop members have devised a four-stage classification scheme:
• Stage 1 is mild disease where there are no symptoms, but only signs of disease.
• Stage 2 encompasses patients with some symptoms that require a variety of treatments, such as ocular lubrication, supplements and topical steroids for relief.
• Stage 3 includes complications that involve the cornea and require topical steroid treatment.
• Stage 4 includes serious complications, such as lid and corneal morbidities, which require surgical intervention.5
Recognition and Treatment
Early recognition and treatment are paramount for successful outcomes. Meibomian gland disease is a progressive condition and early treatment can prevent permanent scarring and closure of meibomian gland orifices.2,3,7 Fortunately for those who treat this disease process, there are several new strategies to help manage the conditions that present. Most notably, there are many challenges to mechanical therapy—lid scrubs, massage and warm compresses.9 Topical antibiotic drops and ointments do not show good efficacy because of poor penetration and minimal anti-inflammatory effects. Oral antibiotics—especially the tetracyclines—exhibit better efficacy, but cause multiple side effects.1,7,9
The use of topical azithromycin (AzaSite, Inspire Pharmaceuticals) has become popular due to its independent anti-inflammatory effect as well as its antibacterial properties.9 It has excellent penetration and attains lasting tissue concentrations when applied directly to the lid, making it ideal for the treatment of MGD.1,9 Topical application of azithromycin plus lid hygiene has become the first line of therapy. If additional therapy is necessary, oral tetracycline, omega-3 fatty acid supplements, topical cyclosporine and steroids can be added.9 Treating accompanying allergic eye disease is essential for a good outcome in lens wearers. Other strategies to minimize any allergic effect include the use of daily disposable lenses, frequent lubrication, washing hair before bedtime and cold compresses. Additional experimental measures to treat MGD include duct probing, pulsed light therapy and hormonal supplementation.10
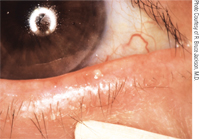
Expression of the meibomian glands and noting the quality of the secretions is a key to diagnosis.
For the most part, MGD is an under recognized, under-treated condition that, if left unchecked, can negatively impact the successful wear of contact lenses. All of us look forward to additional insights from the International Workshop on how to effectively manage this disease process.
1. Nichols K. Cracking down on meibomian gland dysfunction. Optometric Management. 2010 Oct. Available at: www.optometric.com/article.aspx?article=104841 (Accessed November 2010).
2. Foulks GN, Borchman D. Meibomian gland dysfunction: The past, present, and future. Eye Contact Lens. 2010 Sep;36(5):249-53.
3. International Workshop Previews: MGD Report. Rev Ophthalmol. 2010 Jun:17(6): 4-5.
4. Foster CS, Yuksel E, Anzaar F, Ekong A. Dry Eye Syndrome. 2010 Nov. Available at: www.emedicine.medscape.com/article/1210417-overview (Accessed November 2010).\
5. Donnenfeld E. Clinicians aim to standardize meibomian gland dysfunction therapy. Ocular Surgery News. 2010 Jun. Available at: www.osnsupersite.com/view.aspx?rid=64009 (Accessed November 2010).
6. Arita R, Itoh K, Inoue K, et al. Contact lens wear is associated with decrease of meibomian glands. Ophthalmology. 2009 Mar;116(3):379-84.
7. Donnenfeld E. Study strongly links allergic conjunctivitis, meibomian gland duct distortion. Cornea. 2010;29(8):858-60. Available at: www.osnsupersite.com/view.aspx?rid=67652 (Accessed November 2010).
8. Hardten D. Committee aims to hone meibomian gland dysfunction diagnosis, treatment. Ocular Surgery News. 2010 Jun. Available at: www.osnsupersite.com/view.aspx?rid=63946 (Accessed November 2010).
9. Donnenfeld E. New Treatment for Meibomian Gland Dysfunction. Eyecare Educators. Available at: www.eyecareeducators.com/site/new_treatment_for_meibomian_gland_dysfunction.htm (Accessed November 2010).
10. Bethke W. The experts open up on meibomian gland dysfunction. Rev Ophthalmol. 2010 Nov:17(11):47-51.


